How Long Does It Take To Stop Period On Testosterone

The air crackled with nervous energy in the support group meeting. Sunlight streamed through the window, illuminating dust motes dancing in the air as several people shared their experiences, their voices a blend of hope and uncertainty. Sarah, a young trans man with bright eyes and a determined spirit, tentatively raised his hand. "I'm starting testosterone soon," he began, his voice slightly trembling. "And I'm just wondering… how long until it… stops?"
The question of how long it takes to stop menstruating on testosterone (T) is a common and crucial one for many transgender and non-binary individuals embarking on hormone replacement therapy. While the timeframe varies considerably from person to person, understanding the general expectations, factors influencing the process, and potential challenges is vital for informed decision-making and realistic expectations. This article will delve into the complexities of this journey, providing insights and shedding light on what to expect.
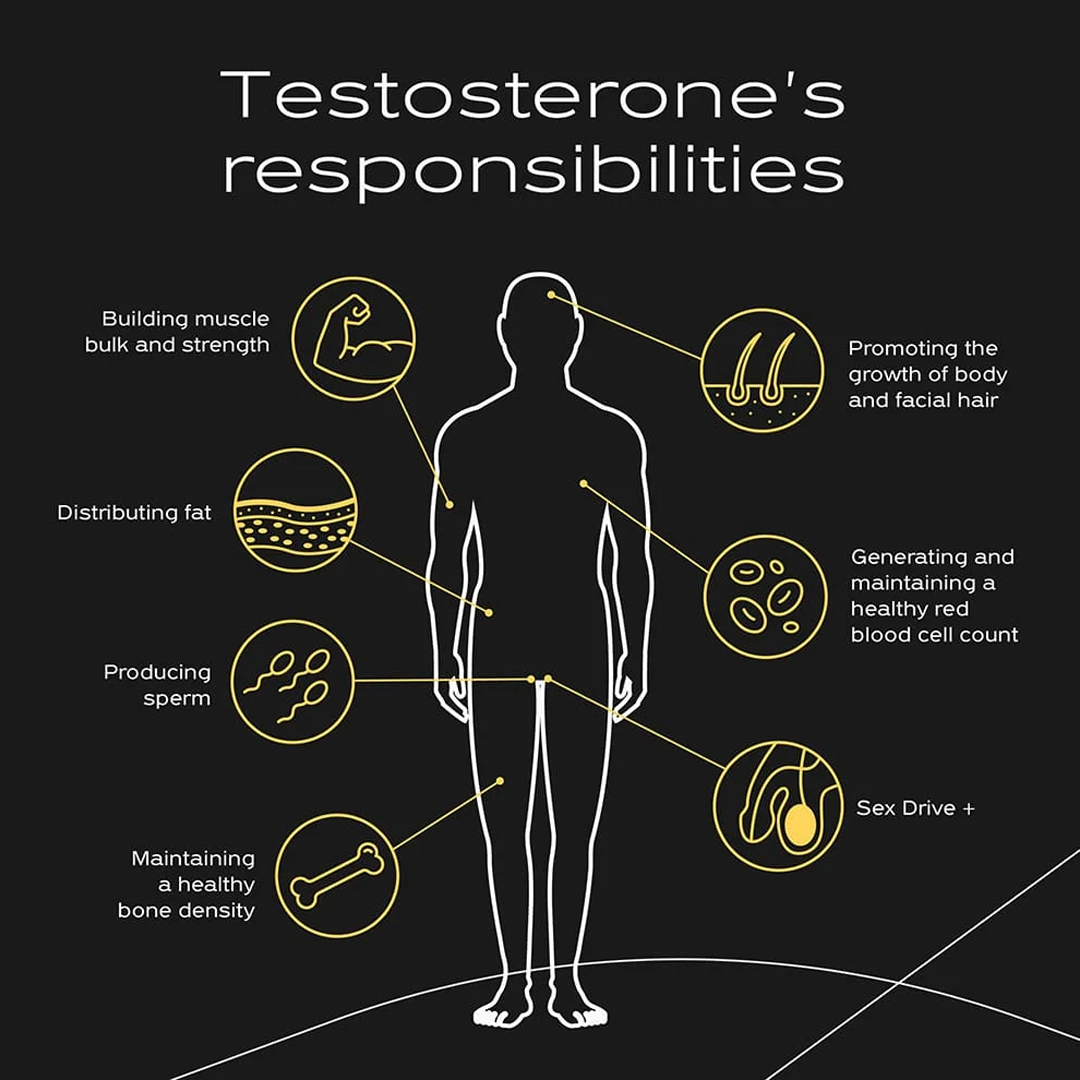
Understanding Testosterone and Menstruation
To understand the process of menstruation cessation on testosterone, it's important to first understand the hormonal changes at play. Testosterone is an androgen, a hormone that plays a key role in developing and maintaining male characteristics. When a person assigned female at birth begins taking testosterone, it gradually suppresses estrogen production.
