How Does Your Immune System Discover Your Eyes
For decades, the eye has been considered an immune-privileged site, shielded from the full force of the body's defenses. But recent research is challenging this long-held belief, revealing intricate pathways through which the immune system can, and sometimes must, interact with the eye.
Understanding how the immune system "discovers" the eye, and the mechanisms that regulate this interaction, is crucial for developing effective treatments for a range of ocular diseases, from autoimmune conditions to infections. This article explores the latest findings on this complex interplay, delving into the cellular and molecular processes involved.
The Immune Privilege Paradigm
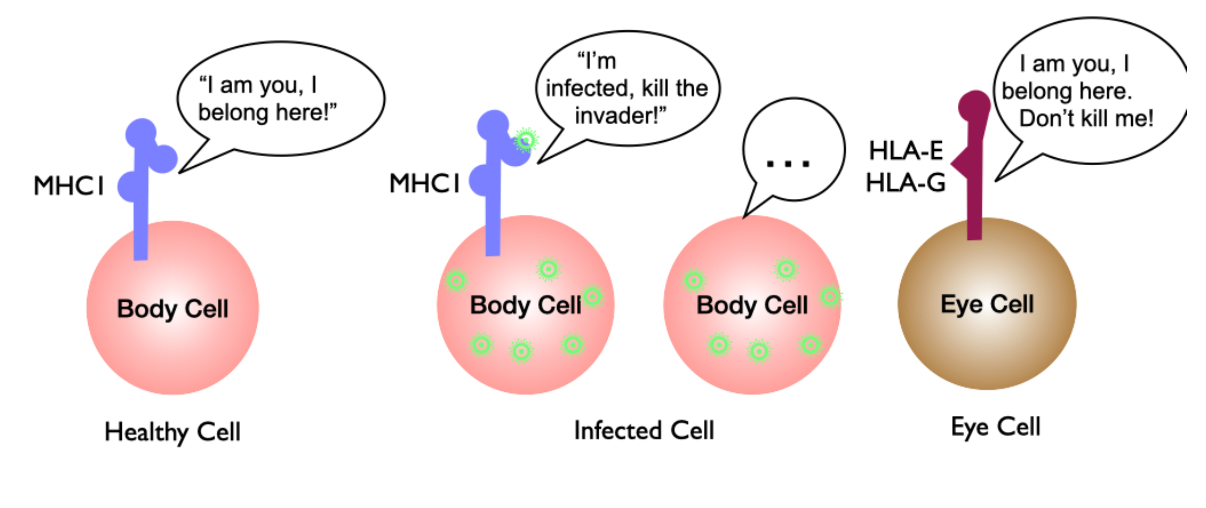
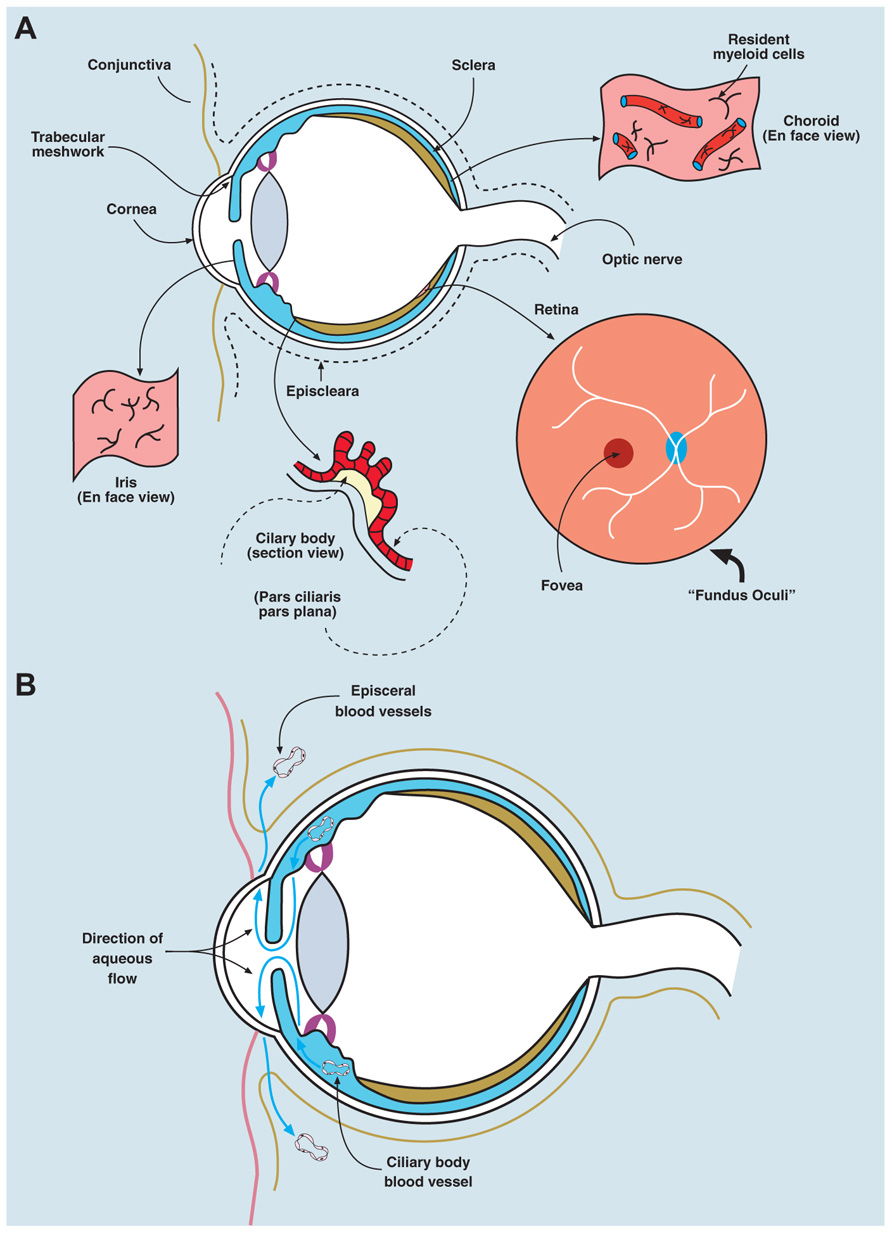
Traditionally, the eye's immune privilege was attributed to several factors. These included physical barriers like the blood-retinal barrier, the production of immunosuppressive factors within the eye, and the limited expression of major histocompatibility complex (MHC) molecules on ocular cells.
The blood-retinal barrier, similar to the blood-brain barrier, restricts the entry of immune cells and large molecules into the eye. This barrier helps maintain a stable microenvironment necessary for optimal visual function. It is composed of tight junctions between endothelial cells in the retinal capillaries and between retinal pigment epithelium (RPE) cells.
Additionally, ocular cells produce factors like transforming growth factor-beta (TGF-β) and pigment epithelium-derived factor (PEDF), which suppress immune cell activation and proliferation. These immunosuppressive factors contribute to a tolerogenic environment within the eye.
Breaching the Defenses: How the Immune System Gains Access
Despite these protective mechanisms, the immune system can and does interact with the eye. This interaction can be beneficial in clearing infections or repairing tissue damage, but it can also be detrimental, leading to inflammation and vision loss.
