Does Priority Health Cover Weight Loss Medication

Priority Health members seeking weight loss medication coverage face a complex reality. Coverage varies significantly depending on the specific plan and individual circumstances.
This article cuts through the confusion surrounding Priority Health's coverage of weight loss medications. We provide a concise overview of what you need to know, focusing on plan variations, requirements, and how to navigate the process effectively.
Navigating Priority Health's Weight Loss Medication Coverage
Priority Health does offer coverage for some weight loss medications, but it's not universal. Coverage is heavily dependent on the specific plan you have.
It's crucial to understand the specifics of your individual plan. Many plans require prior authorization before covering weight loss drugs.
Key Factors Influencing Coverage
Several factors influence whether Priority Health will cover weight loss medication. This includes your BMI (Body Mass Index), specific medical conditions, and plan-specific formularies.
A BMI of 30 or higher, or a BMI of 27 or higher with weight-related health conditions, is generally required. Common weight-related conditions include type 2 diabetes, high blood pressure, and high cholesterol.
Priority Health's formulary – the list of covered medications – plays a critical role. Weight loss drugs must be included in the formulary for your specific plan to be covered.
Understanding Prior Authorization
Prior authorization is a common requirement for weight loss medications. This process requires your doctor to submit a request to Priority Health, justifying the medical necessity of the medication.
The prior authorization request typically includes your medical history, BMI, and any co-existing conditions. It must demonstrate that you meet Priority Health's criteria for coverage.
Be prepared to provide comprehensive documentation to support your request. Your doctor’s office can guide you on what is needed.
Commonly Covered Medications (Potentially)
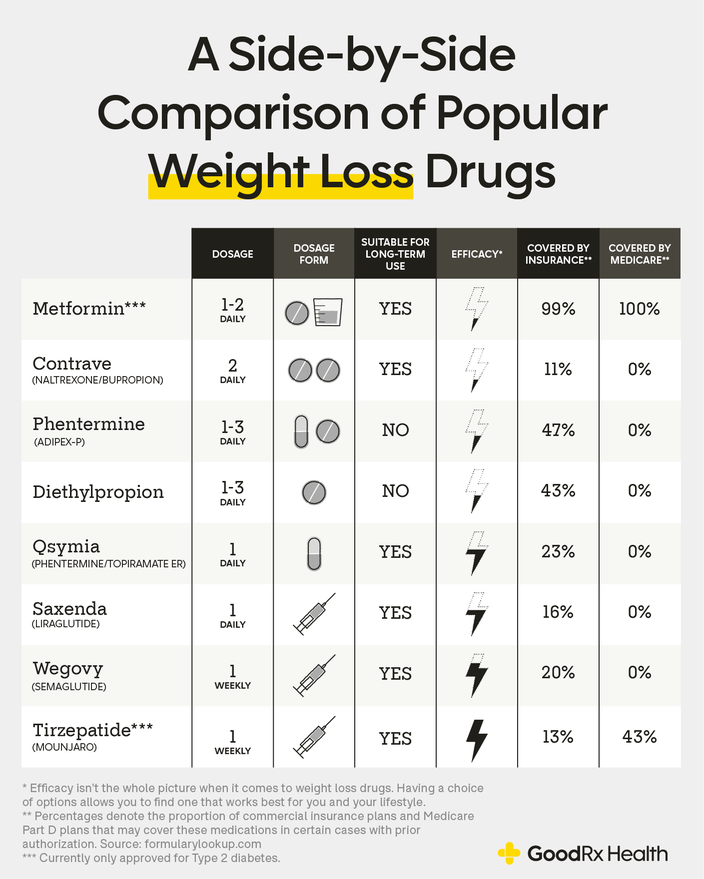
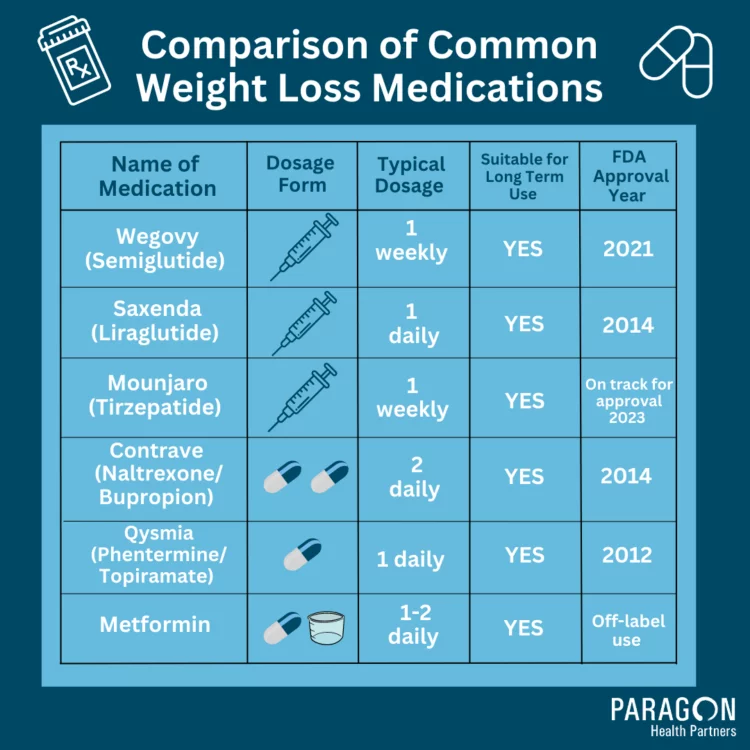
While coverage varies, certain weight loss medications are more likely to be covered by Priority Health than others. These often include medications like phentermine, orlistat, and newer GLP-1 receptor agonists.
GLP-1 receptor agonists, such as semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda), have shown significant efficacy in weight loss. However, access can be restricted.
It is important to verify if the specific medication is listed on your plan's formulary. Contact Priority Health or review your plan documents online.
Where to Find Plan-Specific Information
The most reliable source of information is your Priority Health plan documents. These documents outline the specific coverage details, including any limitations or requirements.
Priority Health's website also provides access to plan-specific information. You can log in to your account to view your formulary and coverage details.
Contacting Priority Health directly is highly recommended. Customer service representatives can answer specific questions about your coverage.
Appealing a Denial
If your prior authorization request is denied, you have the right to appeal the decision. The appeal process involves submitting additional documentation or information to support your case.
Priority Health is required to provide information about the appeal process in the denial letter. Follow the instructions carefully and meet all deadlines.
Consider seeking assistance from your doctor or a patient advocate. They can help you navigate the appeal process effectively.
The Role of Lifestyle Changes
Priority Health, like many insurers, often requires participation in a weight management program. This emphasizes lifestyle changes, such as diet and exercise, alongside medication.
These programs may be offered directly by Priority Health or through affiliated providers. Completion of such a program can be a prerequisite for medication coverage.
Document your efforts to make lifestyle changes. This can strengthen your case for medication coverage.
Next Steps and Ongoing Developments
Review your Priority Health plan documents thoroughly. Contact Priority Health directly to confirm your coverage for specific weight loss medications.
Work closely with your doctor to determine the most appropriate treatment plan. This may involve a combination of medication and lifestyle changes.
Coverage policies can change, so stay informed. Regularly check Priority Health's website or contact them for updates on their weight loss medication coverage.









:max_bytes(150000):strip_icc()/VWH-MiraNorian-WeightLossDrugUpdate-4000x2700-c813fa5051604eec9c136047fb44d23a.png)