Heart Valve Replacement Open Heart Surgery Death Rate

The rhythmic thump of a healthy heart is something most take for granted, yet for millions worldwide, that rhythm is disrupted by faulty heart valves. When valves fail to open and close properly, the consequences can be dire, often necessitating heart valve replacement surgery. But even with advancements in medical technology, a shadow of concern lingers: the risk of death associated with this life-saving procedure.
This article delves into the mortality rates associated with open-heart surgery for heart valve replacement, examining the factors that influence these rates and the ongoing efforts to improve patient outcomes. We will explore data from reputable organizations, analyze risk factors, discuss surgical advancements, and consider the future of heart valve replacement procedures, all with the aim of providing a comprehensive understanding of this critical area of cardiovascular medicine.
Understanding the Landscape of Heart Valve Replacement
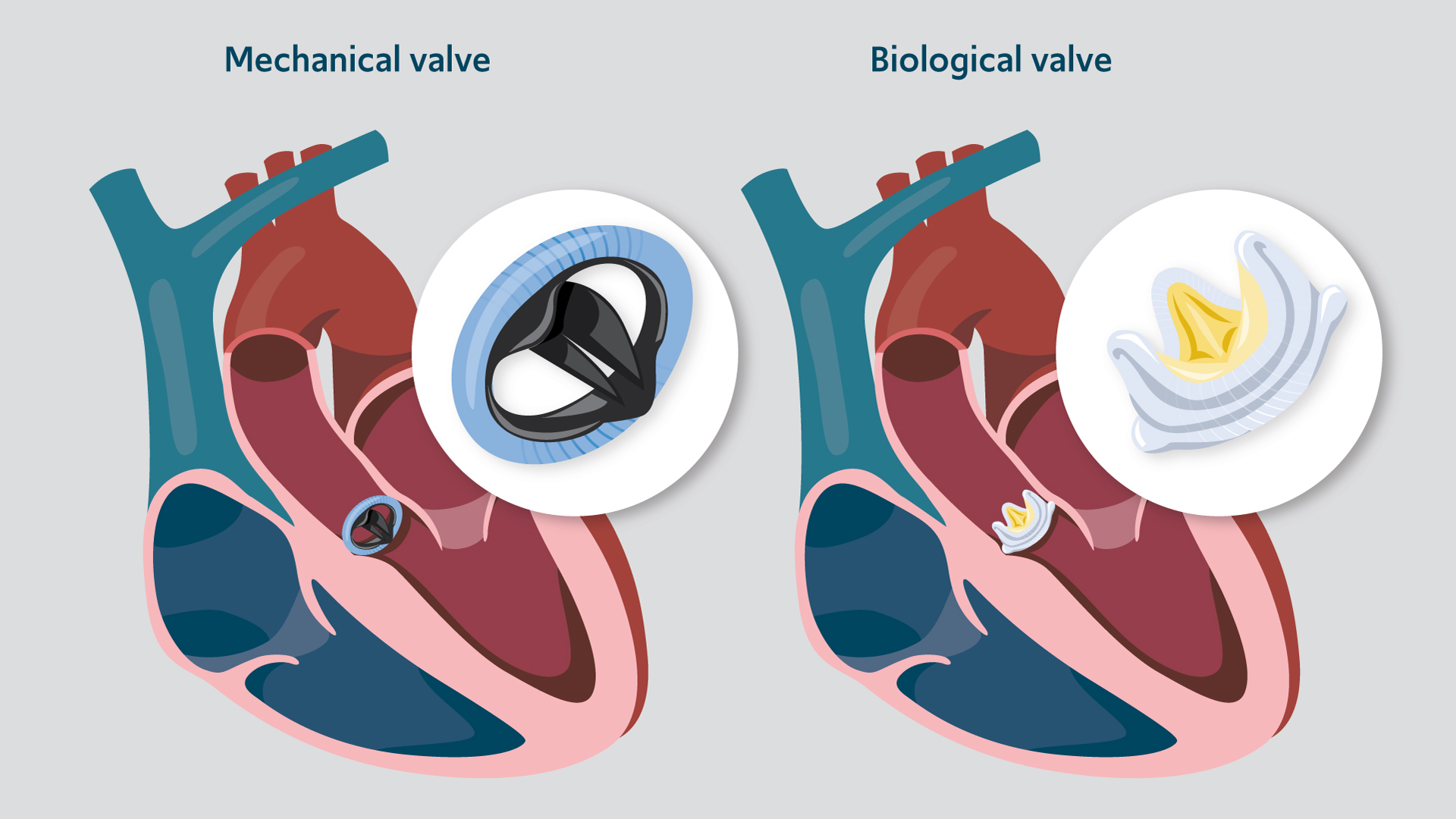
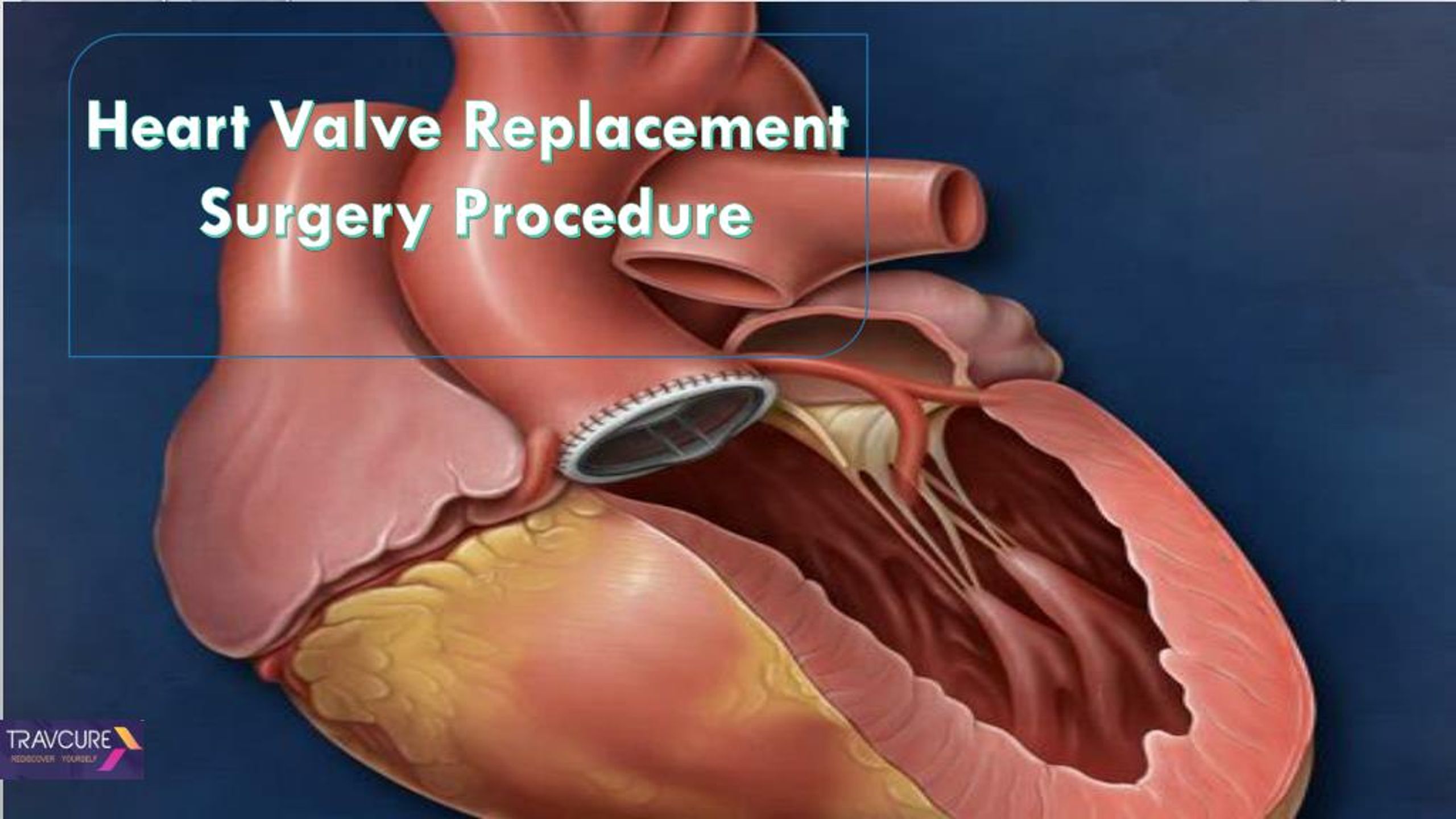
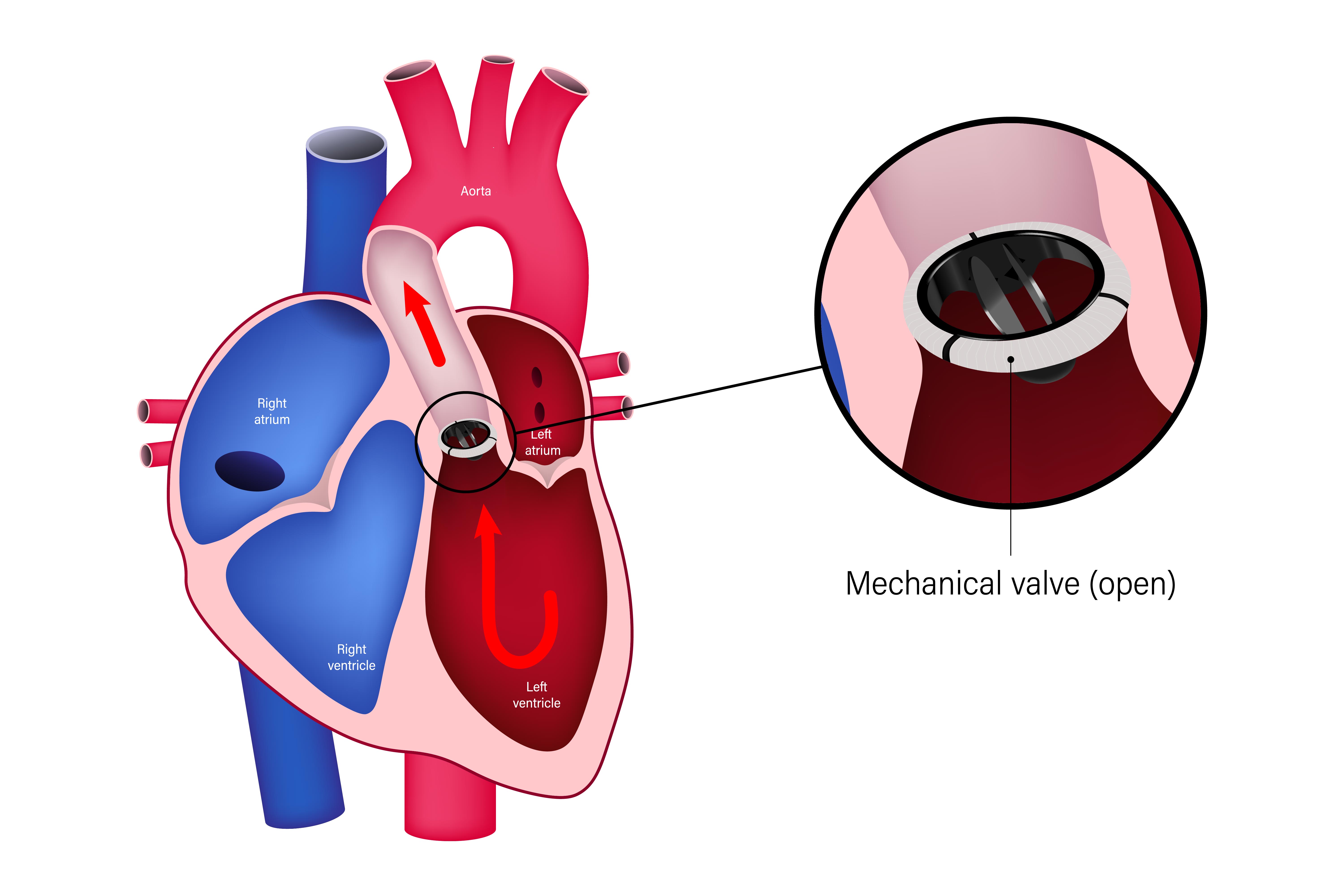
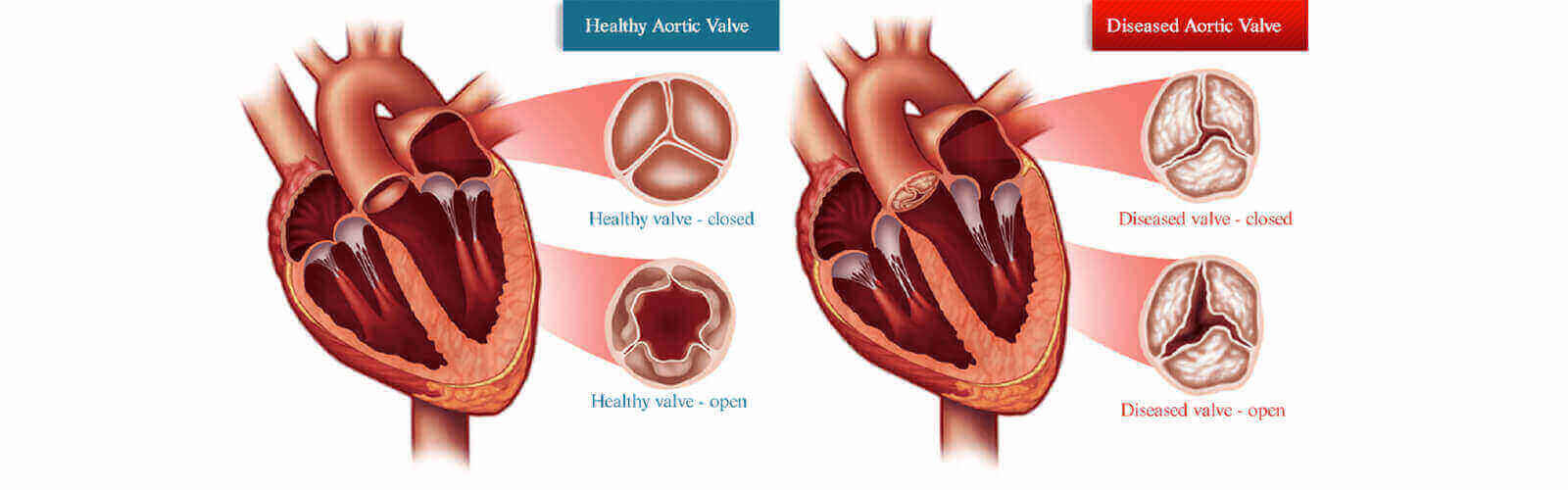
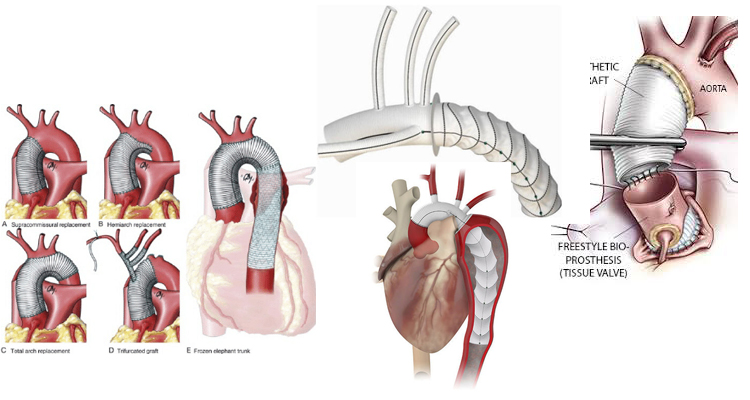
Heart valve replacement surgery, typically performed as open-heart surgery, becomes necessary when a valve