How Much Do Biologics Suppress The Immune System
Imagine your immune system as a diligent, if sometimes overzealous, security guard protecting your body's castle. It's constantly on patrol, identifying and neutralizing threats like bacteria, viruses, and even rogue cells. But what happens when this guard becomes overly aggressive, attacking the castle itself? This is the reality for those with autoimmune diseases, and for many, biologics have become a vital tool to restore peace within the kingdom.
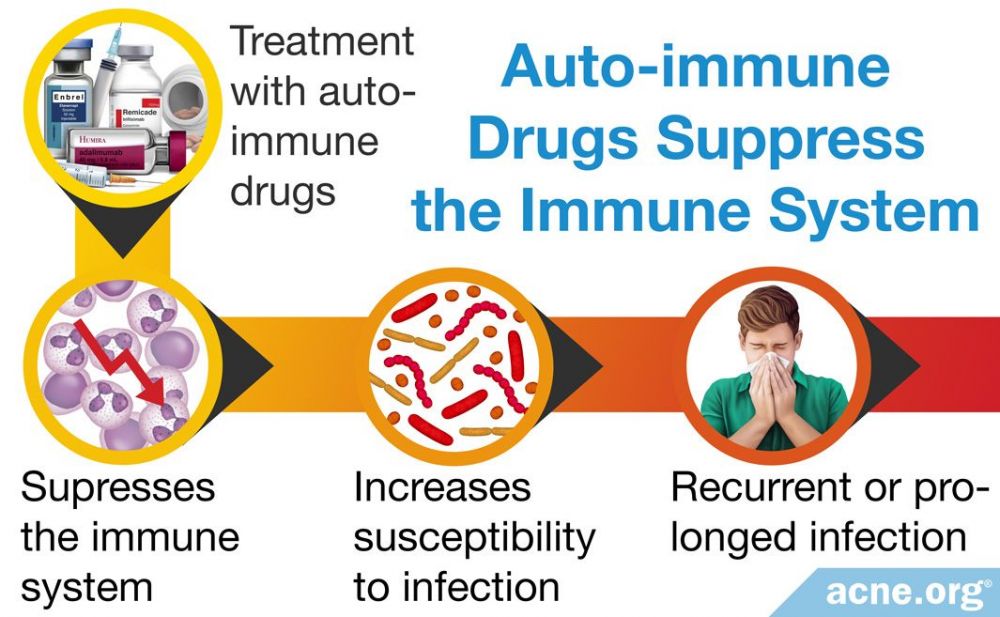
But how much do these powerful drugs, designed to modulate the immune system, actually suppress it? This is a critical question for patients and doctors alike, as the answer directly impacts the delicate balance between managing disease and maintaining overall health. Understanding