How Long Is Immune System Compromised After Chemo
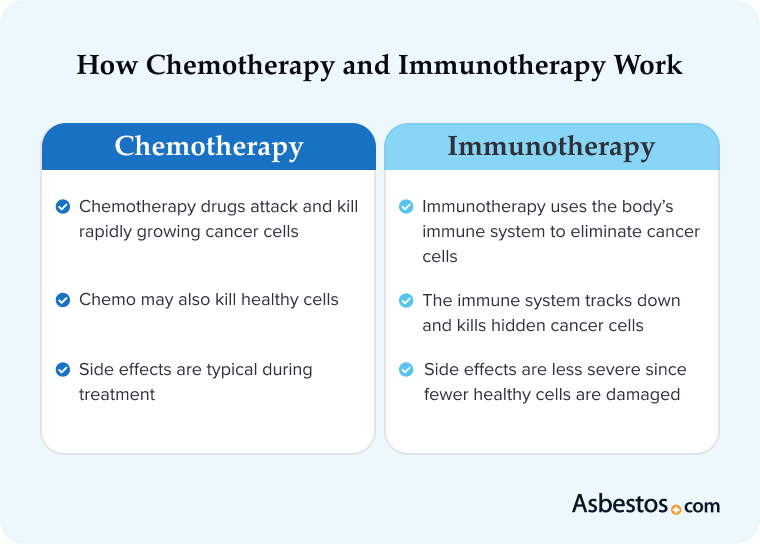
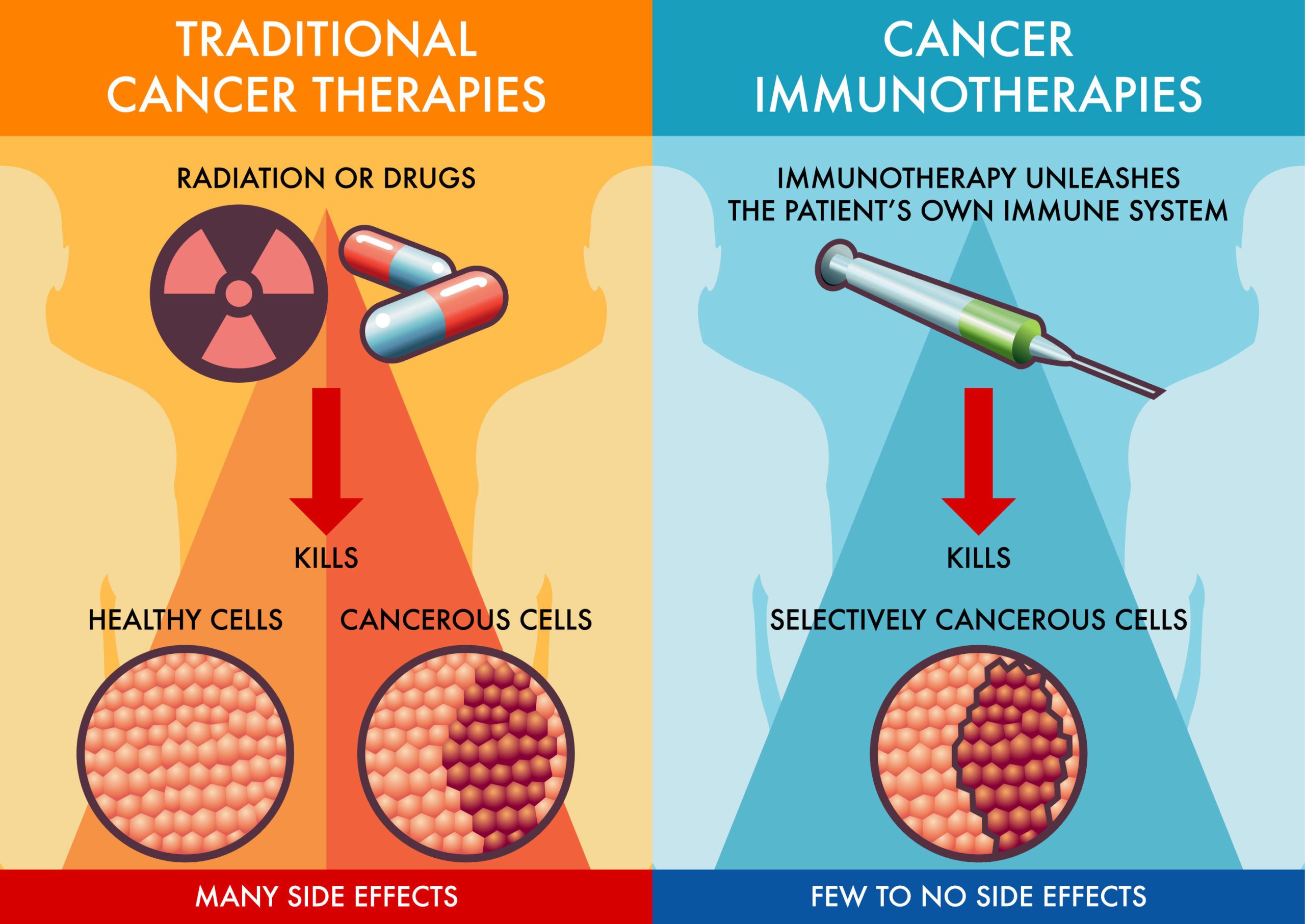
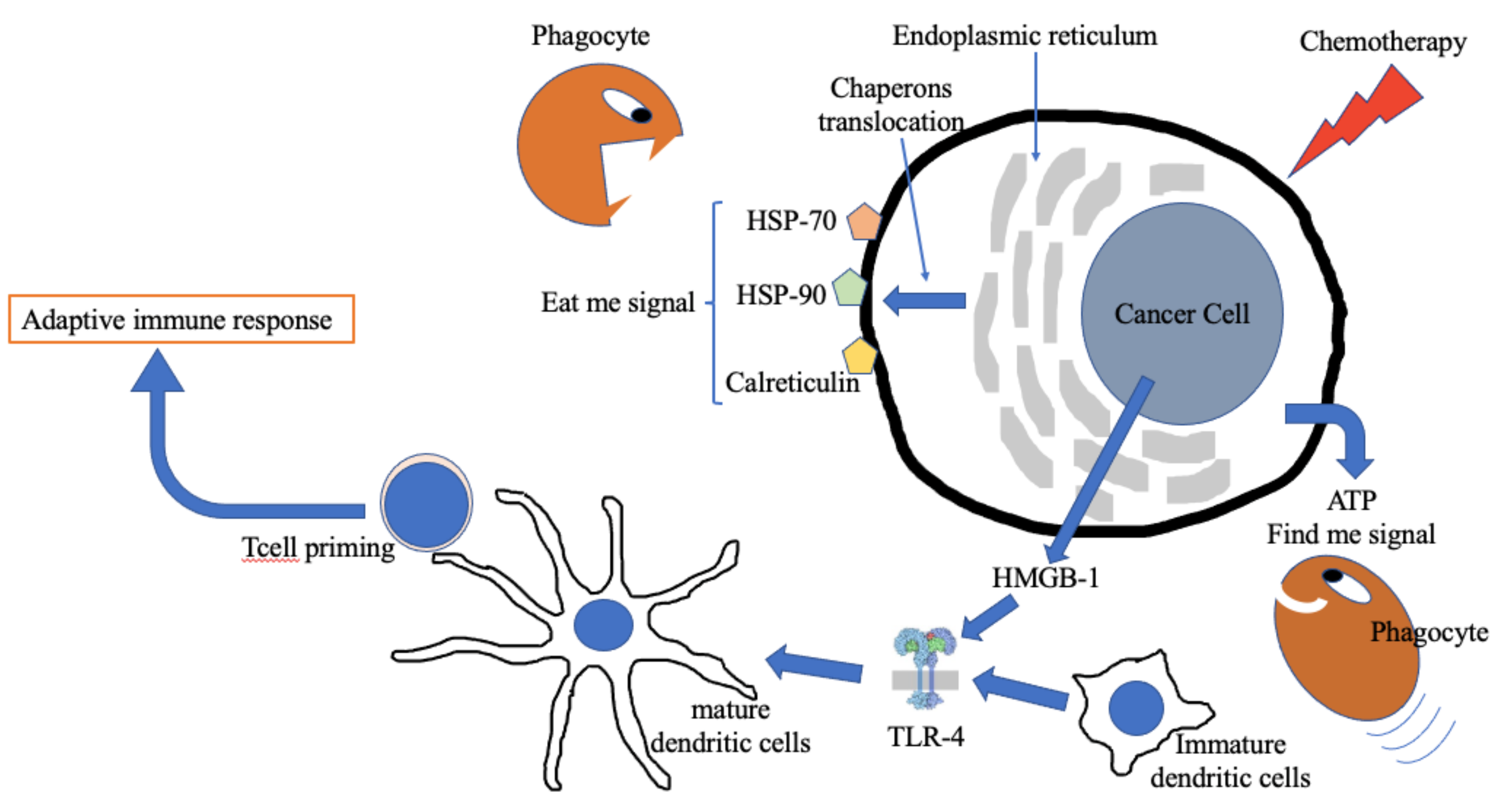
Chemotherapy, a powerful cancer treatment, severely weakens the immune system, leaving patients vulnerable to infections. Understanding the timeline of immune recovery post-chemo is critical for patient safety and management.
This article details the duration of immune system compromise following chemotherapy, highlighting factors influencing recovery time and crucial steps for minimizing infection risk.
The Critical Window: When Is Immunity Lowest?
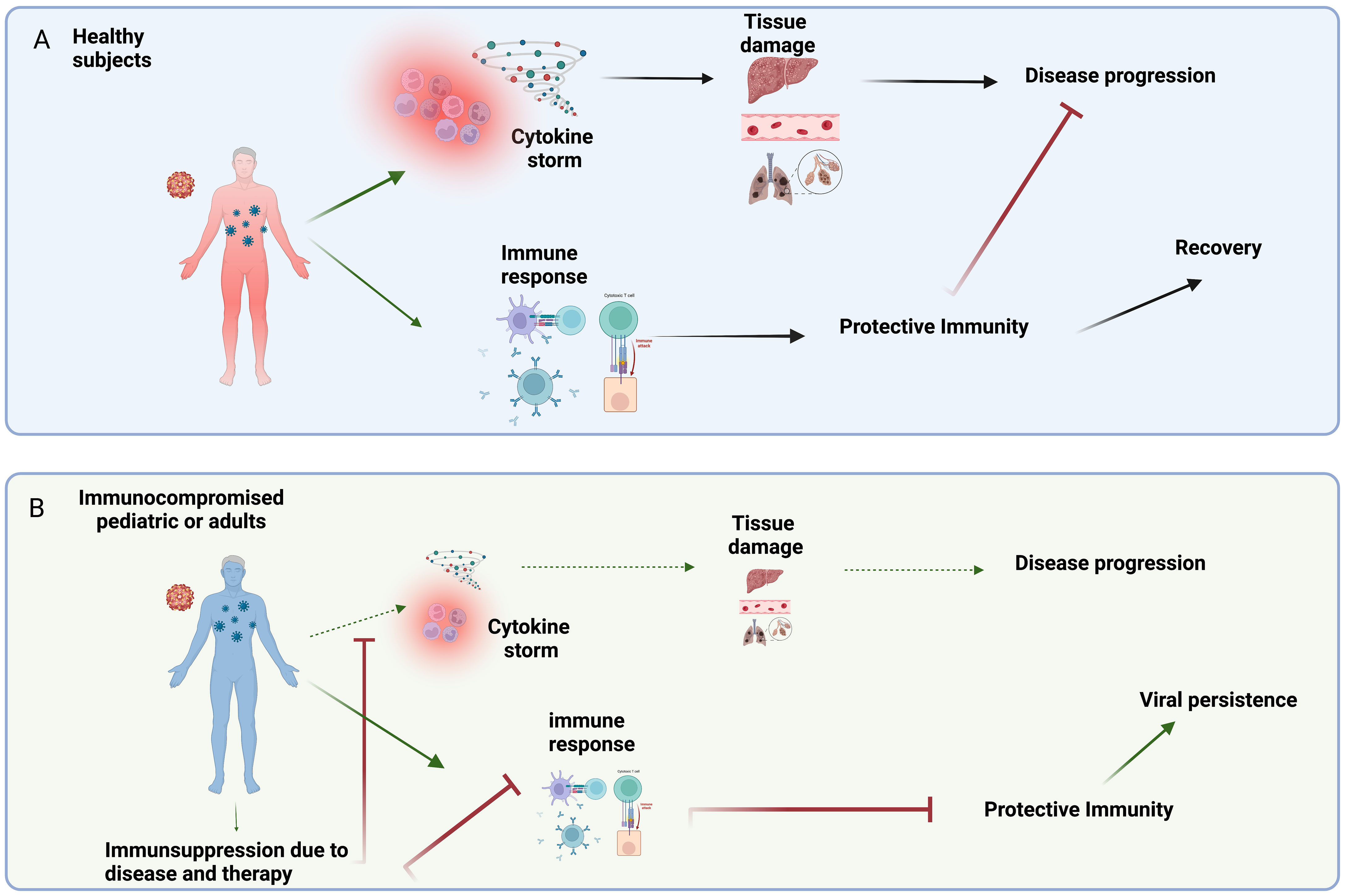
