How Common Is Relapse After Stem Cell Transplant
Stem cell transplants, a lifeline for many battling blood cancers and other severe illnesses, face a harsh reality: relapse. New data reveals the frequency and factors influencing this recurrence, demanding increased vigilance and innovative solutions.
This article examines the prevalence of relapse post-stem cell transplant, analyzing who is most vulnerable, when relapse typically occurs, where the research points to weaknesses, and how advancements are striving to improve long-term outcomes.
Relapse Rates: A Concerning Reality
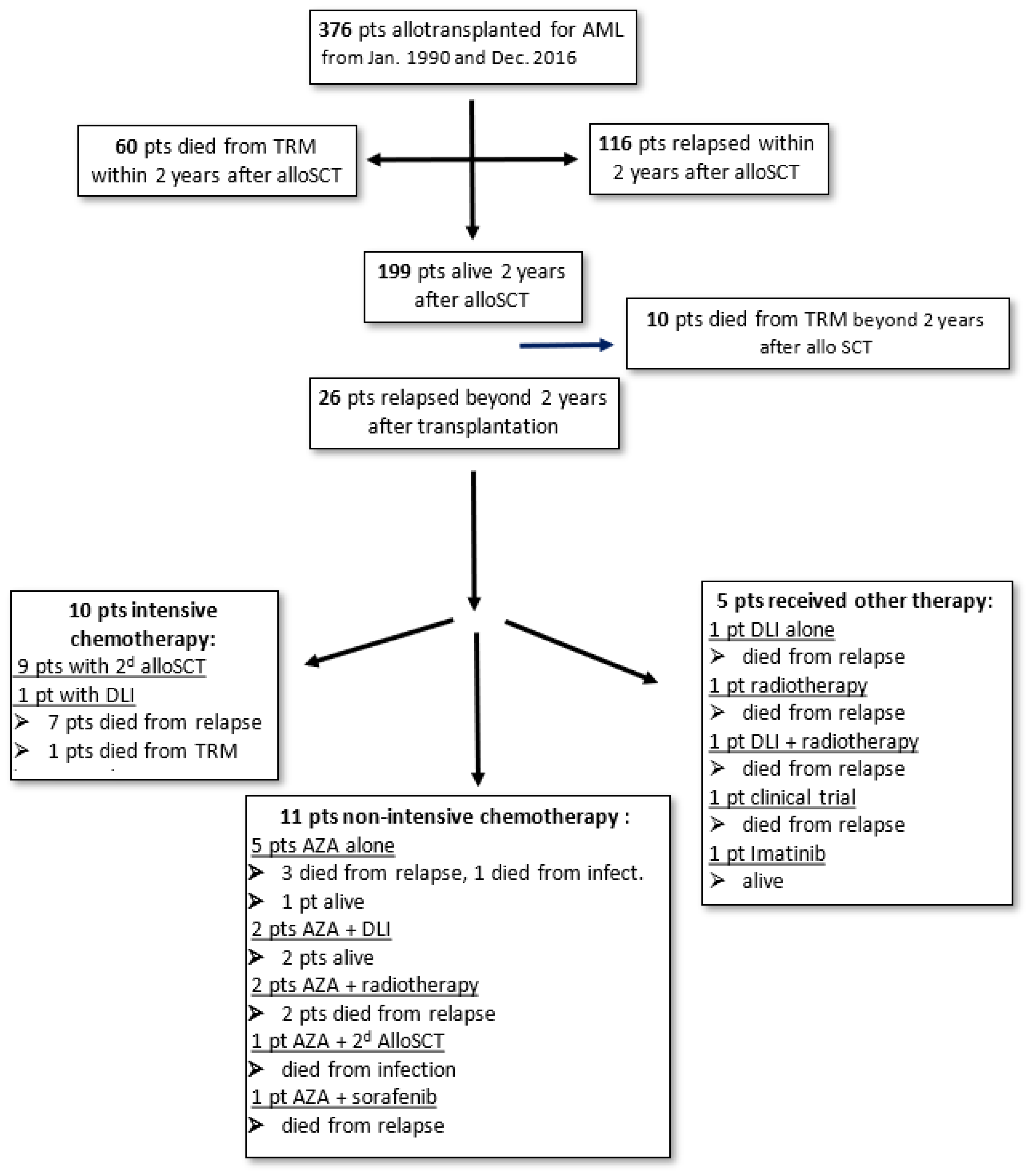
Relapse rates after stem cell transplant vary widely depending on the underlying disease, the type of transplant (autologous or allogeneic), and the patient's overall health. For example, in acute myeloid leukemia (AML), relapse rates can range from 20% to 50% within the first few years post-transplant, according to studies published in Blood, a leading hematology journal. These figures highlight a significant unmet need for improved relapse prevention strategies.
