How Effective Is One Dose Of Japanese Encephalitis Vaccine

Japanese encephalitis (JE), a mosquito-borne viral disease that can cause severe neurological damage, poses a significant threat in many parts of Asia and the Western Pacific. While vaccination is a cornerstone of prevention, questions remain about the effectiveness of a single dose, especially in regions where JE is endemic.
This article examines the available evidence regarding the efficacy of one dose of the JE vaccine, exploring its potential benefits, limitations, and the implications for public health strategies.
Understanding Japanese Encephalitis and the Need for Vaccination
JE is caused by the Japanese encephalitis virus (JEV), which is transmitted to humans through the bite of infected mosquitoes, primarily of the Culex species. The disease is most prevalent in rural, agricultural areas where rice cultivation and pig farming create ideal breeding grounds for the mosquitoes.
Symptoms range from mild, flu-like illness to severe encephalitis, characterized by seizures, coma, and long-term neurological disabilities. The mortality rate among those with encephalitis can be as high as 30%, and a significant proportion of survivors experience permanent neurological sequelae.
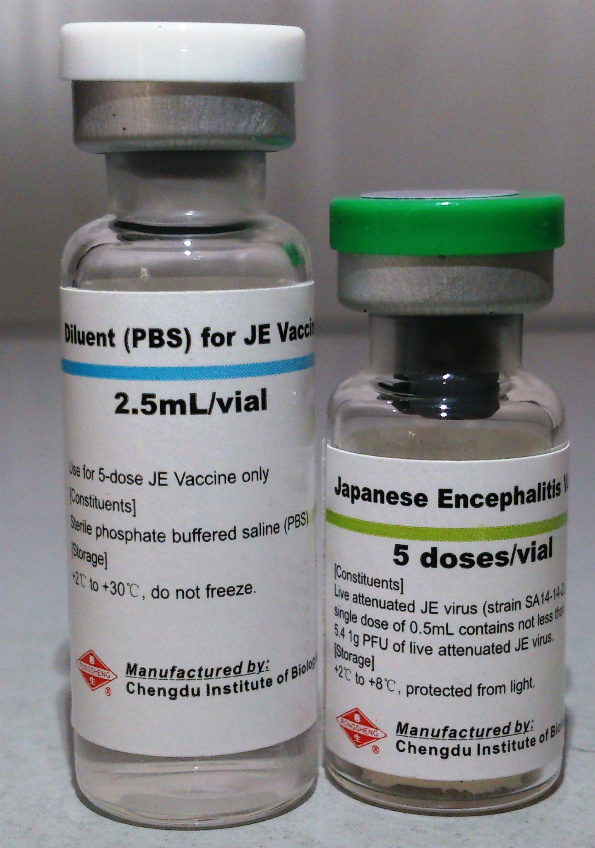
Vaccination is a highly effective method of preventing JE, with several types of vaccines available, including live attenuated vaccines, inactivated vaccines, and recombinant vaccines. These vaccines aim to stimulate the immune system to produce antibodies that protect against JEV infection.
The Effectiveness of a Single Dose: What the Evidence Says
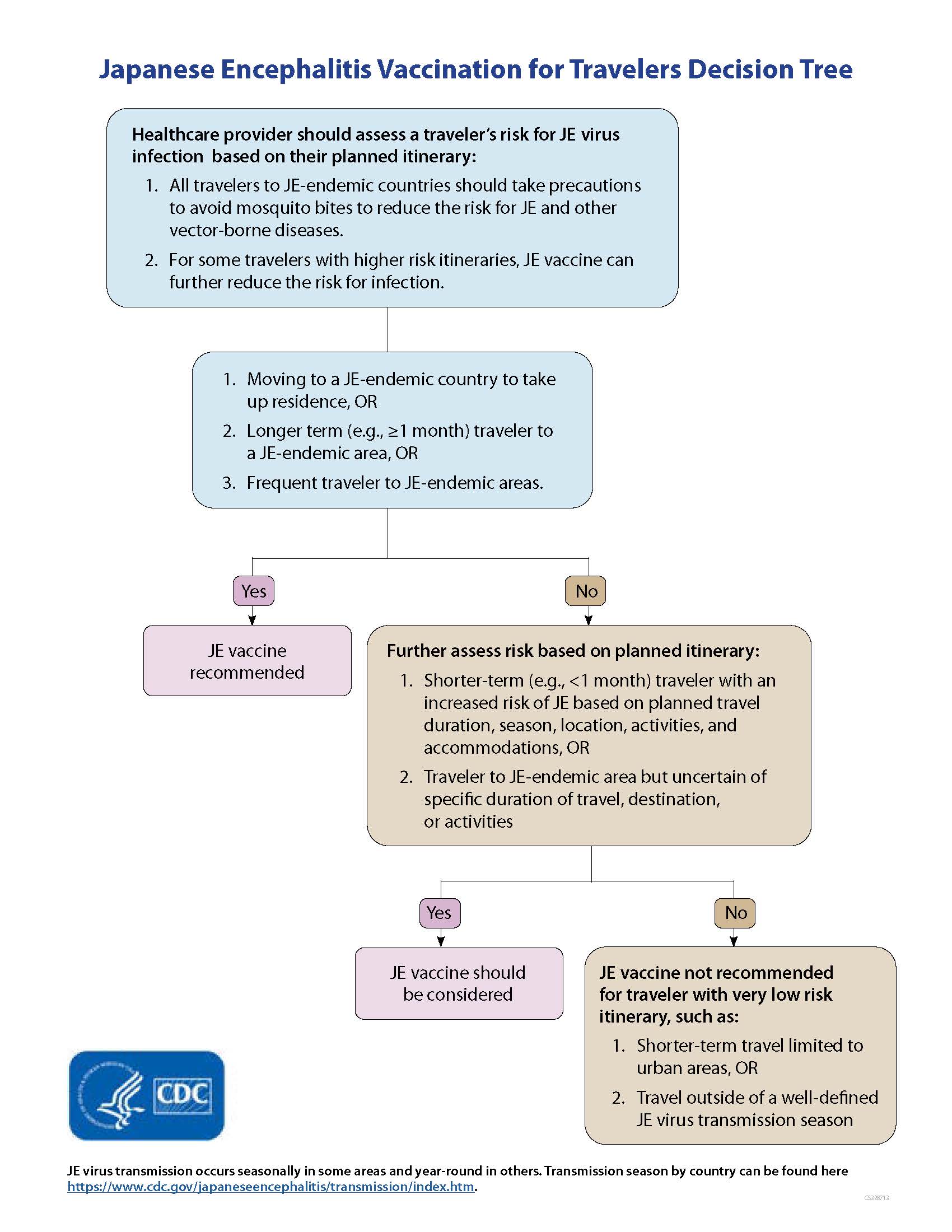
The question of single-dose efficacy is particularly relevant in resource-limited settings where implementing multi-dose schedules can be challenging. Studies have explored the immunogenicity and protective potential of one dose of JE vaccine.
Early studies on some inactivated vaccines, such as the mouse-brain derived inactivated vaccine, showed that a single dose could provide short-term protection, but the long-term immunity was questionable. This led to the recommendation for a two-dose primary series.