The period of greatest immune suppression typically occurs 7-14 days after chemotherapy administration. This nadir represents the point where white blood cell counts, particularly neutrophils, are at their lowest.
Neutropenia, a deficiency of neutrophils, is the primary driver of increased infection risk. The severity and duration of neutropenia directly correlate with the likelihood of developing serious infections.
According to the National Cancer Institute, patients experiencing febrile neutropenia (fever with low neutrophil count) require immediate medical attention.
How Long Does Immune Suppression Last?
Immune system recovery is not immediate and varies widely. For most patients, neutrophil counts begin to rebound within 3-4 weeks after chemotherapy.
However, full immune reconstitution, involving the restoration of all immune cell types and functions, can take significantly longer, ranging from several months to over a year.
Studies published in the journal "Blood" have shown that the recovery of T-cell function, crucial for long-term immunity, can be particularly delayed.
Factors Influencing Immune Recovery Time
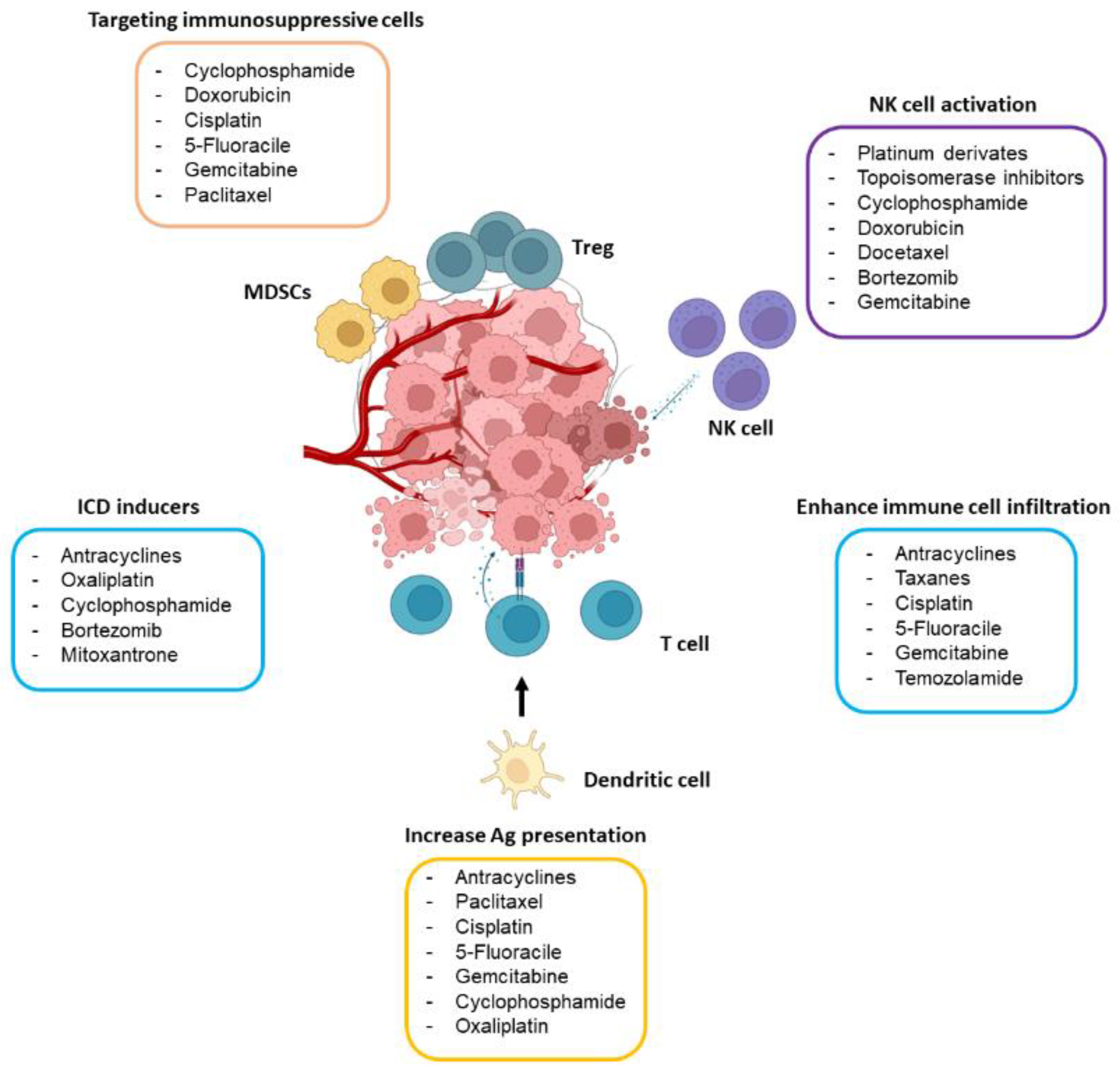
Several factors influence the duration of immune suppression post-chemo. The type of chemotherapy regimen used plays a significant role.
More aggressive and myelosuppressive regimens, which heavily impact bone marrow function, lead to more prolonged immune suppression.
Patient-specific factors, such as age, nutritional status, and pre-existing conditions, also contribute to recovery time. Older patients and those with comorbidities may experience slower immune reconstitution.
Prior radiation therapy or stem cell transplantation can further delay immune recovery. These treatments also impact the bone marrow's ability to produce new immune cells.
Minimizing Infection Risk During Immune Suppression
Protecting against infection is paramount during the period of immune compromise. Patients are advised to practice meticulous hygiene, including frequent handwashing.
Avoiding crowds and contact with sick individuals is crucial. Wearing a mask in public settings may offer additional protection.
The Centers for Disease Control and Prevention (CDC) recommends that patients receive vaccinations, such as influenza and pneumococcal vaccines, once their immune system has recovered sufficiently.
Prophylactic antibiotics or antiviral medications may be prescribed to prevent specific infections. These are generally reserved for patients at highest risk.
It is also important to avoid live vaccines during treatment and for at least six months after completion, or as directed by the oncologist.
