Does Anthem Cover Mounjaro For Diabetes Type 2

The pharmacy counter hummed with a quiet anticipation, a low thrum beneath the polite coughs and rustling bags. Sunlight streamed through the large windows, illuminating dust motes dancing in the air, a silent ballet mirroring the hopes and anxieties swirling within each person waiting. Sarah clutched her prescription, the paper slightly crinkled from nervous fidgeting, hoping against hope that this new medication, Mounjaro, would be the key to finally managing her type 2 diabetes.
The big question on many minds is: Does Anthem, one of the nation's largest health insurers, cover Mounjaro for individuals diagnosed with type 2 diabetes? The answer, like many aspects of healthcare coverage, isn't a simple yes or no, but rather a nuanced exploration of policy specifics, formulary tiers, and individual plan designs.
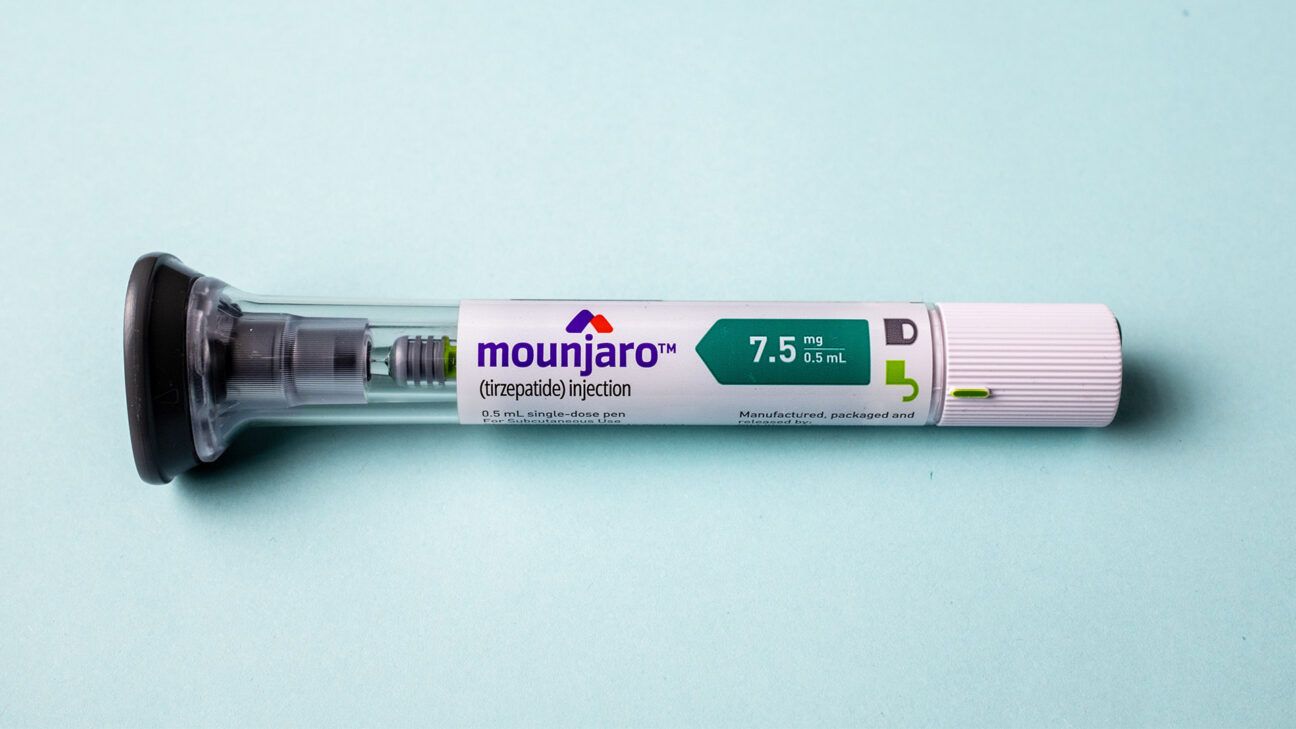
Understanding Mounjaro and its Significance
Mounjaro (tirzepatide) is a relatively new medication approved by the FDA for the treatment of type 2 diabetes. It works by mimicking the effects of two naturally occurring hormones: glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP).
This dual action helps lower blood sugar levels, improve insulin sensitivity, and, as a welcome side effect for many, promote weight loss. Mounjaro has demonstrated impressive results in clinical trials, often outperforming existing diabetes medications in terms of blood sugar control and weight reduction.