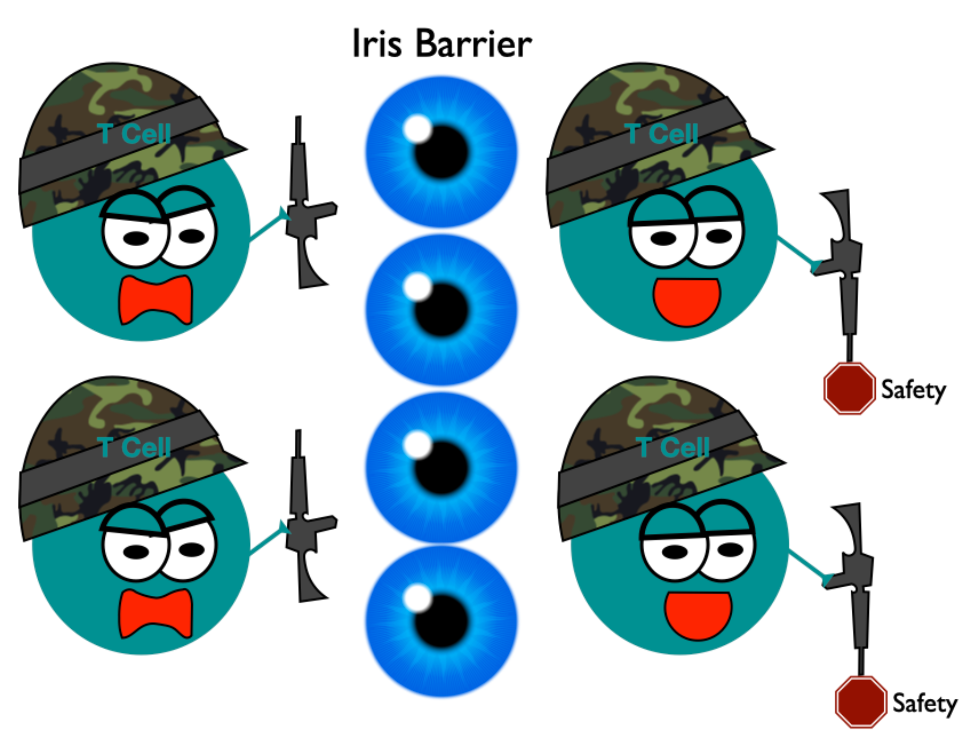
One key pathway involves the breakdown of the blood-retinal barrier. Inflammation, infection, or trauma can compromise the integrity of this barrier, allowing immune cells to enter the eye. This breach allows for the recruitment of immune cells like T cells and macrophages.
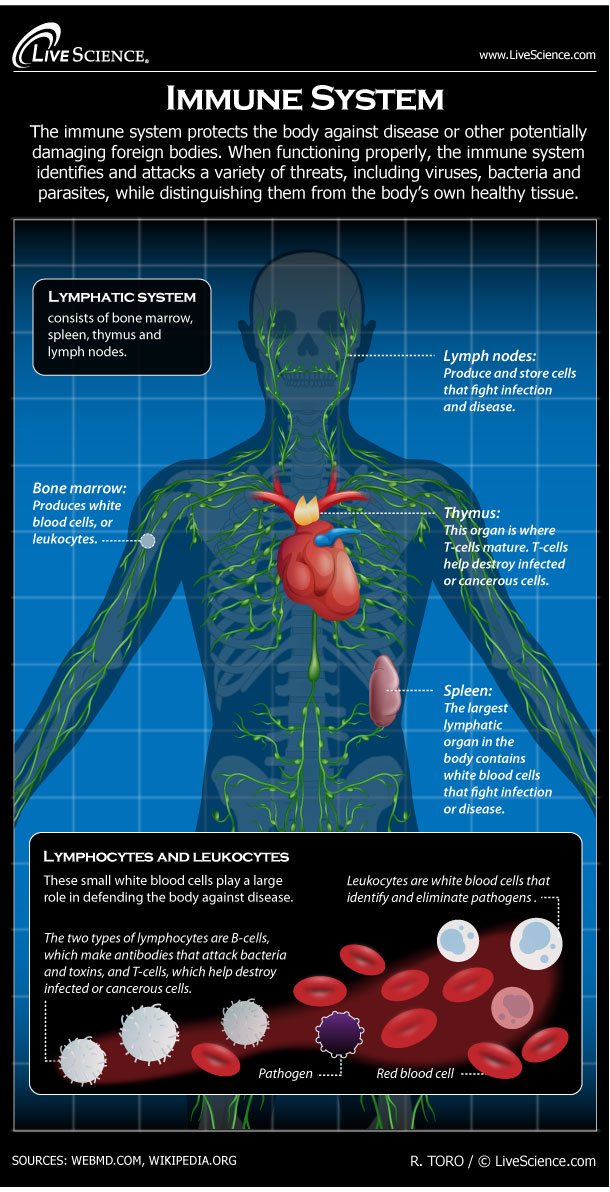
Another route involves the lymphatic system, specifically the cervical lymph nodes. Although the eye lacks traditional lymphatic vessels, recent research has shown that immune cells can migrate from the eye to these lymph nodes, where they can activate an immune response. This drainage occurs primarily through the choroid.