This reduction in estrogen is what ultimately leads to the stopping of menstrual cycles. However, the body's response to hormonal changes is not uniform, and individual factors significantly influence the timeline.
The Timeline: What to Expect
While there's no one-size-fits-all answer, some general timelines can be outlined. Many individuals experience changes in their menstrual cycle within the first few months of starting testosterone. These changes often include lighter, shorter, and less frequent periods.
For some, menstruation may stop completely within 2-6 months. However, it's crucial to understand that this is just an average. Others may experience irregular bleeding or spotting for a longer period, sometimes up to a year or more.
Factors Influencing the Timeline
Several factors can impact how quickly menstruation ceases on testosterone. Dosage is a critical aspect. Individuals on higher doses of testosterone may experience a faster cessation compared to those on lower doses.
Individual physiology also plays a significant role. Each person's body responds differently to hormonal changes, influenced by genetics, metabolism, and overall health. Pre-existing conditions, such as polycystic ovary syndrome (PCOS), can also affect the timeline. Body Mass Index (BMI) can be a factor, with some studies suggesting that individuals with higher BMIs may experience a slower cessation of menstruation.
The method of testosterone administration can also be a factor. Injections, gels, and patches can all have slightly different absorption rates and hormonal fluctuations, which can influence the overall process.
Navigating the Transition: Practical Tips and Considerations
Starting testosterone is a significant step, and managing expectations is crucial. It’s essential to have open and honest communication with your healthcare provider. Regular check-ups and bloodwork will help monitor hormone levels and ensure that the testosterone dosage is appropriate.
Keep a detailed record of your menstrual cycles, noting any changes in frequency, duration, and flow. This information can be invaluable in tracking progress and identifying any potential issues. Remember, every body is different. Patience and self-compassion are paramount during this transition.
Addressing Potential Concerns
It's not uncommon to experience spotting or breakthrough bleeding during the initial months of testosterone therapy. While this is often a normal part of the process, it's essential to discuss any unusual or persistent bleeding with your healthcare provider. They can help rule out other potential causes and provide appropriate guidance.
Some individuals may experience mood changes or other side effects during this transition. Open communication with your healthcare team and support network can help manage these challenges effectively. Finding a supportive community of other trans and non-binary individuals can also provide invaluable emotional support and shared experiences. Many find that having a therapist or counselor who specializes in gender-affirming care to be very helpful.
The Role of Healthcare Providers
A knowledgeable and supportive healthcare provider is an indispensable ally in this journey. An endocrinologist or a physician specializing in transgender healthcare can provide personalized guidance and monitor your progress. They can adjust your testosterone dosage as needed and address any concerns or questions you may have.
They can also help you understand the potential risks and benefits of testosterone therapy and guide you through the various options available. Don't hesitate to seek a second opinion if you feel your current provider is not adequately meeting your needs.
