High-risk Populations Include Which Of The Following
The stark reality of health disparities continues to cast a long shadow, particularly when considering the impact of infectious diseases and chronic conditions. Vulnerable populations, often bearing the brunt of these health crises, face unique challenges that exacerbate their risk and complicate efforts to achieve equitable healthcare outcomes. Identifying and understanding these high-risk groups is crucial for effective public health interventions and resource allocation.
This article delves into the question: High-risk populations include which of the following? It will explore a wide range of factors, from age and underlying health conditions to socioeconomic status and geographical location, that contribute to increased vulnerability. By examining data from reputable organizations and official statements, we aim to provide a comprehensive overview of the individuals and communities most in need of targeted support and protection. Ultimately, this understanding is a critical step toward building a more resilient and equitable healthcare system for all.
Defining High-Risk: A Multifaceted Approach
Defining "high-risk" isn't a simple task; it requires a nuanced understanding of various interconnected factors. The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) provide guidelines. They highlight specific groups that are more susceptible to severe illness or adverse outcomes from various health threats.
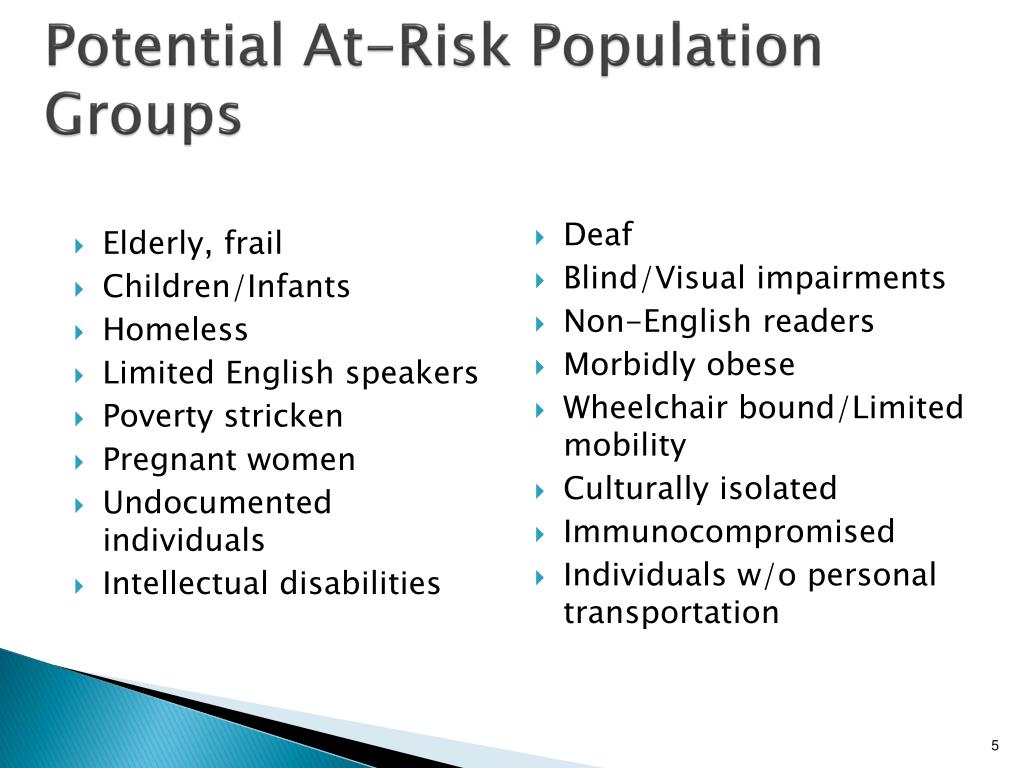
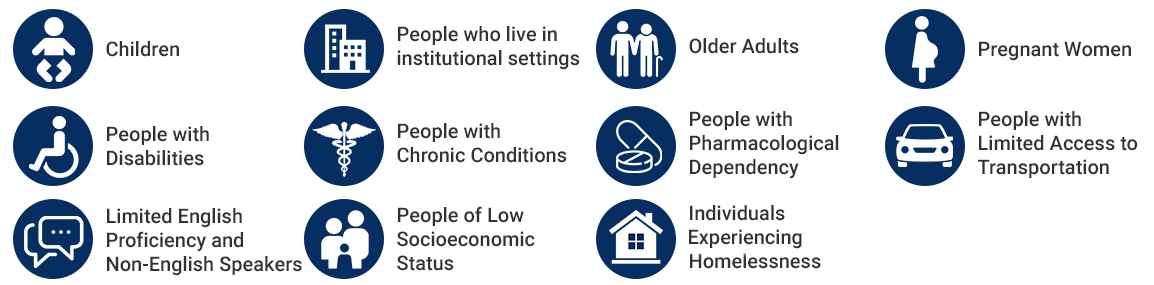
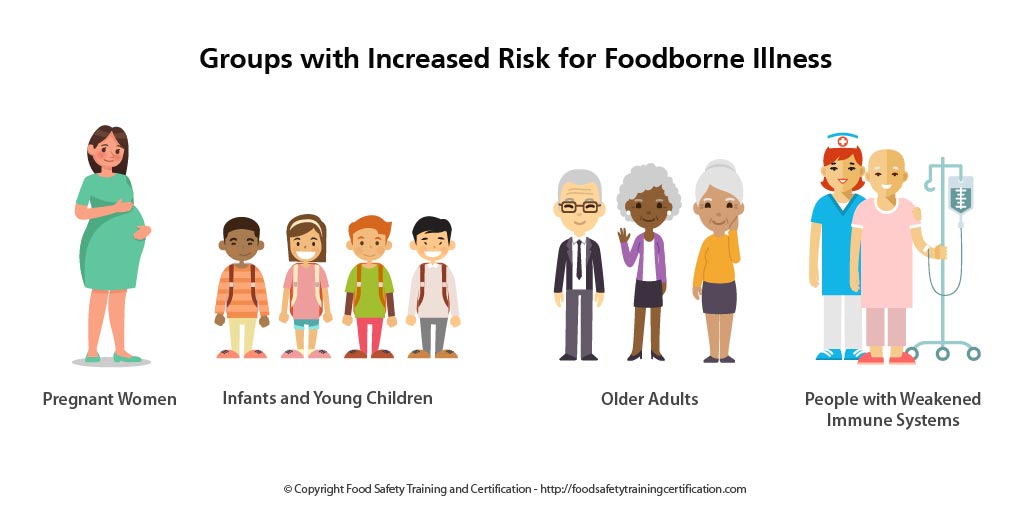
Age is a significant determinant. Older adults, particularly those over the age of 65, often have weakened immune systems and are more likely to have pre-existing conditions, making them more vulnerable to complications from infections like influenza and COVID-19. Children, especially infants and young children, also represent a high-risk group due to their developing immune systems.