the nuances of biologic-induced immunosuppression is key to navigating treatment effectively and minimizing potential risks.
The Rise of Biologics: A Targeted Approach
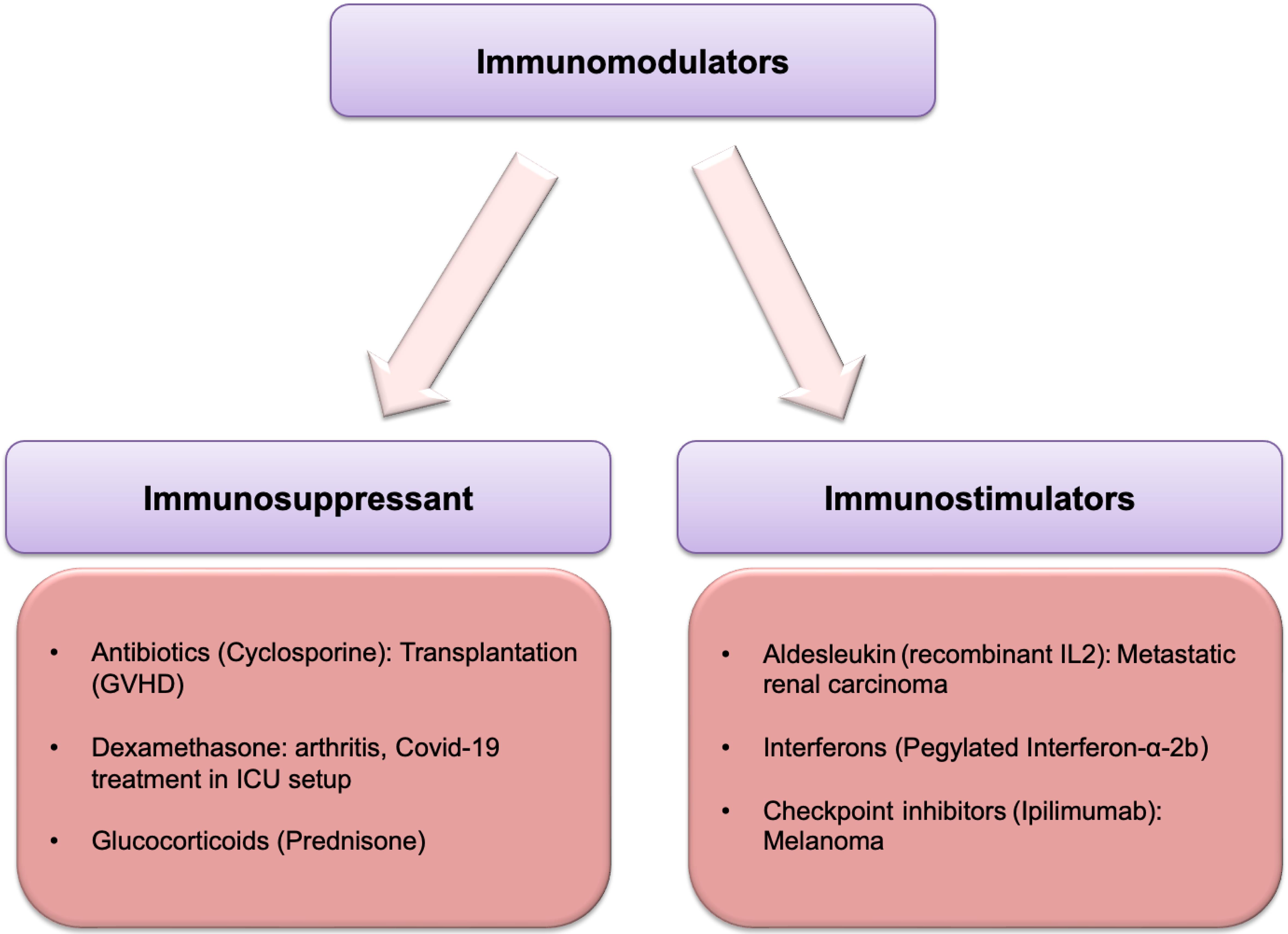
Biologics represent a significant advancement in the treatment of autoimmune and inflammatory conditions. Unlike traditional immunosuppressants that broadly dampen the entire immune system, biologics are designed to target specific components of the immune response.
This targeted approach offers the potential for greater efficacy and fewer side effects. They are often genetically engineered proteins derived from living cells.
This allows them to interact with the immune system in very specific ways, blocking certain inflammatory molecules or inhibiting the activity of specific immune cells.