becomes severely stenotic (narrowed) or regurgitant (leaky). These conditions force the heart to work harder, eventually leading to heart failure if left untreated. Replacement valves can be either mechanical, offering durability but requiring lifelong anticoagulation medication, or bioprosthetic, made from animal tissue and generally not requiring long-term anticoagulation but with a limited lifespan.
The decision to undergo surgery is never taken lightly. It involves a careful assessment of the patient's overall health, the severity of their valve disease, and potential risks and benefits of the procedure. Modern advancements have introduced less invasive techniques, but open-heart surgery remains the gold standard in many cases.
Mortality Rates: A Statistical Overview
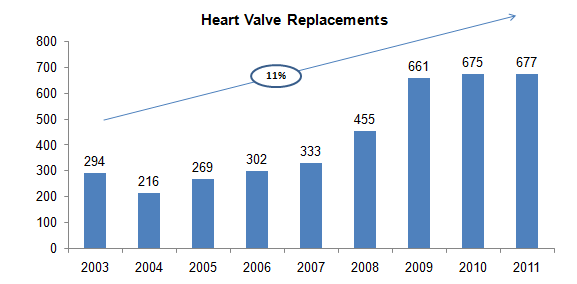
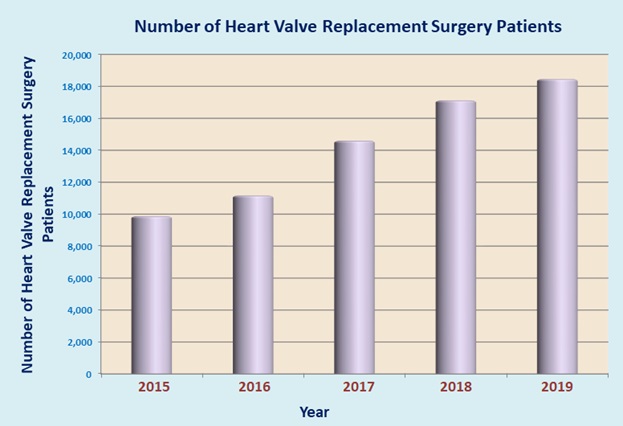
Mortality rates for heart valve replacement vary considerably depending on several factors, including patient age, overall health, and the specific type of valve being replaced. Data from the Society of Thoracic Surgeons (STS) National Database is often cited as a benchmark for surgical outcomes in the United States. According to recent STS reports, the overall in-hospital mortality rate for isolated heart valve replacement ranges from approximately 2% to 8%.