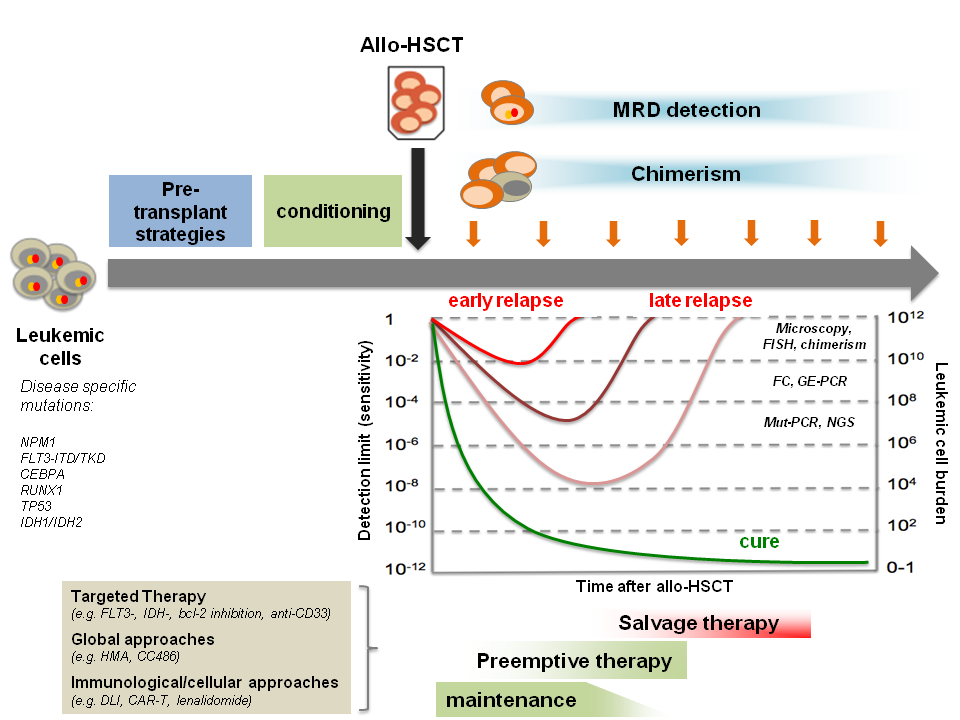
Studies by the Center for International Blood and Marrow Transplant Research (CIBMTR) show that patients with high-risk disease features at the time of transplant are more likely to relapse. Minimal residual disease (MRD), the presence of even a small number of cancer cells after treatment, is a strong predictor of relapse across various hematologic malignancies.
Who Is Most at Risk?
Several factors increase the risk of relapse after stem cell transplant. Patients with advanced disease stage at the time of transplant, those who didn't achieve complete remission before transplant, and those with specific genetic mutations are at higher risk.
Older patients often have a more challenging time tolerating the transplant process and may experience higher relapse rates. The type of stem cell source, whether from a matched related donor, unrelated donor, or umbilical cord blood, also influences relapse risk, with mismatched donors potentially leading to higher rates of graft-versus-host disease (GVHD) and relapse in some cases.
When Does Relapse Typically Occur?