The Role of Antigen-Presenting Cells
Antigen-presenting cells (APCs), such as dendritic cells and macrophages, play a crucial role in initiating an immune response in the eye. These cells capture antigens (foreign substances) and present them to T cells in the lymph nodes, triggering an adaptive immune response.
Resident APCs within the eye, as well as those recruited from the bloodstream, can participate in antigen presentation. This process can lead to the activation of both protective and pathogenic immune responses, depending on the nature of the antigen and the context in which it is presented.
Interestingly, studies have shown that APCs in the eye can also induce T regulatory cells (Tregs), which suppress immune responses and maintain immune tolerance. This highlights the complex and finely tuned nature of the immune response in the eye.
Implications for Ocular Disease
Understanding how the immune system interacts with the eye has significant implications for the treatment of ocular diseases. For example, in autoimmune conditions like uveitis, the immune system mistakenly attacks the eye's own tissues.
Knowing the specific immune cells and molecules involved in uveitis can help researchers develop targeted therapies that suppress the harmful immune response without compromising the eye's overall health. This could involve the use of biologic drugs that block the action of specific inflammatory cytokines.
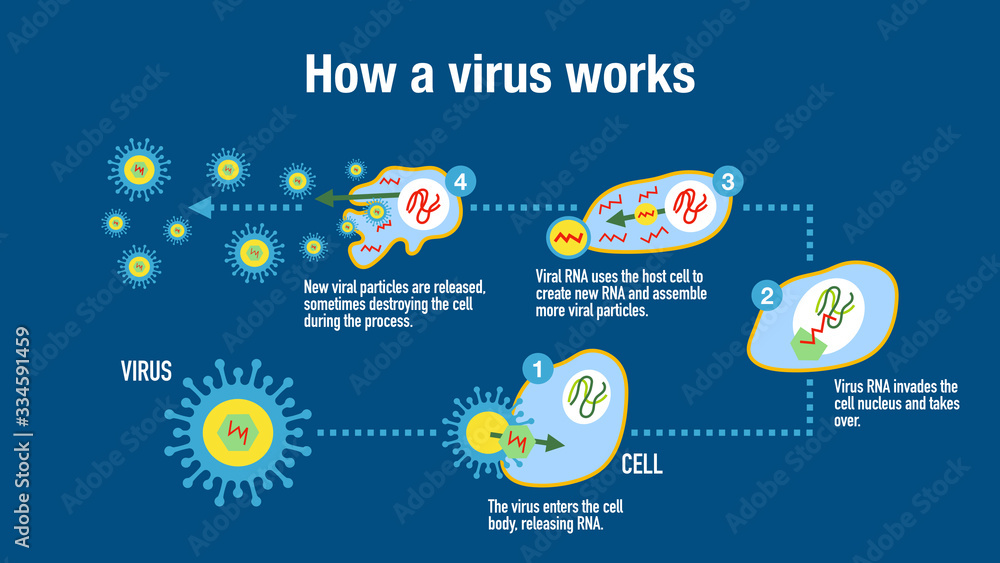
Similarly, in infectious diseases like viral retinitis, understanding how the immune system clears the infection can guide the development of effective antiviral therapies and immunomodulatory strategies. Boosting the local immune response in a controlled manner can help eliminate the virus while minimizing damage to the retina.
Future Directions
Research into the eye's immune system is ongoing, with a focus on identifying new targets for therapeutic intervention. One promising area is the development of therapies that promote immune tolerance in the eye.
This could involve using gene therapy to deliver immunosuppressive factors directly to the eye or developing nanoparticles that deliver antigens in a way that induces Treg activation. Ultimately, a deeper understanding of the eye's immune system will lead to more effective and targeted treatments for a wide range of ocular diseases.
The ability to manipulate the immune system within the eye, either to enhance protection or suppress inflammation, holds immense promise for improving the lives of individuals suffering from vision-threatening conditions. The eye, once considered an isolated fortress, is now recognized as a dynamic participant in the body's complex immune landscape. Further research is critical to fully unlocking its secrets.





![How Does Your Immune System Discover Your Eyes [DIAGRAM] Diagram Of The Human Immune System - MYDIAGRAM.ONLINE](https://jamanetwork.com/data/Journals/JAMA/933829/jpg150012fa.png)