These numbers, while seemingly small, represent real lives and families. The specific rate for each patient depends on the surgical risk, which can be calculated using the STS risk calculator before undergoing the surgery.
It's crucial to note that these are averages, and individual patient risk can be significantly higher or lower. Furthermore, reporting methodologies and data collection practices can vary across different countries and institutions, making direct comparisons challenging.
Factors Influencing Mortality Rates
Several key factors contribute to the mortality rates associated with heart valve replacement surgery. Age is a significant predictor, with older patients generally facing a higher risk due to underlying health conditions and decreased physiological reserve. Pre-existing conditions such as chronic kidney disease, diabetes, and coronary artery disease also increase the likelihood of complications and mortality.
The urgency of the procedure also plays a role. Emergency surgeries, performed when a patient's condition is rapidly deteriorating, tend to have higher mortality rates compared to elective procedures. Type of valve – mechanical versus bioprosthetic – does not seem to affect the mortality rates significantly.
Surgical technique and the experience of the surgical team are also critical. Centers with higher volumes of heart valve replacement surgeries tend to have better outcomes, suggesting a learning curve and enhanced proficiency among the surgeons and support staff.
Advancements in Surgical Techniques
While open-heart surgery remains a common approach, less invasive techniques are gaining traction. Transcatheter aortic valve replacement (TAVR), initially developed for patients deemed too high-risk for traditional surgery, has now expanded to include lower-risk patients. TAVR involves inserting a new valve through a catheter, typically guided through an artery in the leg, eliminating the need for a large incision in the chest.
Minimally invasive valve surgery, performed through smaller incisions, is another alternative. These techniques can reduce pain, shorten hospital stays, and potentially lower the risk of complications. Not all patients are candidates for less invasive procedures, and the suitability depends on factors such as valve anatomy and overall health.
Robotic-assisted valve surgery, while not widely available, offers enhanced precision and dexterity, potentially leading to improved outcomes. These technological advancements are continuously evolving, offering hope for safer and more effective heart valve replacement procedures.
The Importance of Post-Operative Care
Successful heart valve replacement extends beyond the operating room. Post-operative care is crucial for ensuring a smooth recovery and minimizing the risk of complications. This includes careful monitoring of vital signs, pain management, wound care, and rehabilitation.
Patients receiving mechanical valves require lifelong anticoagulation therapy to prevent blood clots. Adherence to medication regimens and regular monitoring of blood clotting levels are essential to minimize the risk of stroke and bleeding. Comprehensive cardiac rehabilitation programs help patients regain strength and improve their cardiovascular health.
Patient education plays a vital role in post-operative success. Understanding potential complications, knowing when to seek medical attention, and adopting healthy lifestyle habits contribute to long-term well-being.
Moving Forward: The Future of Heart Valve Replacement
Ongoing research is focused on developing even more advanced and less invasive heart valve replacement techniques. Scientists are exploring new biomaterials for bioprosthetic valves with increased durability and reduced risk of rejection. Further refinements in TAVR technology aim to expand its applicability to a wider range of patients.
Personalized medicine, tailoring treatment approaches to individual patient characteristics, holds promise for optimizing outcomes. Genetic markers and advanced imaging techniques may help predict the risk of complications and guide treatment decisions. Artificial intelligence (AI) is also starting to play a role, helping to analyze large datasets to identify risk factors and improve surgical planning.
The journey of heart valve replacement is a testament to the advancements in cardiovascular medicine. While risks remain, ongoing research, technological innovations, and a commitment to patient-centered care offer hope for a future where faulty heart valves can be replaced with greater safety and efficacy, ultimately extending and improving the lives of countless individuals.