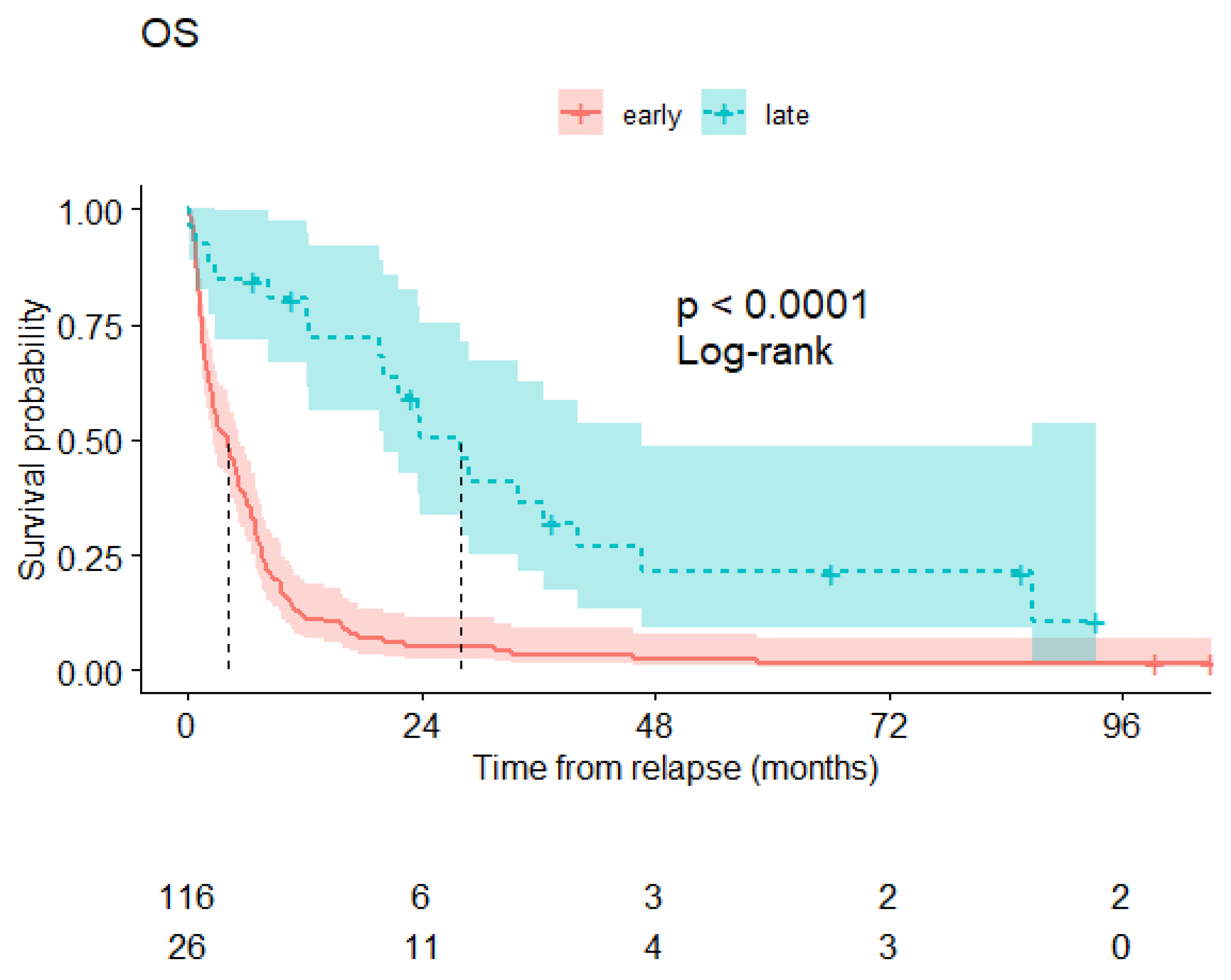
The timing of relapse is crucial for determining treatment strategies. Most relapses occur within the first two years after stem cell transplant.