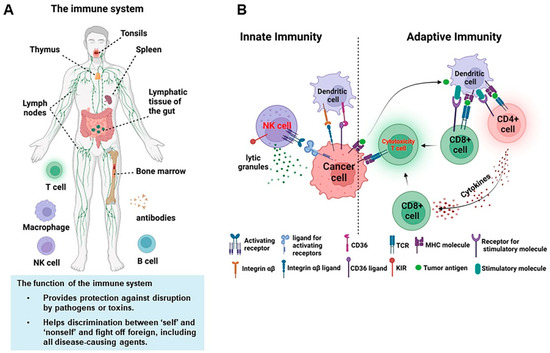
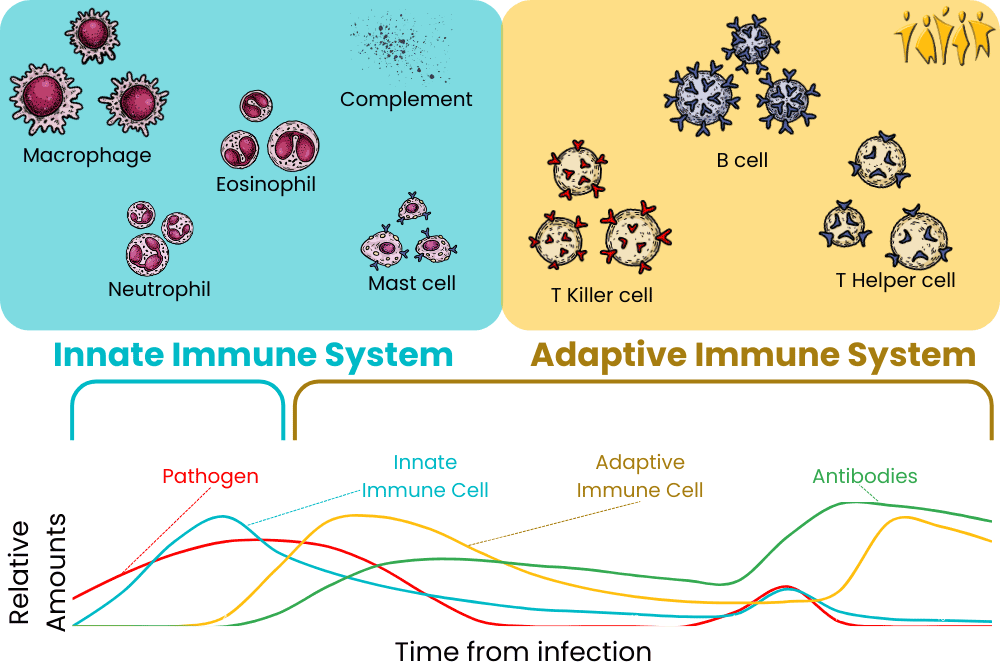
Understanding the Immune System
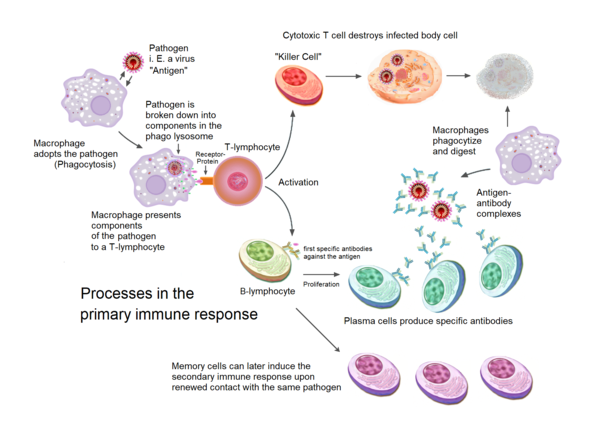
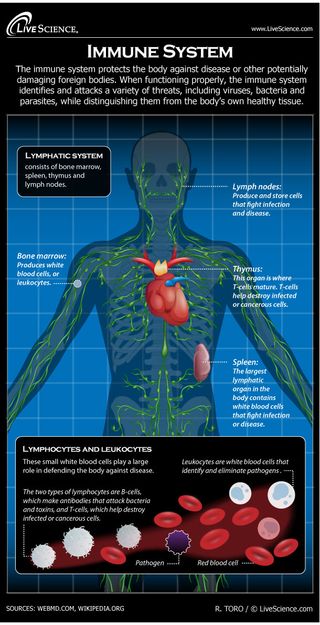
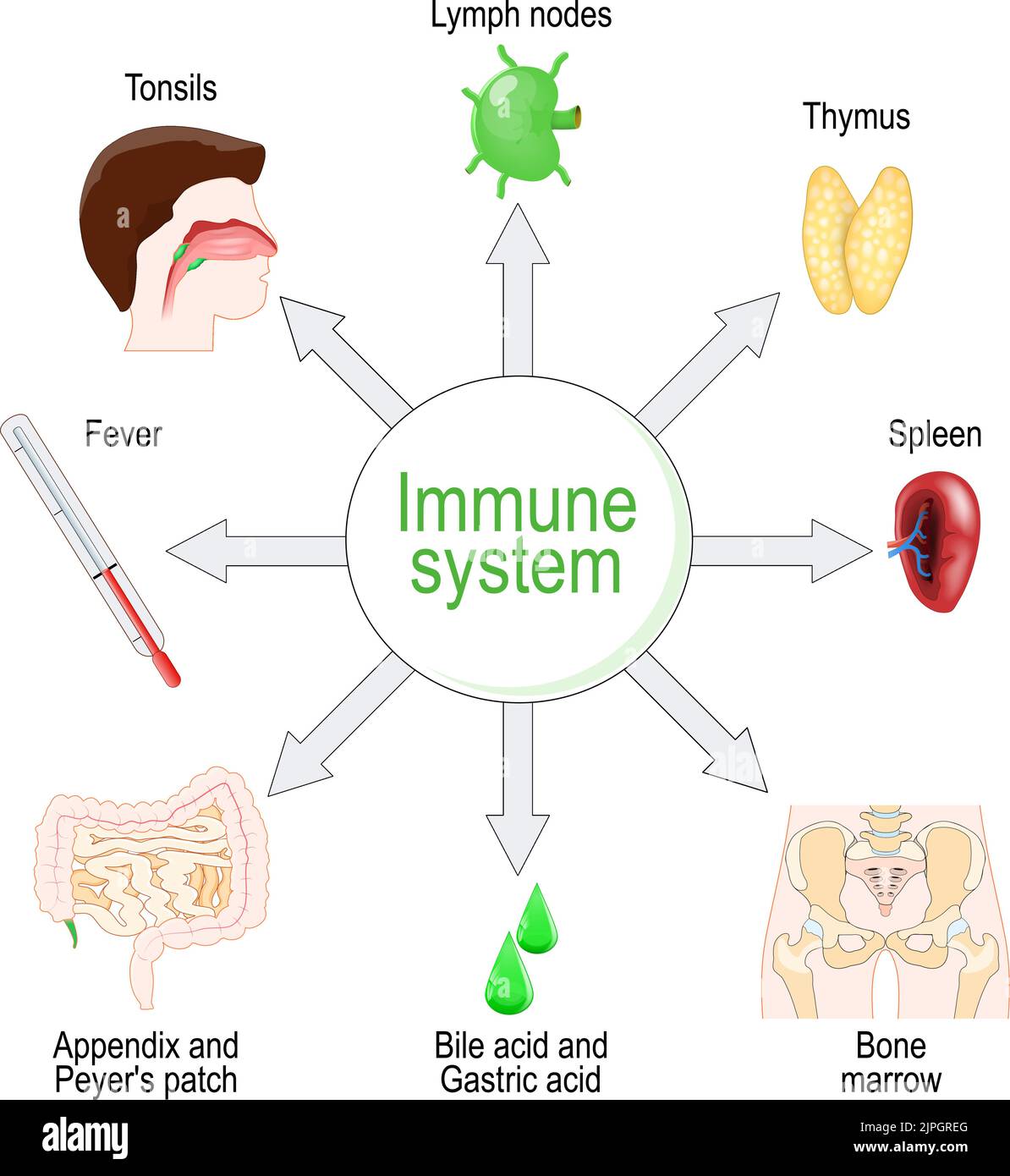
To appreciate how biologics work, it's crucial to understand the basics of the immune system. It's a complex network of cells, tissues, and organs that work together to defend the body against invaders.
Key players include T cells, B cells, and cytokines, which are signaling molecules that help regulate the immune response. In autoimmune diseases, this system malfunctions, leading to chronic inflammation and tissue damage.
Diseases like rheumatoid arthritis, Crohn's disease, psoriasis, and multiple sclerosis are all examples of conditions where the immune system mistakenly attacks the body's own tissues.
How Biologics Suppress the Immune System: Mechanisms of Action
Biologics work by interfering with specific pathways involved in the inflammatory process. One common class of biologics, TNF inhibitors, blocks the action of tumor necrosis factor (TNF), a cytokine that plays a central role in inflammation.
By neutralizing TNF, these drugs can significantly reduce inflammation and alleviate symptoms in conditions like rheumatoid arthritis and Crohn's disease. Other biologics target different cytokines, such as interleukin-17 (IL-17) or interleukin-6 (IL-6), or they may target specific immune cells, such as B cells.