Underlying Health Conditions
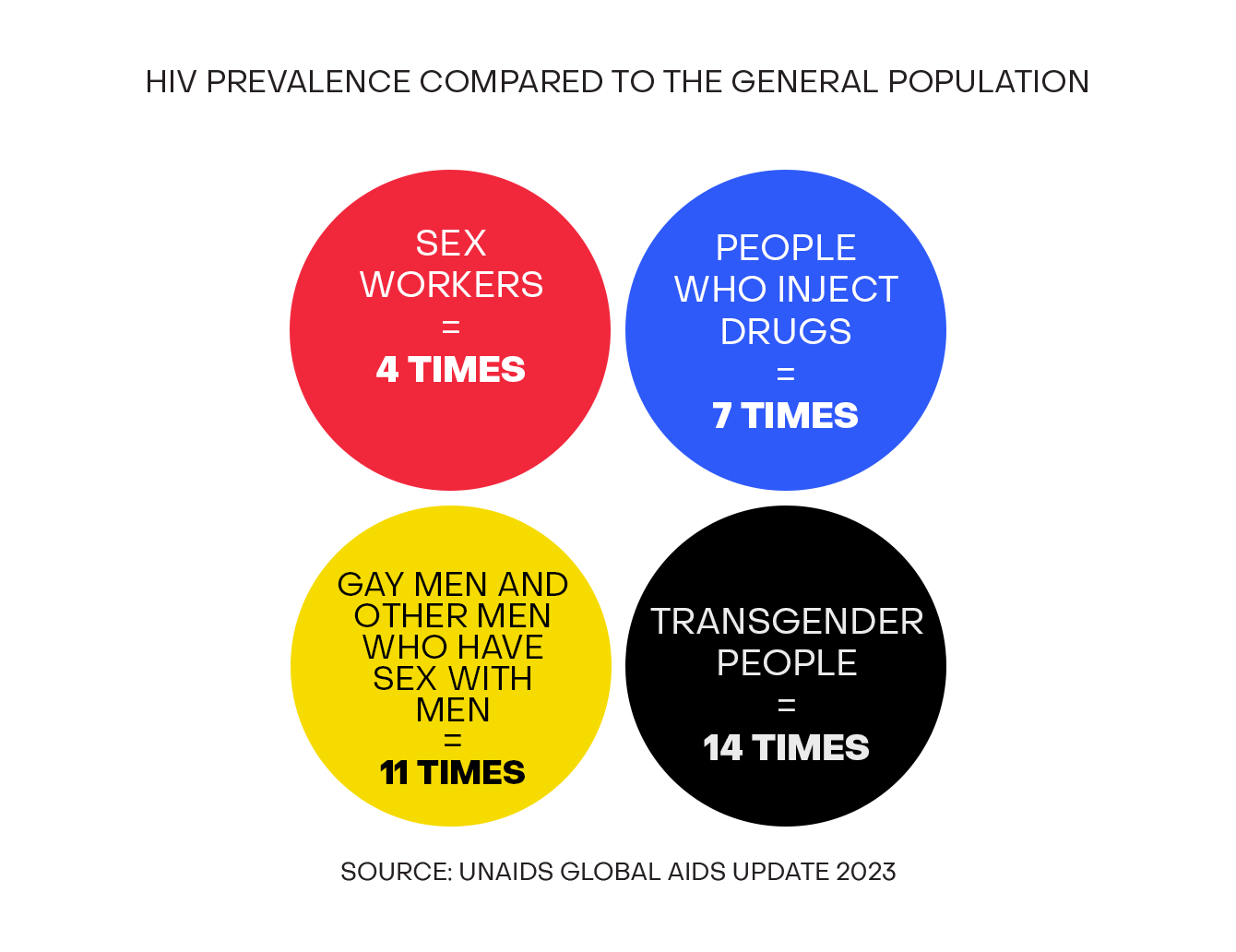
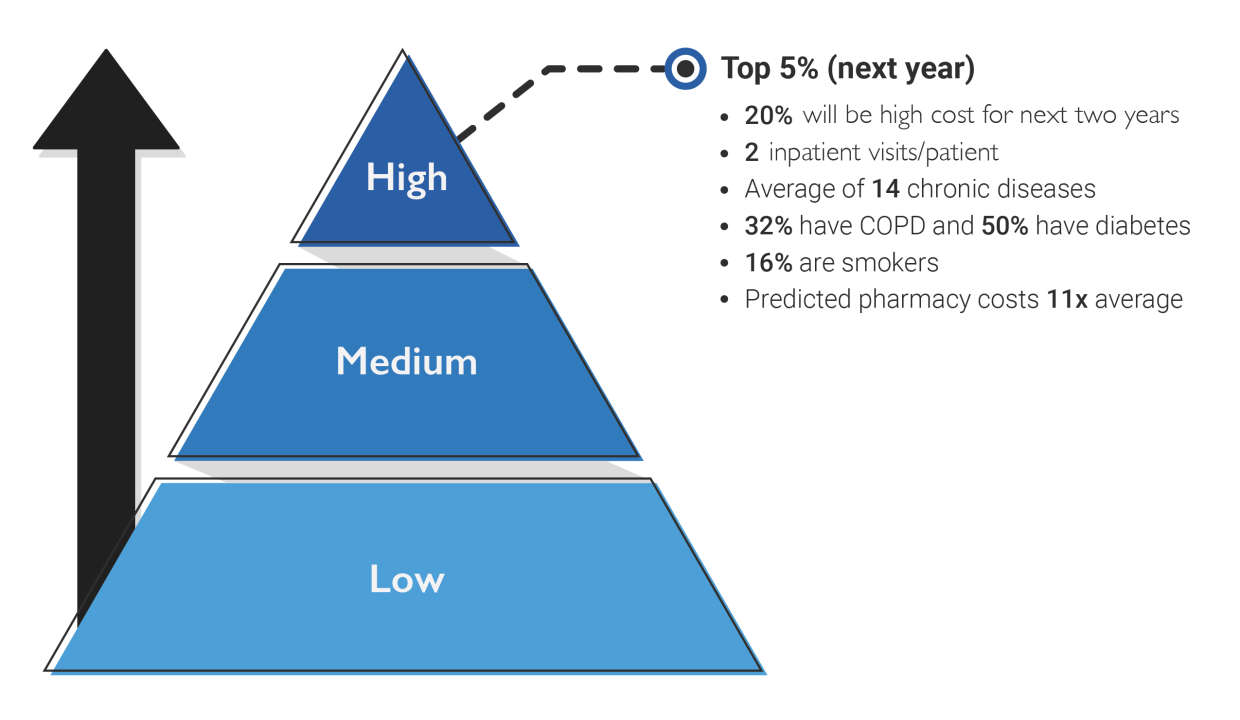
Pre-existing medical conditions significantly elevate an individual's risk. Individuals with chronic diseases such as diabetes, heart disease, lung disease, and kidney disease are more likely to experience severe symptoms and complications from infections. A compromised immune system, whether due to conditions like HIV/AIDS or immunosuppressant medications, also places individuals at increased risk.
Obesity is increasingly recognized as a major risk factor. It contributes to a pro-inflammatory state within the body, impairing immune function and increasing susceptibility to severe illness. Furthermore, pregnant women are considered a high-risk population due to physiological changes that can weaken their immune system and increase their risk of complications during pregnancy and childbirth.
Socioeconomic Disparities
Beyond biological factors, socioeconomic disparities play a crucial role in determining health risks. Individuals living in poverty often face barriers to accessing quality healthcare, including limited access to health insurance, transportation, and healthy food options. These barriers can lead to delayed diagnoses, inadequate treatment, and poorer health outcomes.
Housing insecurity and homelessness are also significant risk factors. Overcrowded living conditions increase the risk of infectious disease transmission. Lack of access to sanitation and hygiene facilities further exacerbates the problem. The WHO emphasizes the need to address these social determinants of health to improve health equity.
Racial and ethnic minorities often experience disproportionately higher rates of chronic diseases and face systemic barriers to healthcare. These disparities are rooted in historical and ongoing discrimination, resulting in unequal access to resources and opportunities. Addressing these inequities requires a multi-pronged approach that tackles systemic racism and promotes culturally competent healthcare.