Early relapses, those occurring within the first year, are often more aggressive and challenging to treat. Late relapses, occurring after two years, may indicate the survival of quiescent disease cells that were resistant to the initial transplant regimen.
Where Are the Weaknesses in Current Approaches?
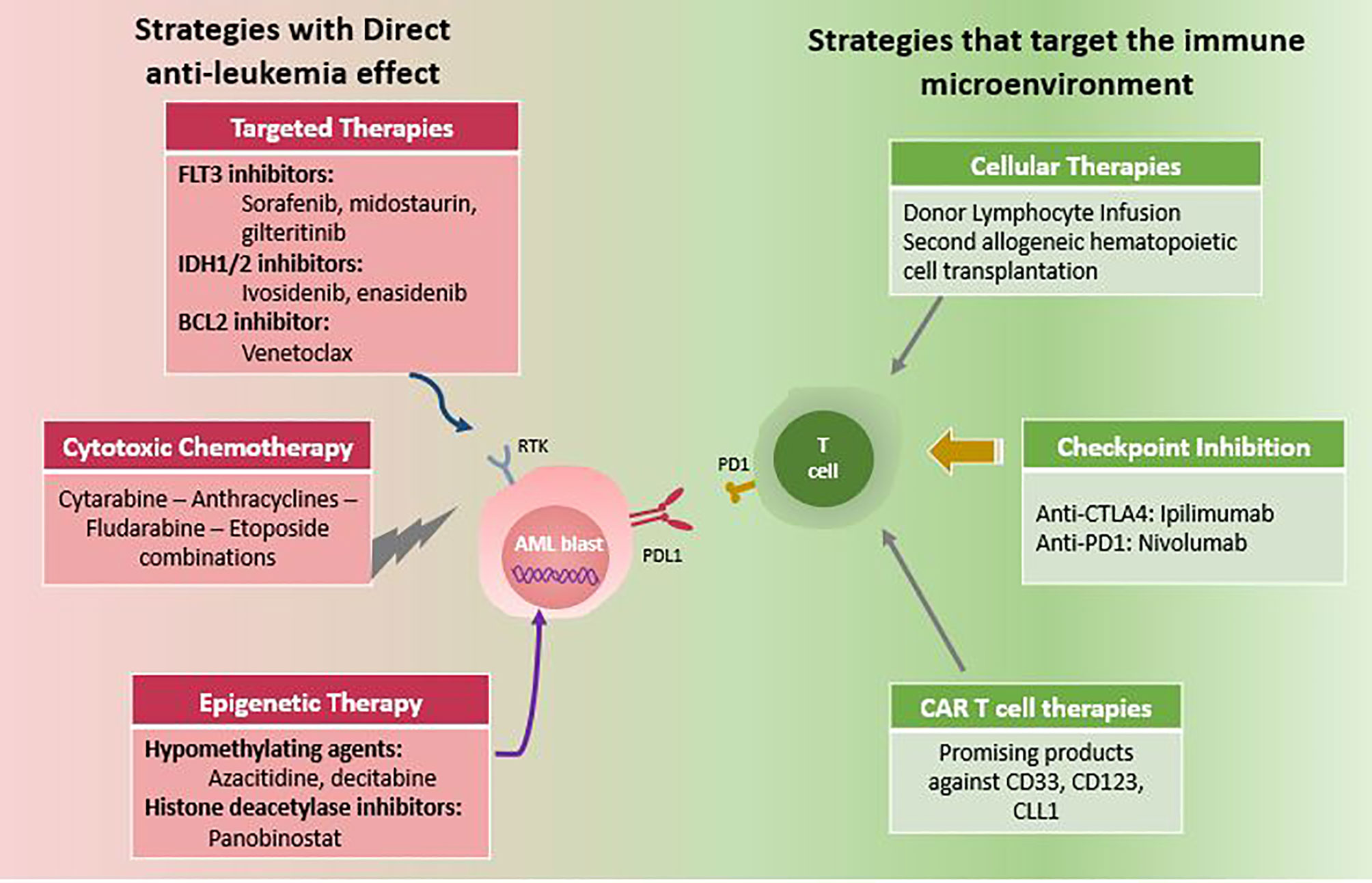
Current transplant regimens, while effective in many cases, still have limitations. The intensity of the conditioning regimen, the chemotherapy and/or radiation given before transplant, can impact relapse risk.
