High Level Disinfectant Mostly In Dialysis Endoscopy And Laboratories

The use of high-level disinfectants (HLDs) is a critical component of infection control in healthcare settings. These powerful chemicals are essential for reprocessing medical devices that come into contact with mucous membranes or non-intact skin, playing a vital role in preventing the transmission of dangerous pathogens. A recent report highlights the crucial, yet often unseen, reliance on HLDs in specialized areas such as dialysis centers, endoscopy units, and clinical laboratories.
At the heart of this story is the ongoing effort to ensure patient safety and prevent healthcare-associated infections (HAIs). This article will explore the vital function of HLDs, focusing on where and how they are used. It will also look at some of the challenges and considerations associated with their application.
The Crucial Role of HLDs
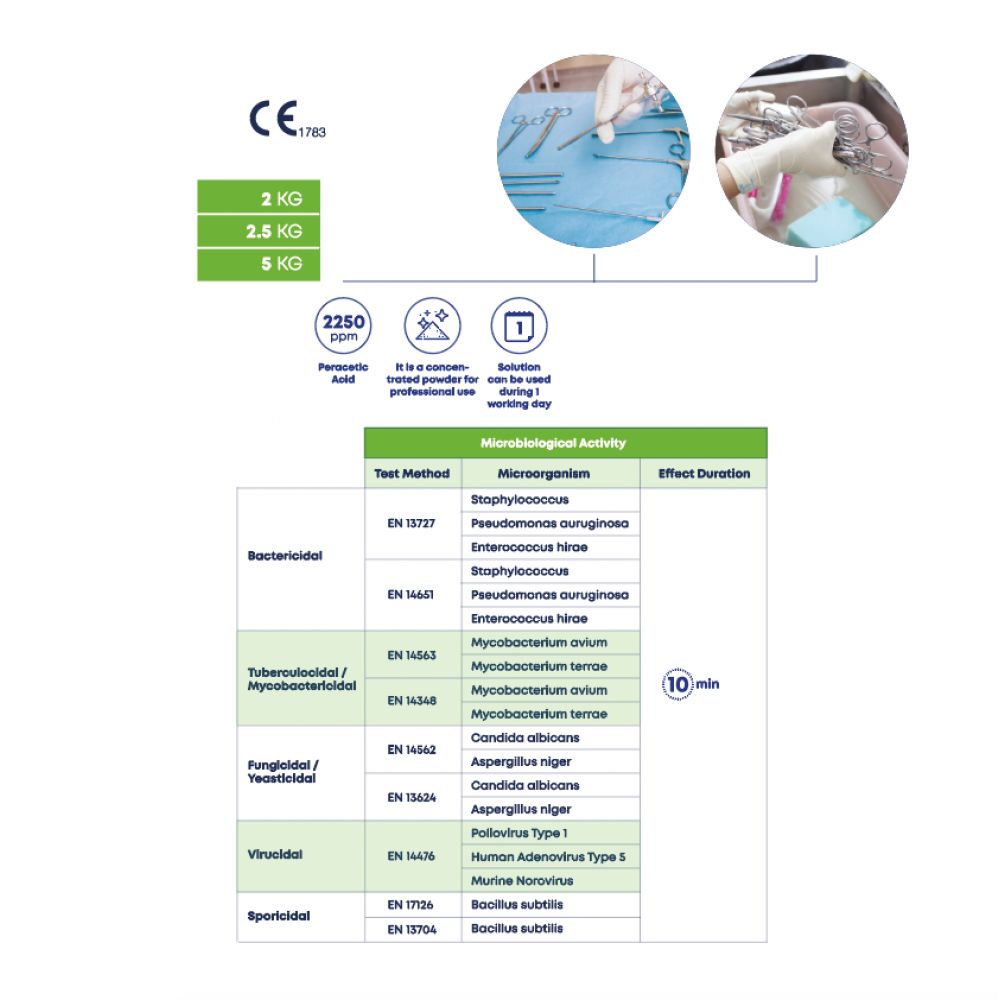
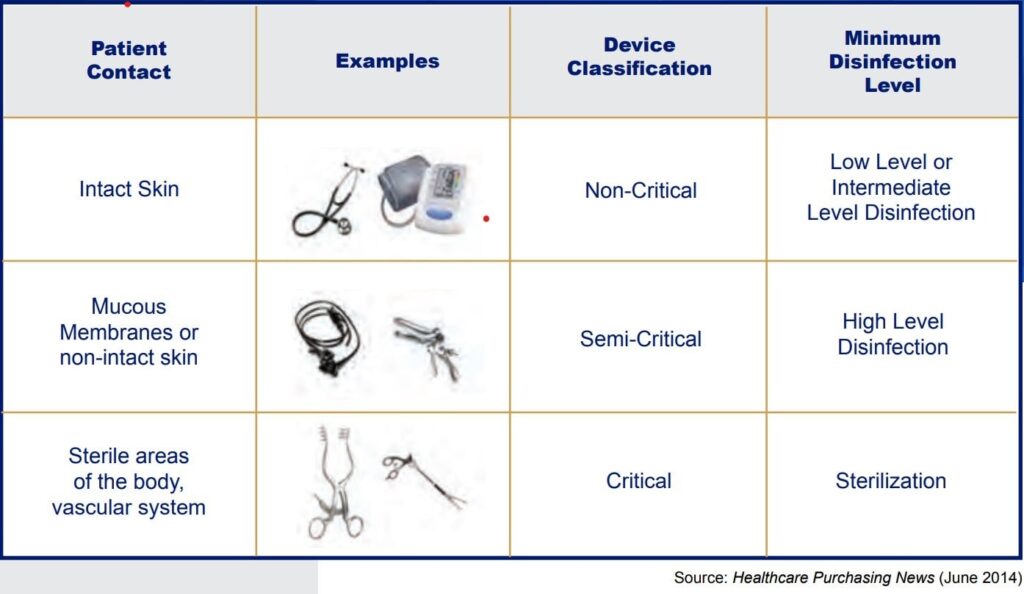
HLDs are chemical disinfectants that can kill all microorganisms, including bacteria, viruses, and fungi. But this excludes high numbers of bacterial spores. They are primarily utilized for semi-critical medical devices. These are items that come into contact with mucous membranes or non-intact skin.