Geographical Factors
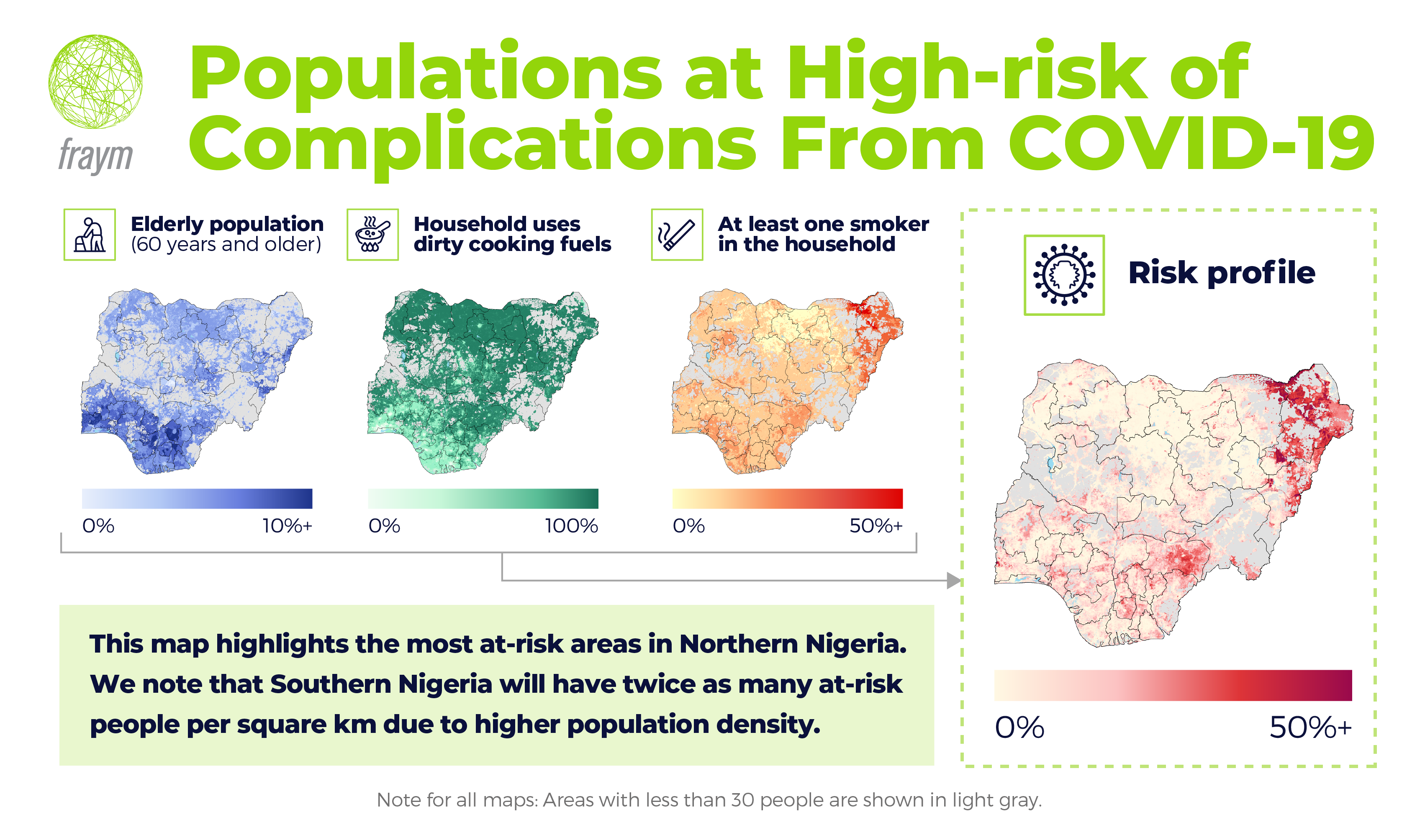
Geographical location can also influence an individual's risk profile. People living in rural areas often have limited access to healthcare services, including specialists and emergency care. Environmental factors, such as air and water pollution, can also contribute to increased health risks in certain regions.
Areas with high population density are more susceptible to outbreaks of infectious diseases. The rapid spread of COVID-19 in densely populated urban areas highlighted the vulnerability of these communities. Furthermore, individuals living in areas affected by natural disasters or conflict are at increased risk due to displacement, lack of access to clean water and sanitation, and disruption of healthcare services.
The Impact of Emerging Health Threats
Emerging infectious diseases, like COVID-19, disproportionately impact high-risk populations. These groups are more likely to experience severe illness, hospitalization, and death. The COVID-19 pandemic exposed the deep-seated health inequities that exist in many societies.