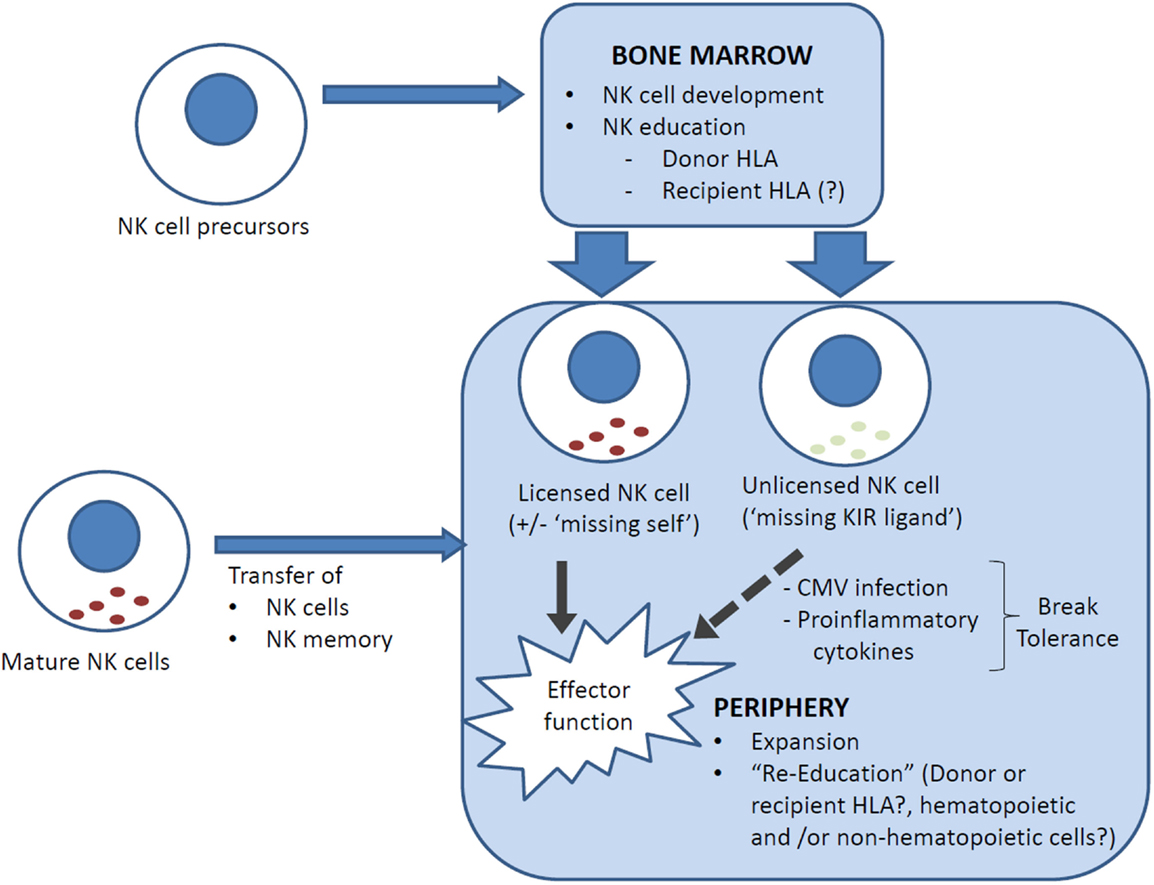
While more intense regimens can eradicate more cancer cells, they also increase the risk of toxicity and complications. Graft-versus-tumor (GVT) effect, where the donor immune cells attack any remaining cancer cells, is a key mechanism for preventing relapse in allogeneic transplants, but can be unpredictable.
