Dopamine Low Dose Vs High Dose
Imagine a bustling hospital ward, the rhythmic beeping of monitors a constant soundtrack to the quiet drama unfolding. Doctors and nurses move with practiced efficiency, their faces etched with concentration as they respond to the ebb and flow of life. Among the arsenal of medications they wield, one stands out for its complex and often misunderstood nature: dopamine.
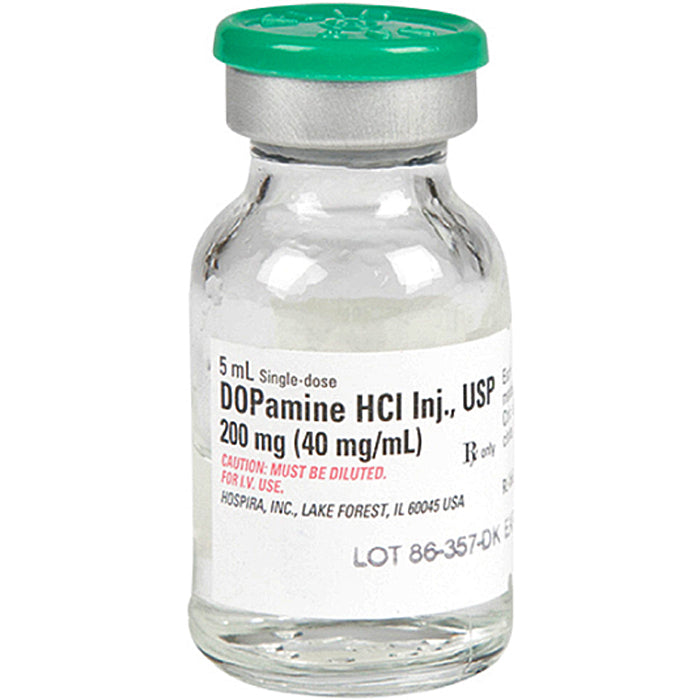
This neurotransmitter, often associated with pleasure and reward, takes on a different role in the critical care setting. Administered intravenously, dopamine can be a powerful tool for managing blood pressure and improving circulation in critically ill patients. However, the effects of dopamine are heavily dose-dependent, with low and high doses producing distinctly different physiological responses. Understanding these nuances is crucial for effective and safe patient care.
The Dual Nature of Dopamine
Dopamine, in its simplest form, is a naturally occurring chemical in the brain. It acts as a messenger, transmitting signals between nerve cells. These signals are fundamental to a wide range of functions, including movement, motivation, pleasure, and attention.
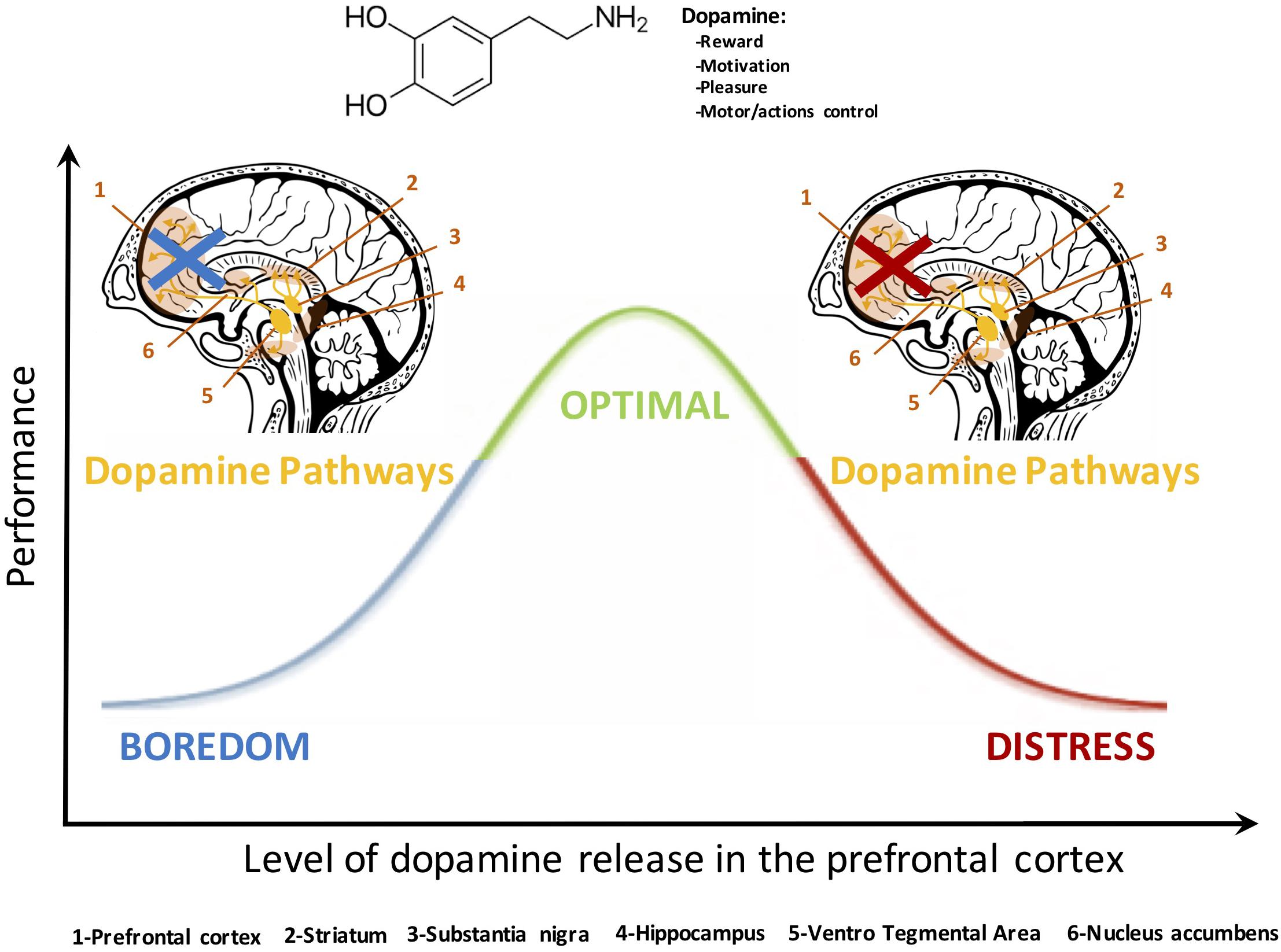
Beyond the brain, dopamine also plays a significant role in the cardiovascular system. It exerts its effects by binding to specific receptors located throughout the body, including the heart and blood vessels. These receptors, known as dopaminergic, adrenergic, and serotonergic receptors, mediate different physiological effects depending on the dose of dopamine administered.
The use of dopamine as a medication dates back several decades. Doctors initially discovered its potential to increase blood pressure in patients suffering from shock or severe hypotension. Over time, research has revealed the intricate relationship between dopamine dosage and its resulting effects on the body.
Low-Dose Dopamine: A Renal Protective Myth?
Historically, low doses of dopamine (typically 0.5-2 mcg/kg/min) were believed to selectively stimulate dopaminergic receptors in the kidneys. This stimulation was thought to increase renal blood flow, leading to increased urine output and improved kidney function.
This concept, often referred to as "renal-dose dopamine," gained widespread acceptance in clinical practice. It was commonly used in attempts to protect the kidneys in patients at risk of or experiencing acute kidney injury (AKI).
However, subsequent research, including large, randomized controlled trials, has challenged the efficacy of low-dose dopamine for renal protection. A 2000 study published in the Journal of the American Medical Association (JAMA) found no evidence that low-dose dopamine improved renal outcomes or reduced the need for dialysis in critically ill patients. Many sources now suggest this is an outdated treatment.