Given the increasing prevalence of type 2 diabetes and the challenges many face in managing the condition, Mounjaro represents a significant advancement. Its potential to improve glycemic control and reduce cardiovascular risk factors makes it a valuable tool for both patients and healthcare providers.
Anthem's Coverage Policies: A Deep Dive
Anthem's coverage for Mounjaro isn't uniform across all its plans. Because Anthem operates various plans (HMO, PPO, etc.) across different states and for different employers, coverage can vary substantially.
Generally, Anthem, like most insurance companies, uses a formulary – a list of covered drugs – to guide its coverage decisions. Mounjaro may or may not be included on Anthem's formulary, or it may be included on a higher tier, requiring higher co-pays or cost-sharing.
Even if Mounjaro is on the formulary, Anthem often requires prior authorization. This means a doctor must submit documentation justifying the medical necessity of the medication.
Common Prior Authorization Requirements
Prior authorization requirements often include demonstrating that the patient has already tried and failed other, more established (and often cheaper) diabetes medications, such as metformin or sulfonylureas.
Anthem may also require documentation of the patient's A1C level, a measure of average blood sugar over the past 2-3 months, to ensure that Mounjaro is appropriate for the patient's level of glycemic control. Documentation of other health factors, such as body mass index (BMI) or other existing conditions, could also be requested.
For instance, Anthem may prioritize coverage for patients with a higher BMI or those with a history of cardiovascular disease, given Mounjaro's potential benefits in these areas. Without meeting these criteria, patients may face denial of coverage, leading to potentially high out-of-pocket costs.
Navigating the Coverage Landscape
For individuals with type 2 diabetes and Anthem insurance, understanding their specific plan details is crucial. The first step is to check the plan's formulary, which is usually available online or by contacting Anthem's customer service.
If Mounjaro is listed, pay close attention to the tier it's on and any associated co-pays or cost-sharing requirements. If Mounjaro isn't on the formulary, or if the cost is prohibitive, discuss alternatives with your doctor.
Your doctor can also help navigate the prior authorization process, providing the necessary documentation to support your request for coverage. If a prior authorization is denied, there's typically an appeals process, which your doctor can assist with as well.
"It's important for patients to be proactive and advocate for their healthcare needs," says Dr. Emily Carter, an endocrinologist specializing in diabetes management. "Don't be afraid to ask questions, explore all your options, and work closely with your doctor to find the best treatment plan for you."
Another avenue to explore is manufacturer savings programs. Eli Lilly, the manufacturer of Mounjaro, sometimes offers programs to help reduce the cost of the medication for eligible patients. Eligibility requirements vary, so it's worth checking the Eli Lilly website or contacting their customer support to learn more.
The Broader Implications of Coverage Decisions
Anthem's coverage decisions, like those of other major insurers, have a significant impact on access to medications like Mounjaro. These decisions can influence treatment choices, healthcare costs, and ultimately, the health outcomes of individuals with type 2 diabetes.
When innovative medications like Mounjaro are readily accessible, patients and healthcare providers have more tools to manage diabetes effectively. This can lead to improved glycemic control, reduced complications, and a better quality of life.
Conversely, restrictive coverage policies can limit access, potentially leading to poorer health outcomes and increased healthcare costs in the long run due to complications from poorly managed diabetes. The balance between cost containment and patient access is a constant challenge in healthcare policy.
The future of Mounjaro coverage will likely depend on several factors, including ongoing clinical trial data, cost-effectiveness analyses, and negotiations between insurance companies and pharmaceutical manufacturers.
As more real-world data emerges on Mounjaro's effectiveness and safety, Anthem may adjust its coverage policies accordingly. The evolving landscape of diabetes treatment requires ongoing evaluation and adaptation to ensure that patients have access to the best possible care.
Looking Ahead: A Hopeful Perspective
While navigating insurance coverage for medications like Mounjaro can be complex and frustrating, it's important to remember that there are resources available to help. Doctors, pharmacists, and patient advocacy groups can provide guidance and support.
The development of new and innovative diabetes medications like Mounjaro offers hope for improved disease management and a better quality of life for millions. By staying informed, advocating for their needs, and working closely with their healthcare providers, individuals with type 2 diabetes can navigate the challenges and access the treatments that are right for them.
Sarah, still waiting at the pharmacy counter, took a deep breath. Regardless of the outcome of her prescription claim, she knew she wasn't alone in her journey. The shared experiences, the collective hope for better health, and the unwavering support of healthcare professionals formed a powerful network, a beacon of light in the often-complicated world of diabetes care. Even if Anthem didn’t cover Mounjaro this time, there were other avenues to explore, other options to consider, and the unwavering belief that better health was within reach.