Left Ventricular Diastolic Dysfunction Icd 10

A surge in diagnoses of Left Ventricular Diastolic Dysfunction (LVDD) is overwhelming healthcare systems nationwide, prompting urgent calls for revised diagnostic protocols and increased resource allocation.
The dramatic increase in LVDD diagnoses, coded under ICD-10, is straining resources and raising concerns about diagnostic accuracy and the effectiveness of current treatment strategies.
The Alarming Increase
Data released this week by the Centers for Disease Control and Prevention (CDC) indicates a 30% increase in LVDD diagnoses over the past year, with the sharpest rises observed in patients over 65.
States like Florida, California, and Texas are reporting the highest incidence rates, placing significant pressure on their respective healthcare infrastructures.
This sudden spike is prompting investigations into potential contributing factors, including environmental influences and evolving diagnostic practices.
Decoding ICD-10 for LVDD
The ICD-10 code I50.3 is primarily used to classify diastolic (restrictive) heart failure, and thus is frequently used to diagnose LVDD.
However, some medical professionals believe the broad application of this code might be contributing to overdiagnosis.
“The criteria for diagnosing LVDD can be subjective, leading to inconsistencies in coding and potentially inflating the numbers,” explains Dr. Emily Carter, a leading cardiologist at the American Heart Association.
Who is Affected?
While LVDD can affect individuals of any age, the elderly population is disproportionately impacted.
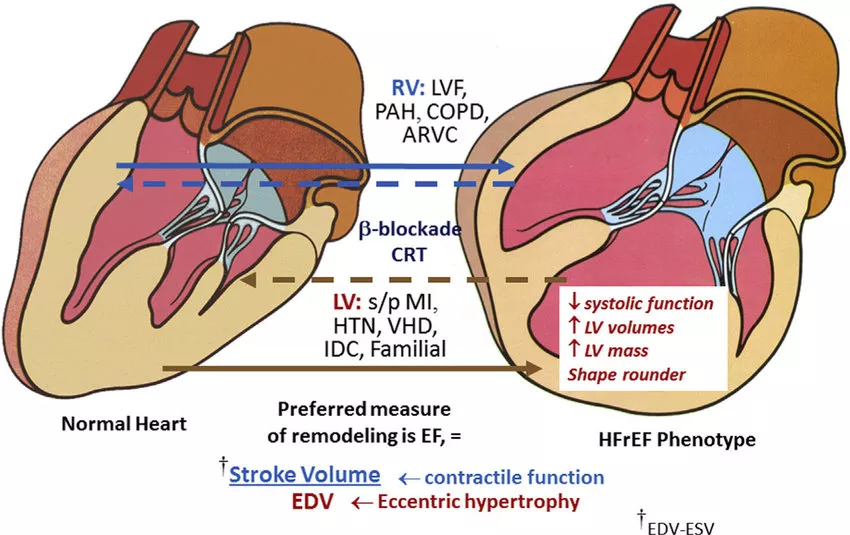
Individuals with pre-existing conditions such as hypertension, diabetes, and coronary artery disease are also at heightened risk.
Early symptoms often include shortness of breath, fatigue, and swelling in the ankles and feet.
Where is the Problem Most Acute?
Major metropolitan areas with large aging populations are experiencing the most significant strain.
Hospitals in Miami, Los Angeles, and Houston are reporting longer wait times for diagnostic testing and treatment of LVDD.
Rural communities are also struggling to cope due to limited access to specialized cardiology services.
When Did This Surge Begin?
The significant increase in LVDD diagnoses became noticeable in the last fiscal year, starting around Q3.
Experts are analyzing data to determine if the surge correlates with any specific events, such as changes in environmental conditions or public health initiatives.
Preliminary findings suggest a potential link to long-term effects of previous respiratory infections, but more research is needed.
How is LVDD Diagnosed?