The current consensus, based on substantial evidence, is that low-dose dopamine does not provide any significant benefit for kidney protection and may even be harmful in some cases. Consequently, its use for this purpose has largely been abandoned in modern clinical practice.
High-Dose Dopamine: A Pressor Agent
At higher doses (typically 5-20 mcg/kg/min), dopamine primarily stimulates adrenergic receptors, specifically alpha-1 and beta-1 receptors. This stimulation leads to a cascade of effects on the cardiovascular system.
Stimulation of beta-1 receptors in the heart increases heart rate and contractility. This leads to a greater cardiac output and improved blood flow to the organs.
Simultaneously, stimulation of alpha-1 receptors in blood vessels causes vasoconstriction, narrowing the blood vessels. This increases systemic vascular resistance and, consequently, blood pressure. It is still an older method of treatment, with other methods like norepinephrine being preferred in most cases.
High-dose dopamine is primarily used as a vasopressor, a medication that increases blood pressure, in patients with severe hypotension, particularly in cases of cardiogenic or septic shock. It helps to maintain adequate blood pressure to perfuse vital organs and prevent further deterioration.
In these situations, dopamine's ability to increase both cardiac output and vascular resistance makes it a valuable tool in restoring hemodynamic stability. However, it's important to be aware of the potential side effects associated with high-dose dopamine.
Potential Side Effects and Considerations
While dopamine can be life-saving in certain situations, it's not without its risks. Side effects can vary depending on the dose and the individual patient.
Common side effects of high-dose dopamine include tachycardia (rapid heart rate), arrhythmias (irregular heartbeats), and myocardial ischemia (reduced blood flow to the heart muscle). Vasoconstriction can also reduce blood flow to the extremities, potentially leading to tissue damage.
Another important consideration is that dopamine's effects can be influenced by the patient's underlying medical conditions and other medications they are taking. For example, patients with pre-existing heart conditions may be more susceptible to arrhythmias.
Furthermore, prolonged use of dopamine can lead to tachyphylaxis, a phenomenon where the body becomes less responsive to the drug over time. This may necessitate increasing the dose to achieve the desired effect, further increasing the risk of side effects. For these reasons, most practitioners prefer other medications like norepinephrine.
Due to these potential risks, dopamine should only be administered under close medical supervision, with careful monitoring of the patient's vital signs and cardiac rhythm. Clinicians must weigh the potential benefits of dopamine against the risks before initiating treatment.
The Future of Dopamine in Critical Care
The understanding of dopamine's role in critical care continues to evolve. As research advances, we gain a more nuanced perspective on its benefits and limitations.
While the use of low-dose dopamine for renal protection has largely fallen out of favor, high-dose dopamine remains a valuable tool in managing severe hypotension. However, the trend in critical care is to use dopamine as a second-line agent, using norepinephrine as the primary agent.
Ongoing research is focusing on identifying specific patient populations who may benefit most from dopamine and developing strategies to minimize its potential side effects. This includes exploring alternative vasopressors and inotropes that may offer a more favorable risk-benefit profile.
The development of more selective dopamine receptor agonists is another area of interest. These drugs could potentially target specific dopaminergic pathways without causing the widespread cardiovascular effects associated with traditional dopamine administration.
Conclusion
Dopamine, a seemingly simple neurotransmitter, reveals its complexity within the context of critical care. The understanding of its dual nature, dose-dependent effects, and potential risks is paramount for making informed clinical decisions.
While the "renal-dose dopamine" era has passed, high-dose dopamine continues to play a role in managing severe hypotension, particularly in situations where other vasopressors are ineffective or contraindicated.
As medical knowledge advances, the future of dopamine in critical care likely involves a more targeted and personalized approach, focusing on identifying the right patients and minimizing potential harm. The constant pursuit of knowledge and refinement of clinical practice will ultimately lead to improved outcomes for critically ill patients.