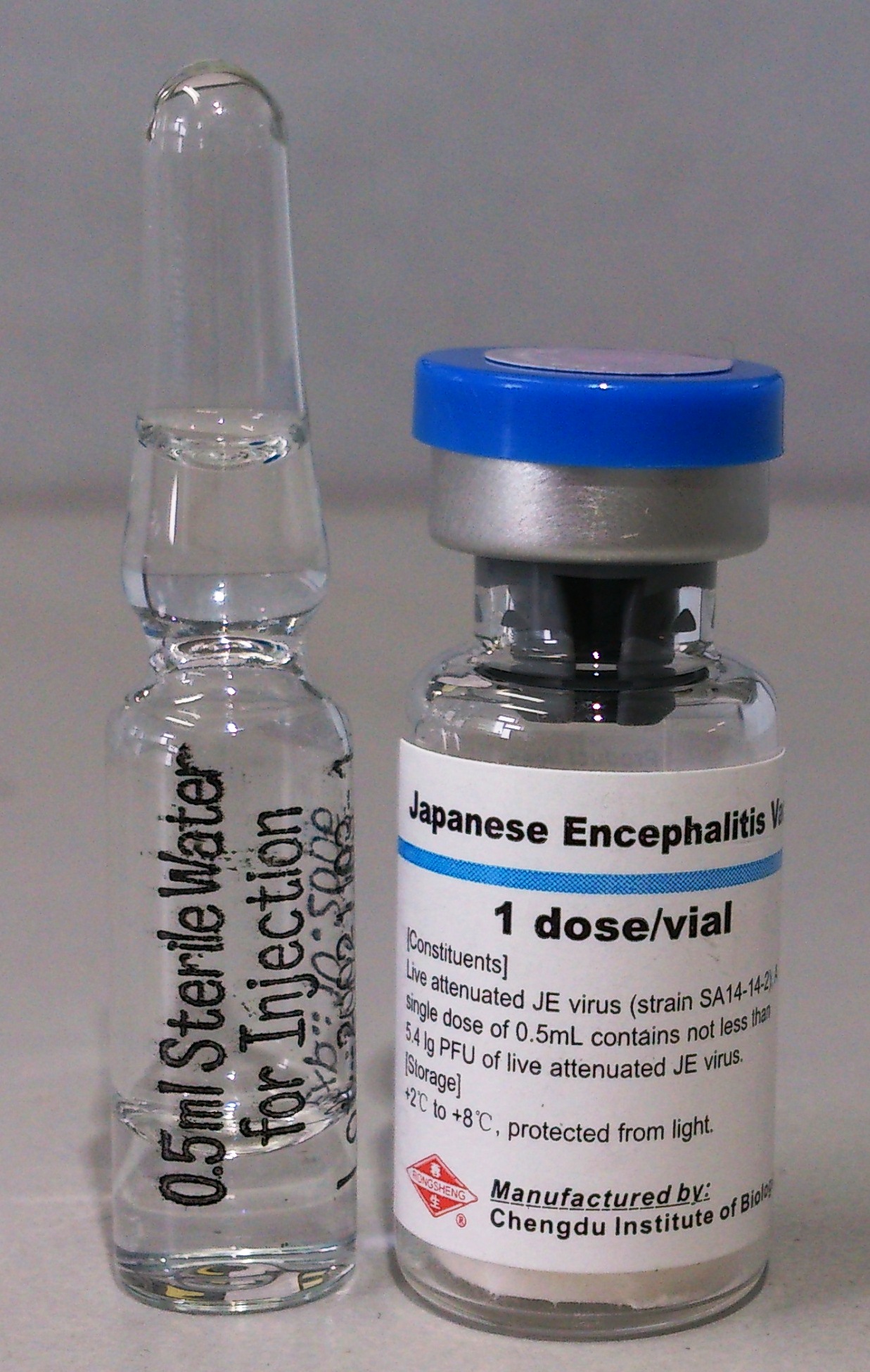
More recent research has focused on newer vaccines, including live attenuated vaccines like the SA 14-14-2 strain. Some studies suggest that a single dose of the SA 14-14-2 vaccine can induce a robust immune response, providing protection for at least a year, particularly in children.
However, the duration of protection offered by a single dose may vary depending on factors such as the individual's age, immune status, and the specific vaccine used. Studies from different regions have reported varying levels of seroconversion rates (the development of detectable antibodies) after a single dose.
Considerations and Limitations
While a single dose may offer some level of protection, it's important to acknowledge its limitations. Long-term studies are often needed to definitively assess the duration of immunity and the need for booster doses.
The World Health Organization (WHO) recommends a primary series of JE vaccination, typically consisting of two doses for inactivated vaccines. For live attenuated vaccines, a single dose is often considered sufficient for primary immunization in many national immunization programs, although boosters may be recommended later in life, depending on the risk of exposure.
The decision to use a single-dose or multi-dose schedule should be based on a comprehensive assessment of the local epidemiology, vaccine availability, cost-effectiveness, and logistical feasibility. Public health officials must consider the balance between providing some immediate protection through a single dose and aiming for more durable immunity with a complete series.
Furthermore, the emergence of new JEV genotypes and the potential for waning immunity underscore the need for ongoing surveillance and research to inform vaccination strategies. Constant evaluation of vaccine effectiveness is crucial.
Potential Impact and Implications
The effectiveness of a single dose of JE vaccine has significant implications for public health programs, especially in regions with limited resources. A single-dose strategy can allow for broader coverage and faster implementation of vaccination campaigns, particularly in emergency situations or areas with high transmission rates.