For example, rituximab, a biologic used to treat rheumatoid arthritis and other autoimmune diseases, works by depleting B cells, which are responsible for producing antibodies that contribute to inflammation.
"The beauty of biologics is their precision," explains Dr. Anya Sharma, a rheumatologist at the Mayo Clinic. "They allow us to target specific aspects of the immune system that are driving the disease, rather than simply suppressing the entire system indiscriminately."
The Degree of Immunosuppression: A Balancing Act
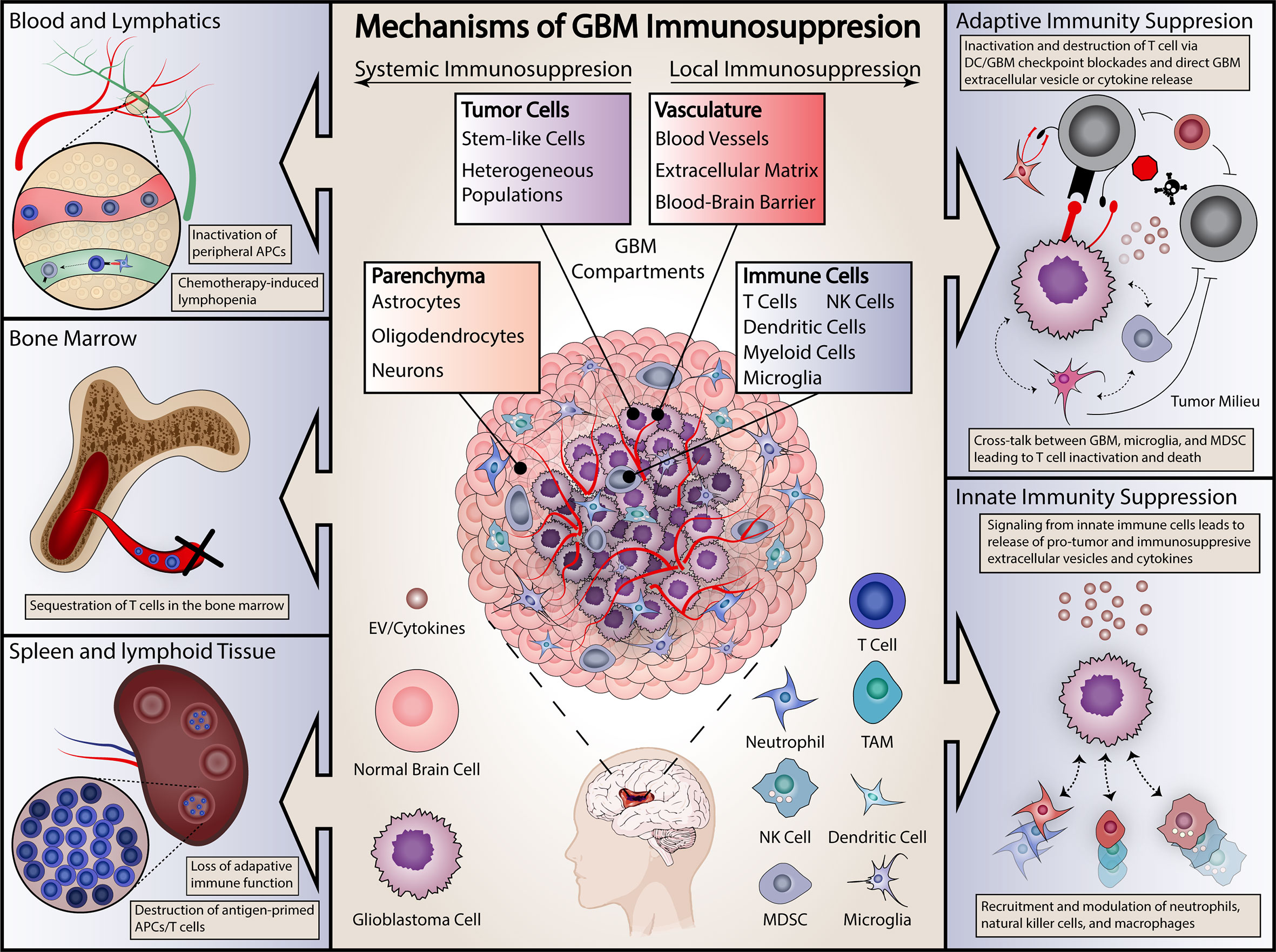
While biologics are more targeted than traditional immunosuppressants, they still carry a risk of suppressing the immune system to some extent. The degree of immunosuppression varies depending on the specific biologic, the dosage, and the individual patient.