Monitoring and Intervention
Regular blood tests are essential for monitoring white blood cell counts. These tests help identify neutropenia and guide treatment decisions.
Growth factors, such as granulocyte colony-stimulating factor (G-CSF), can stimulate neutrophil production and shorten the duration of neutropenia.
If an infection occurs, prompt treatment with antibiotics or other appropriate medications is critical. Delaying treatment can lead to severe complications.
Long-Term Considerations
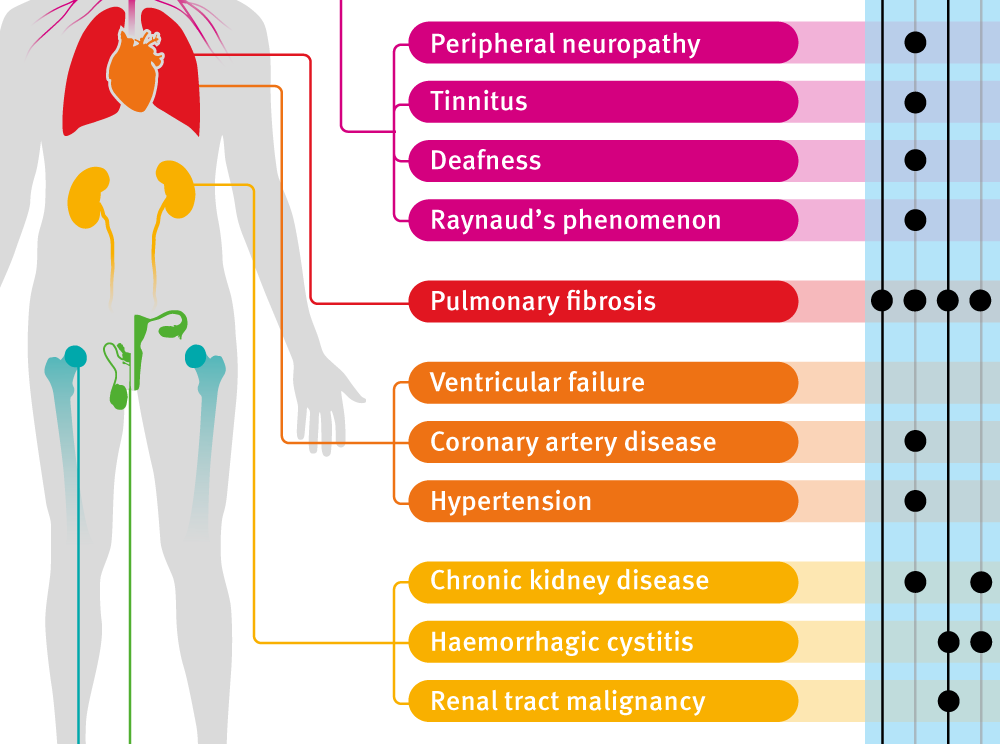
Even after immune cell counts normalize, some immune deficits may persist. Patients may be at increased risk for certain infections or have a blunted response to vaccinations.
Ongoing monitoring and individualized management strategies are essential. Staying in close communication with the oncology team is critical.
Research is ongoing to develop strategies to accelerate immune reconstitution and improve long-term immune function after chemotherapy. New therapies are being investigated to enhance T-cell recovery and improve vaccine responses.
Next Steps and Ongoing Developments
Patients should discuss their individual risk factors and immune recovery timeline with their oncologist. Adhering to recommended infection prevention strategies is paramount.
Continued research focuses on developing targeted therapies to improve immune function after chemotherapy. The goal is to minimize the risk of infection and improve long-term outcomes for cancer survivors.
For further information, consult reputable sources such as the American Cancer Society and the National Comprehensive Cancer Network (NCCN). These organizations offer valuable resources and guidelines for patients undergoing chemotherapy.



:max_bytes(150000):strip_icc()/can-cancer-spread-during-chemotherapy-5210592-FINAL-56da0fe9e94d4ae59539cac0e1014723.jpg)