In contrast, critical devices, which enter sterile tissue or the vascular system, must be sterilized. This typically involves autoclaving or other methods designed to eliminate all microorganisms and spores.
HLDs in Dialysis Centers
Dialysis centers are heavily reliant on HLDs to ensure the safety of patients undergoing hemodialysis. Hemodialysis involves connecting a patient's blood to a machine that filters waste products and excess fluids. The dialyzers and bloodlines are the devices used for this treatment.
Because these components come into direct contact with the patient's blood, rigorous disinfection protocols are necessary to prevent bloodborne infections. HLDs such as peracetic acid and glutaraldehyde are commonly used to disinfect dialyzers and other equipment between patient uses.
According to the Centers for Disease Control and Prevention (CDC), proper disinfection practices are paramount in dialysis centers to prevent outbreaks of infections like hepatitis B and C. Failure to adhere to these protocols can lead to serious health consequences for vulnerable patients.
Endoscopy and HLDs: A Vital Connection
Endoscopy involves the insertion of a flexible tube with a camera into the body to visualize internal organs. This procedure is commonly used for diagnostic and therapeutic purposes. This includes colonoscopies, upper endoscopies, and bronchoscopies.
Endoscopes, being semi-critical devices, require HLDs to eliminate microorganisms that could be transmitted between patients. Automated endoscope reprocessors (AERs) are often used. These machines expose endoscopes to HLDs like ortho-phthalaldehyde (OPA) or peracetic acid. This ensures thorough disinfection.
The Food and Drug Administration (FDA) has issued numerous guidelines and warnings regarding the proper reprocessing of endoscopes. It stresses the importance of meticulously following manufacturer's instructions. Any lapses in the cleaning and disinfection process can lead to outbreaks of antibiotic-resistant bacteria. This includes Pseudomonas aeruginosa and E. coli.
Laboratories: HLDs as a Foundation of Safety
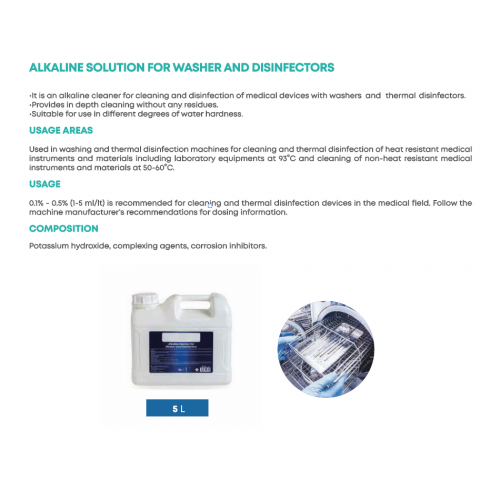
Clinical laboratories utilize HLDs to disinfect equipment and surfaces that may be contaminated with infectious agents. This is to protect laboratory personnel and prevent the spread of pathogens. Laboratory equipment that comes into contact with patient samples. This includes blood, urine, or other bodily fluids, needs regular disinfection.
HLDs such as bleach (sodium hypochlorite) are used to disinfect surfaces and equipment. This includes countertops, centrifuges, and pipettes. They provide a safe working environment.
Laboratories must adhere to strict biosafety protocols. These are outlined by organizations like the World Health Organization (WHO). This includes the proper use of HLDs to mitigate the risk of laboratory-acquired infections.
Challenges and Considerations
Despite their effectiveness, HLDs pose several challenges. One concern is the potential for chemical exposure. Workers who handle HLDs must be properly trained in safe handling procedures. They also need to be provided with appropriate personal protective equipment (PPE), such as gloves, masks, and eye protection.
Another challenge is the development of microbial resistance to certain disinfectants. Overuse or misuse of HLDs can contribute to the selection of resistant strains of bacteria. This makes infections harder to treat. Healthcare facilities must implement strategies to minimize the development of resistance. This includes rotating disinfectants and using them judiciously.
The cost of HLDs can also be a factor, particularly for smaller healthcare facilities. Some HLDs are more expensive than others, and facilities must balance cost considerations with the need for effective disinfection.
The Future of High-Level Disinfection
The field of high-level disinfection is constantly evolving. Researchers are continuously working to develop new and improved disinfectants. These disinfectants have better efficacy, lower toxicity, and reduced environmental impact. Technologies like ultraviolet (UV) light disinfection and hydrogen peroxide vapor sterilization are also gaining popularity. They offer alternative methods for disinfecting medical devices and surfaces.
Ultimately, the use of HLDs remains a cornerstone of infection prevention in dialysis centers, endoscopy units, and clinical laboratories. Proper implementation of disinfection protocols and adherence to best practices are essential. This will safeguard patient safety and prevent the spread of infectious diseases. Continuous monitoring and evaluation of disinfection practices are also necessary to ensure their effectiveness and address any emerging challenges.