However, it's essential to ensure that the single dose provides adequate protection, especially for vulnerable populations like young children. Booster doses may be needed to maintain long-term immunity and prevent outbreaks.
For instance, in countries where JE is endemic, a single-dose campaign targeting children can significantly reduce the incidence of the disease in the short term. This approach is often combined with vector control measures, such as mosquito spraying and environmental management, to further reduce the risk of transmission.
Ongoing research and surveillance are essential to monitor the effectiveness of single-dose strategies and determine the optimal vaccination schedules for different populations and regions. This includes assessing the duration of immunity, the need for booster doses, and the impact of vaccination on disease incidence.
Conclusion
The effectiveness of a single dose of Japanese encephalitis vaccine is a complex issue that depends on factors such as the type of vaccine, the individual's immune response, and the local epidemiological context. While some vaccines, particularly live attenuated vaccines, may offer substantial protection with a single dose, long-term immunity and the need for booster doses remain important considerations.
Public health authorities must carefully weigh the benefits and limitations of single-dose strategies, considering the broader context of disease control efforts. By combining vaccination with other preventive measures, such as vector control and public awareness campaigns, it is possible to significantly reduce the burden of Japanese encephalitis and protect vulnerable populations.
Continued research and surveillance are crucial to refine vaccination strategies and ensure that they remain effective in the face of evolving viral strains and changing epidemiological patterns. Prioritizing JE control will require both innovative approaches and sustained commitment from healthcare professionals and policymakers worldwide.






.png?format=1500w)