How Are Advancements Improving Outcomes?
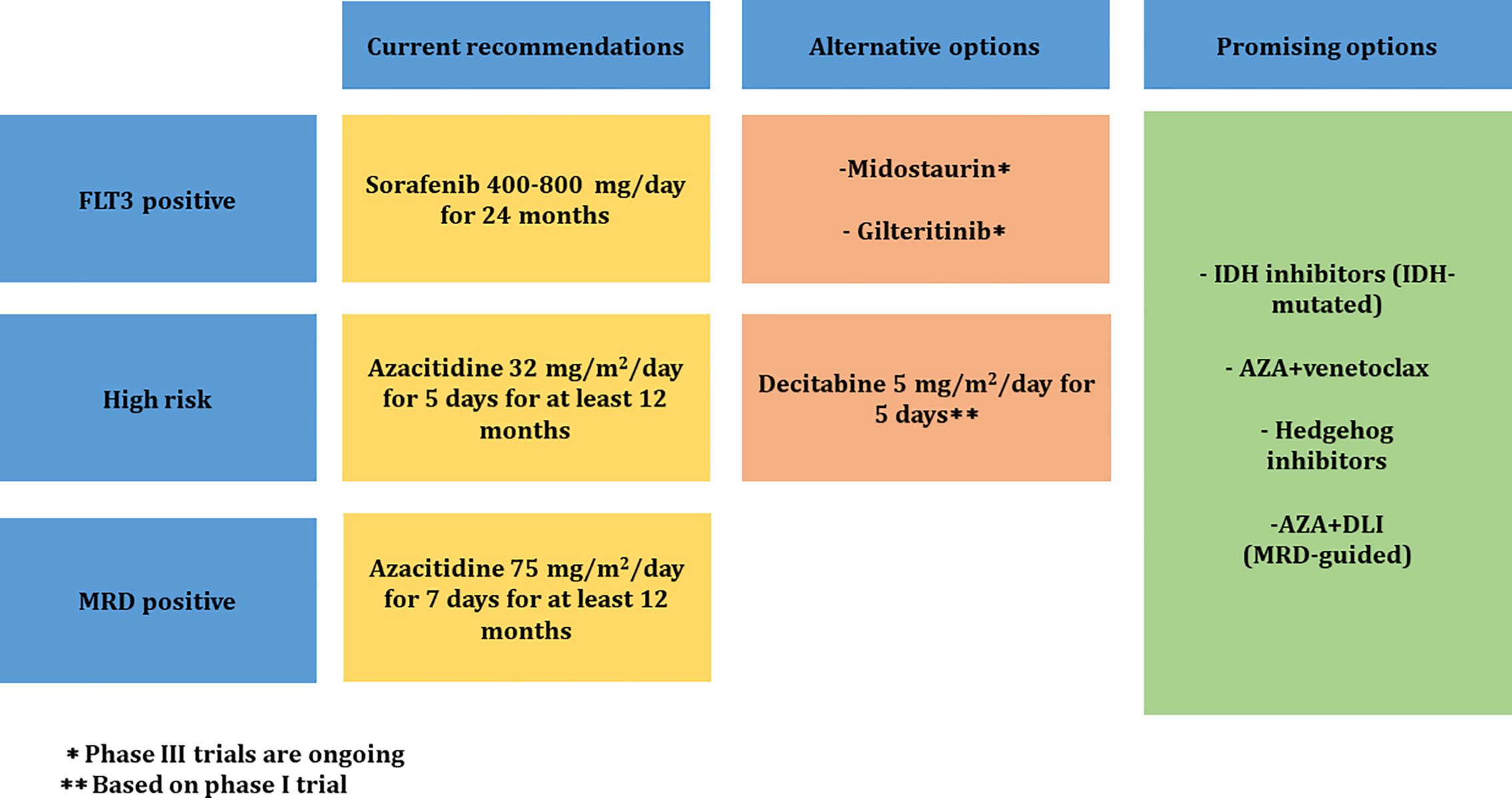
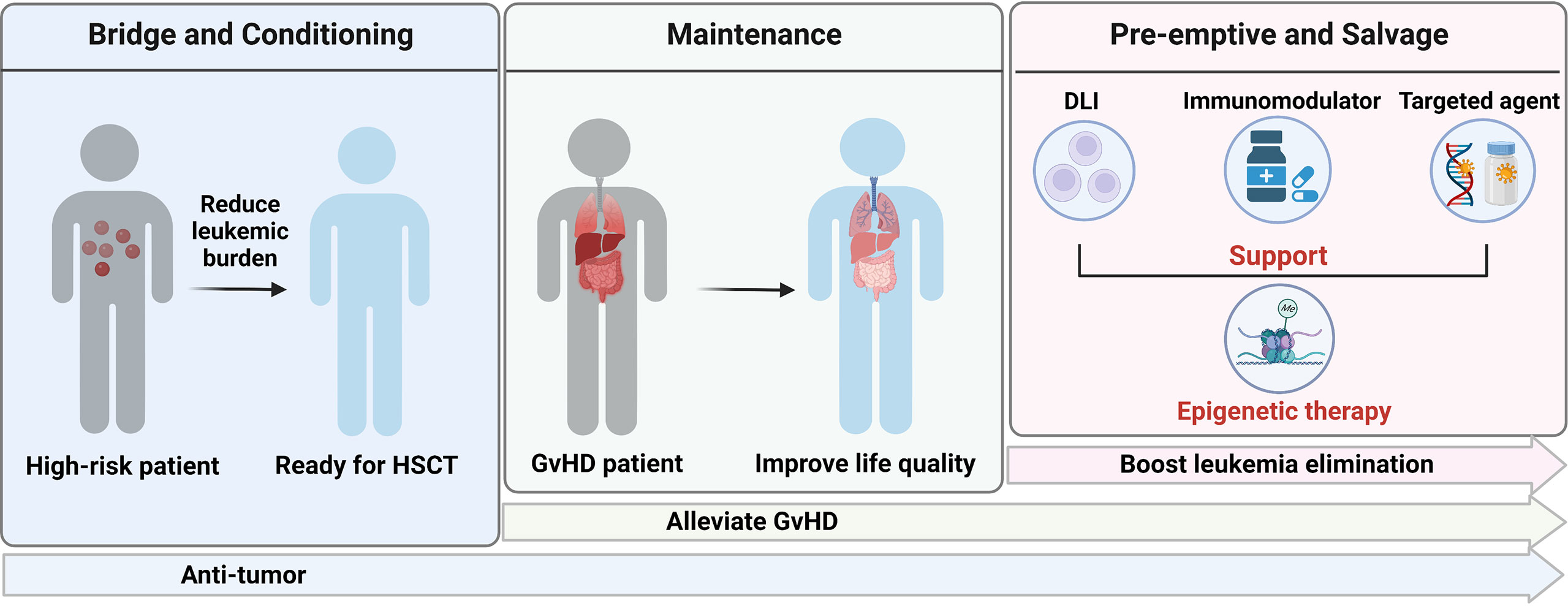
Significant advancements are being made to reduce relapse rates after stem cell transplant. Post-transplant maintenance therapy, using drugs like azacitidine or lenalidomide, has shown promise in reducing relapse risk in certain diseases, such as AML and multiple myeloma.