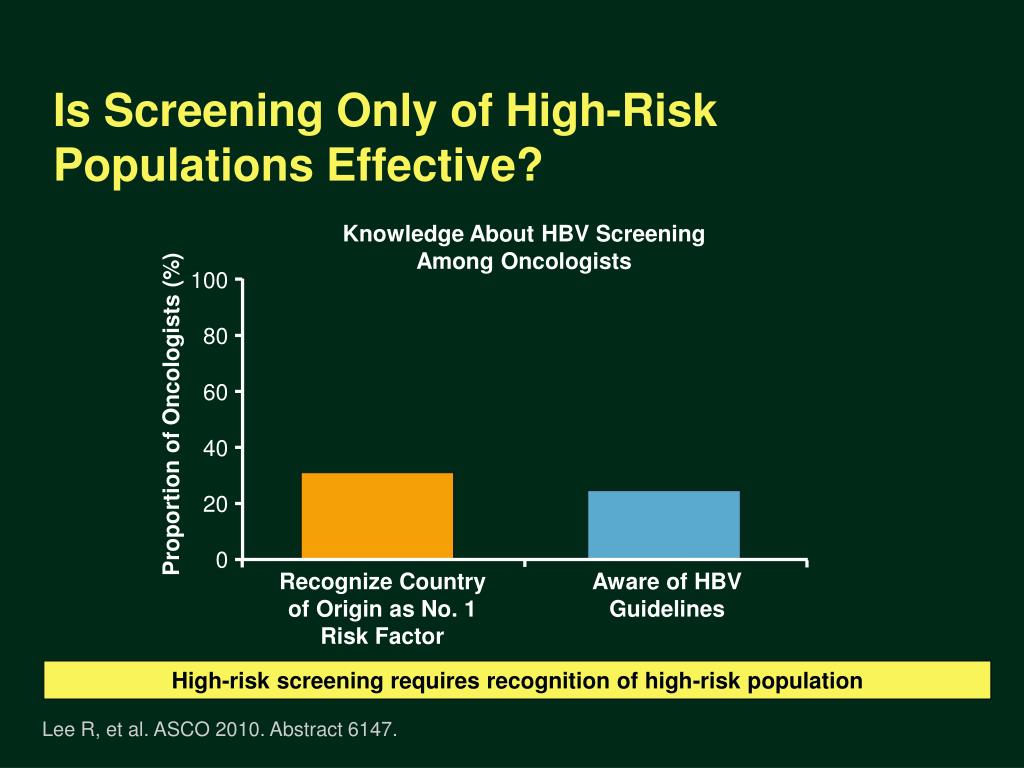
Vaccination campaigns are crucial for protecting high-risk populations from infectious diseases. However, vaccine hesitancy and limited access to vaccines can hinder these efforts. Targeted outreach and education programs are needed to address these barriers and ensure equitable access to vaccines for all.
Climate change poses a significant threat to public health, particularly for vulnerable populations. Extreme weather events, such as heatwaves, floods, and droughts, can exacerbate existing health conditions and increase the risk of infectious diseases. Addressing climate change is essential for protecting the health and well-being of all populations, especially those most at risk.
Moving Forward: Protecting Vulnerable Populations
Protecting high-risk populations requires a comprehensive and coordinated approach. This includes strengthening public health infrastructure, improving access to healthcare, addressing social determinants of health, and promoting health equity.
Data collection and analysis are essential for identifying and monitoring high-risk populations. This information can be used to target interventions and allocate resources effectively. Collaboration between healthcare providers, public health agencies, and community organizations is crucial for delivering coordinated care to vulnerable populations.
Ultimately, creating a more equitable and resilient healthcare system requires a commitment to addressing the root causes of health disparities. This includes tackling systemic racism, poverty, and other forms of discrimination. By investing in the health and well-being of all populations, we can create a society where everyone has the opportunity to thrive.
.jpg)