Beyond Menstruation: Other Effects of Testosterone
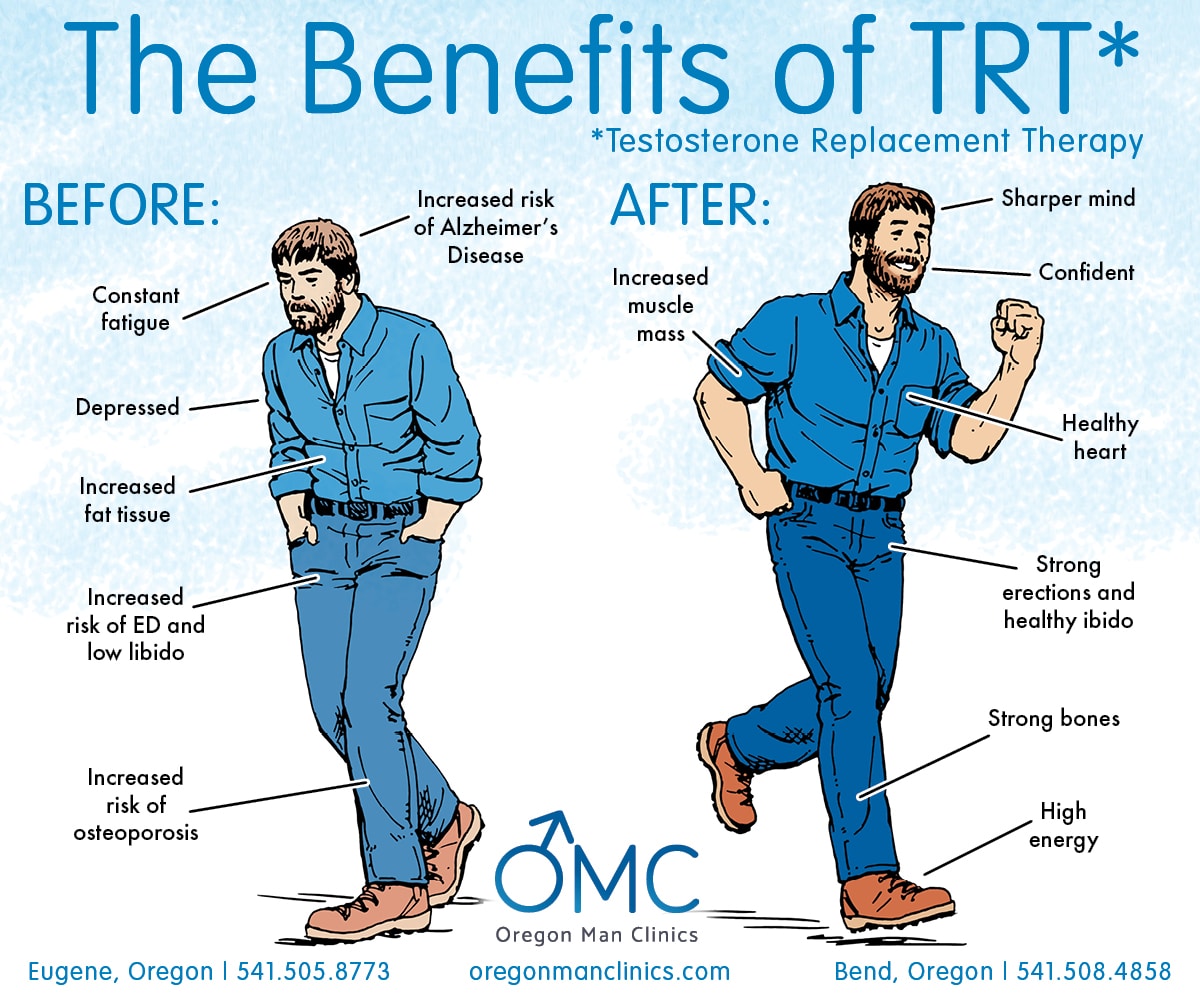
While the cessation of menstruation is a significant milestone, it's important to remember that testosterone therapy brings about a range of other physical and emotional changes. These may include increased muscle mass, deepening of the voice, facial hair growth, and changes in skin texture.
Many individuals also experience increased energy levels and improved mood. It's essential to be prepared for these changes and to embrace them as part of your transition. Understanding the broader spectrum of effects can contribute to a more fulfilling and informed experience with hormone therapy.
The Long-Term Perspective
For most individuals, the cessation of menstruation on testosterone is a permanent change. However, if testosterone therapy is stopped, menstrual cycles will typically resume. It's crucial to carefully consider the long-term implications of hormone therapy before starting. Discuss your long-term goals and expectations with your healthcare provider to ensure you are making informed decisions that align with your individual needs.
Consistent monitoring and follow-up care are essential to maintaining optimal health and well-being throughout your transition. Remember that your journey is unique, and your experiences may differ from others. Embrace your individuality and celebrate your progress along the way.
The journey to stopping menstruation on testosterone can be a complex and multifaceted one. By understanding the potential timeline, influencing factors, and available support resources, individuals can navigate this transition with greater confidence and self-assurance. Patience, communication, and self-compassion are key ingredients in this journey, and with the right support, it can be a truly transformative experience.