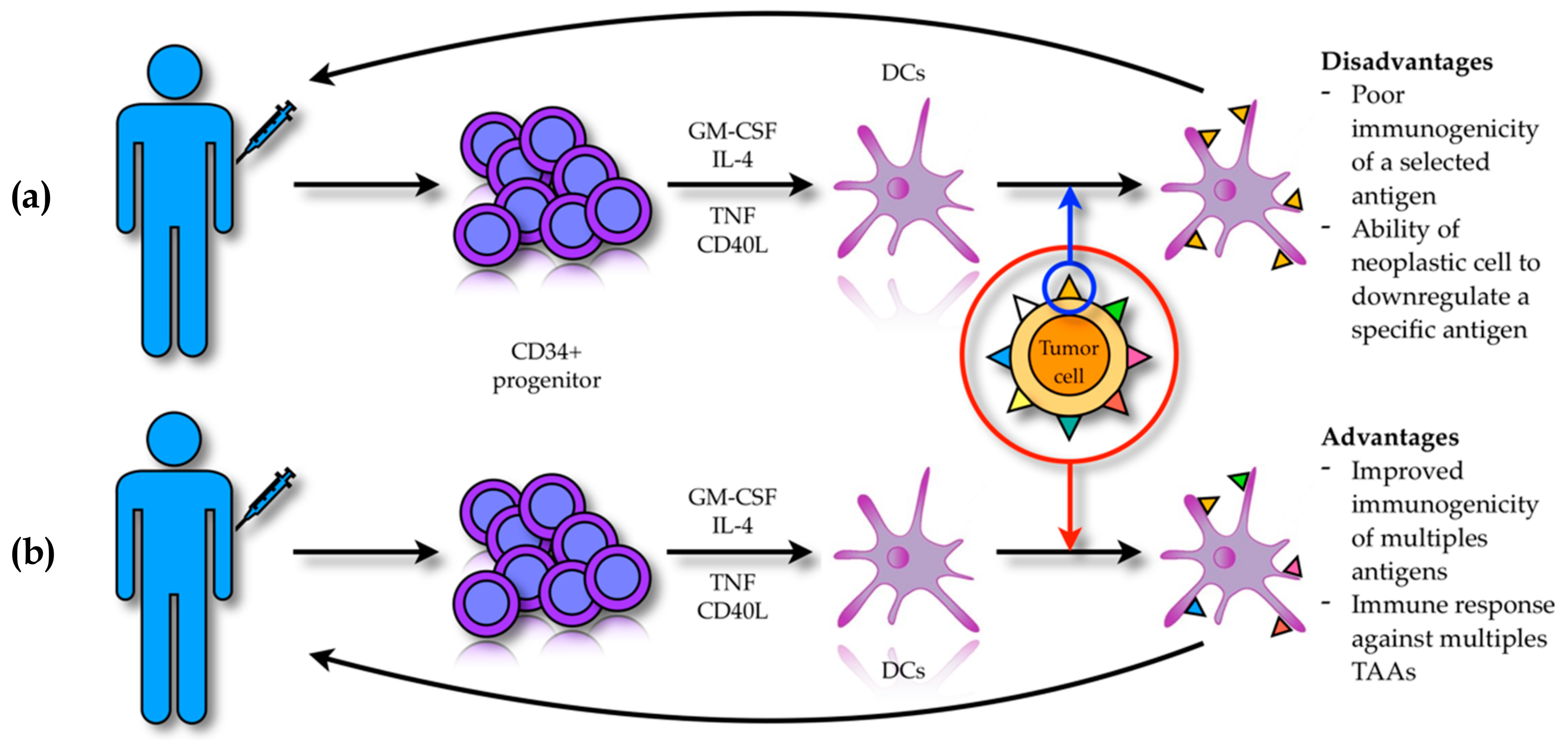
Chimeric antigen receptor (CAR) T-cell therapy, a type of immunotherapy, is being explored as a treatment option for relapsed disease after transplant. MRD monitoring, using highly sensitive techniques, allows for early detection of disease recurrence and prompt intervention.
Clinical trials are investigating novel strategies to enhance the GVT effect while minimizing GVHD. These include the use of donor lymphocyte infusions (DLIs) and checkpoint inhibitors.
Future Directions
Ongoing research is focused on identifying biomarkers that can predict relapse risk. Personalized treatment approaches are being developed to tailor transplant regimens and post-transplant therapies based on individual patient characteristics and disease biology.
Improving our understanding of the mechanisms underlying relapse and developing more effective strategies to prevent and treat recurrence remain critical priorities in the field of stem cell transplantation.