Some biologics, like TNF inhibitors, are generally considered to be less immunosuppressive than others, such as rituximab, which depletes B cells. Patients taking biologics are generally at a slightly increased risk of infections, particularly respiratory infections like pneumonia and influenza.
They may also be at a higher risk of opportunistic infections, which are infections caused by organisms that typically don't cause disease in people with healthy immune systems. Some studies have also suggested a slightly increased risk of certain types of cancer in patients taking biologics, although this risk is still being investigated.
The risk of infection or other complications needs to be carefully weighed against the benefits of controlling the underlying autoimmune disease. Doctors carefully monitor patients taking biologics for signs of infection and take steps to minimize the risk, such as recommending vaccinations and practicing good hygiene.
Factors Influencing Immunosuppression
Several factors can influence the degree of immunosuppression associated with biologics. These include the specific biologic being used, the dosage, the duration of treatment, and the patient's overall health.
Patients with other underlying medical conditions, such as diabetes or chronic lung disease, may be at a higher risk of infection while taking biologics. Concomitant use of other immunosuppressants, such as corticosteroids, can also increase the risk of immunosuppression.
Older adults are generally more susceptible to infections and may experience a greater degree of immunosuppression from biologics compared to younger patients.
Minimizing the Risks: Monitoring and Prevention
Careful monitoring is essential to minimize the risks associated with biologic-induced immunosuppression. Doctors typically perform regular blood tests to monitor immune cell counts and assess liver and kidney function.
Patients are also advised to report any signs of infection, such as fever, cough, or sore throat, to their doctor promptly. Vaccinations are an important part of preventing infections in patients taking biologics, but it's important to note that live vaccines are generally contraindicated.
"We strongly encourage our patients to get vaccinated against influenza and pneumonia before starting biologic therapy," says Dr. David Lee, an infectious disease specialist at UCSF. "This can significantly reduce their risk of developing serious infections."
Practicing good hygiene, such as washing hands frequently and avoiding close contact with sick people, can also help prevent infections.
"The key is to find the right balance between controlling the disease and minimizing the risks of immunosuppression," emphasizes Dr. Sharma.
The Future of Biologics: Personalized Medicine
The field of biologics is constantly evolving, with new drugs and new approaches being developed all the time. One promising area of research is personalized medicine, which aims to tailor treatment to the individual patient based on their genetic makeup and other factors.
By identifying biomarkers that predict response to specific biologics, doctors may be able to select the most effective treatment for each patient while minimizing the risk of side effects. Researchers are also exploring new ways to deliver biologics, such as through subcutaneous injections or oral formulations, which could improve patient convenience and adherence.
Furthermore, scientists are working on developing biologics with even greater specificity and fewer off-target effects, further reducing the risk of immunosuppression.
Living Well with Biologics: A Patient's Perspective
For many people living with autoimmune diseases, biologics have been life-changing. They have enabled them to regain control of their lives, reduce pain and inflammation, and participate more fully in activities they enjoy.
However, it's important to remember that biologics are not a cure and that they do carry risks. Patients need to be actively involved in their care, working closely with their doctors to monitor their condition and manage any side effects.
By staying informed, following their doctor's recommendations, and practicing good self-care, people taking biologics can live full and active lives.
In the end, understanding how much biologics suppress the immune system is not about fear, but about empowerment. It's about equipping patients and healthcare providers with the knowledge to make informed decisions, to navigate the complexities of treatment, and to ultimately, live healthier, more fulfilling lives. The diligent security guard, while needing a little recalibration, is still there, working to protect the castle, thanks to the carefully calibrated intervention of modern medicine.