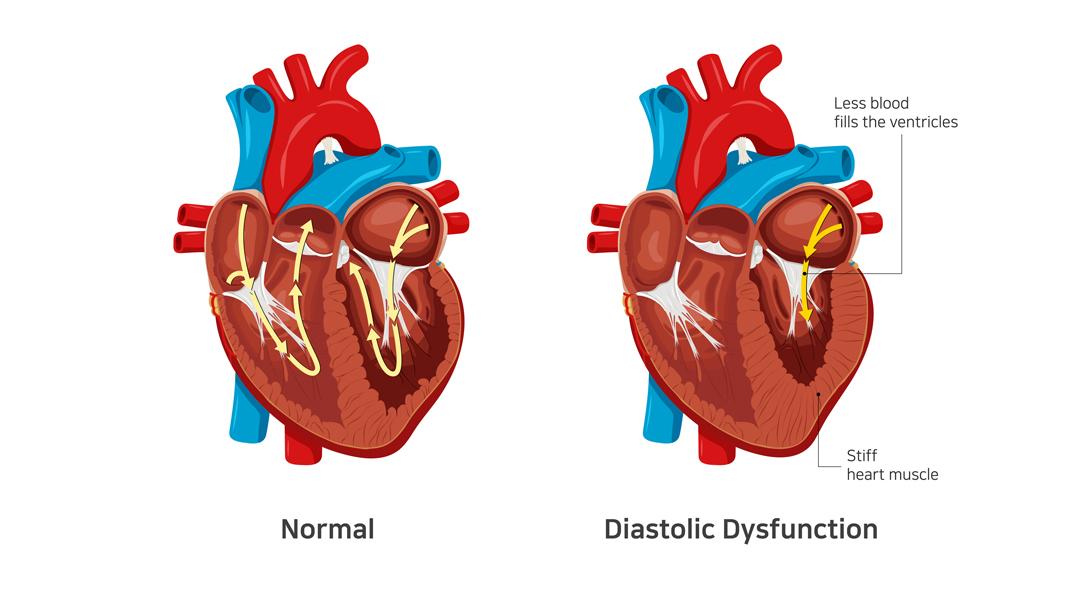
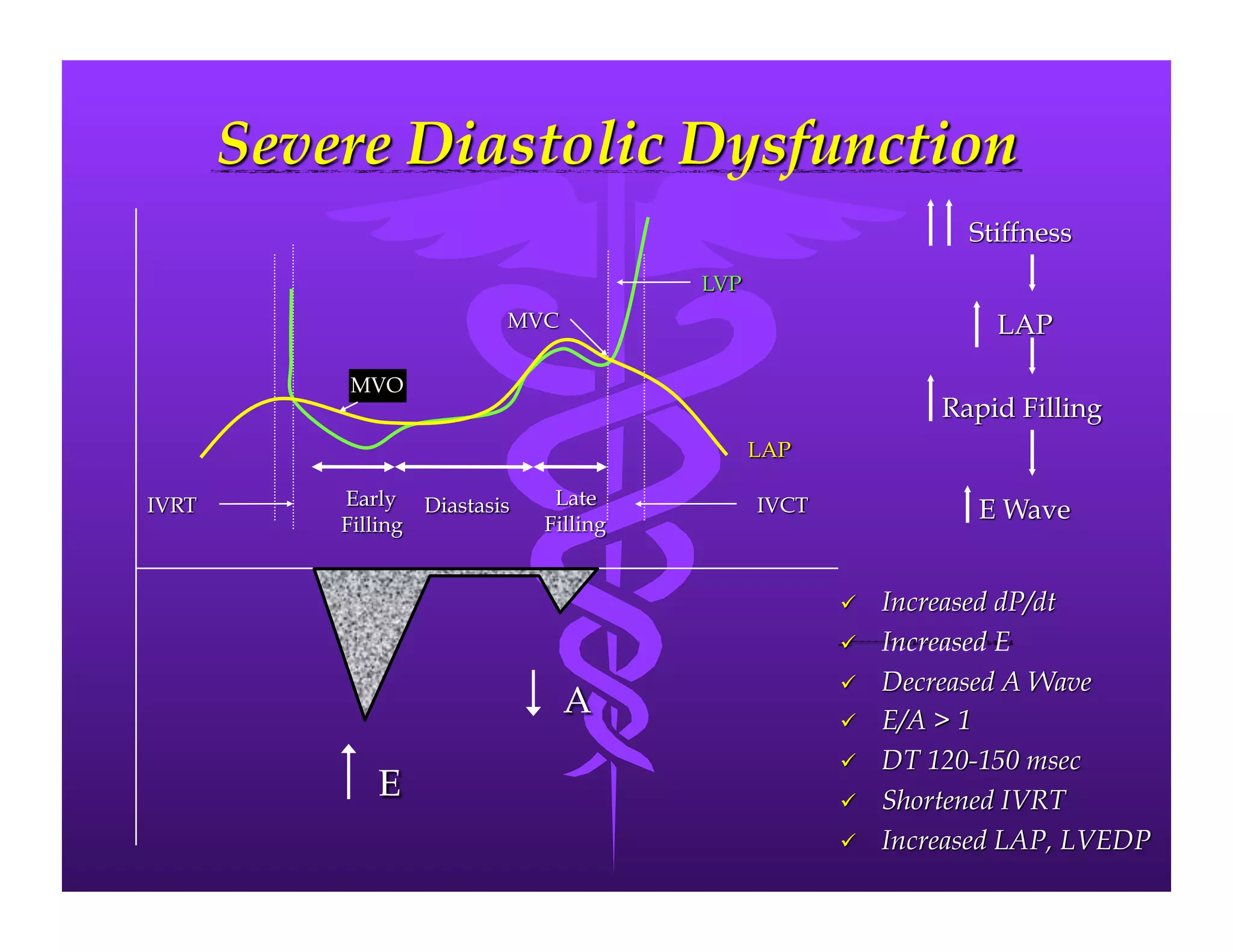
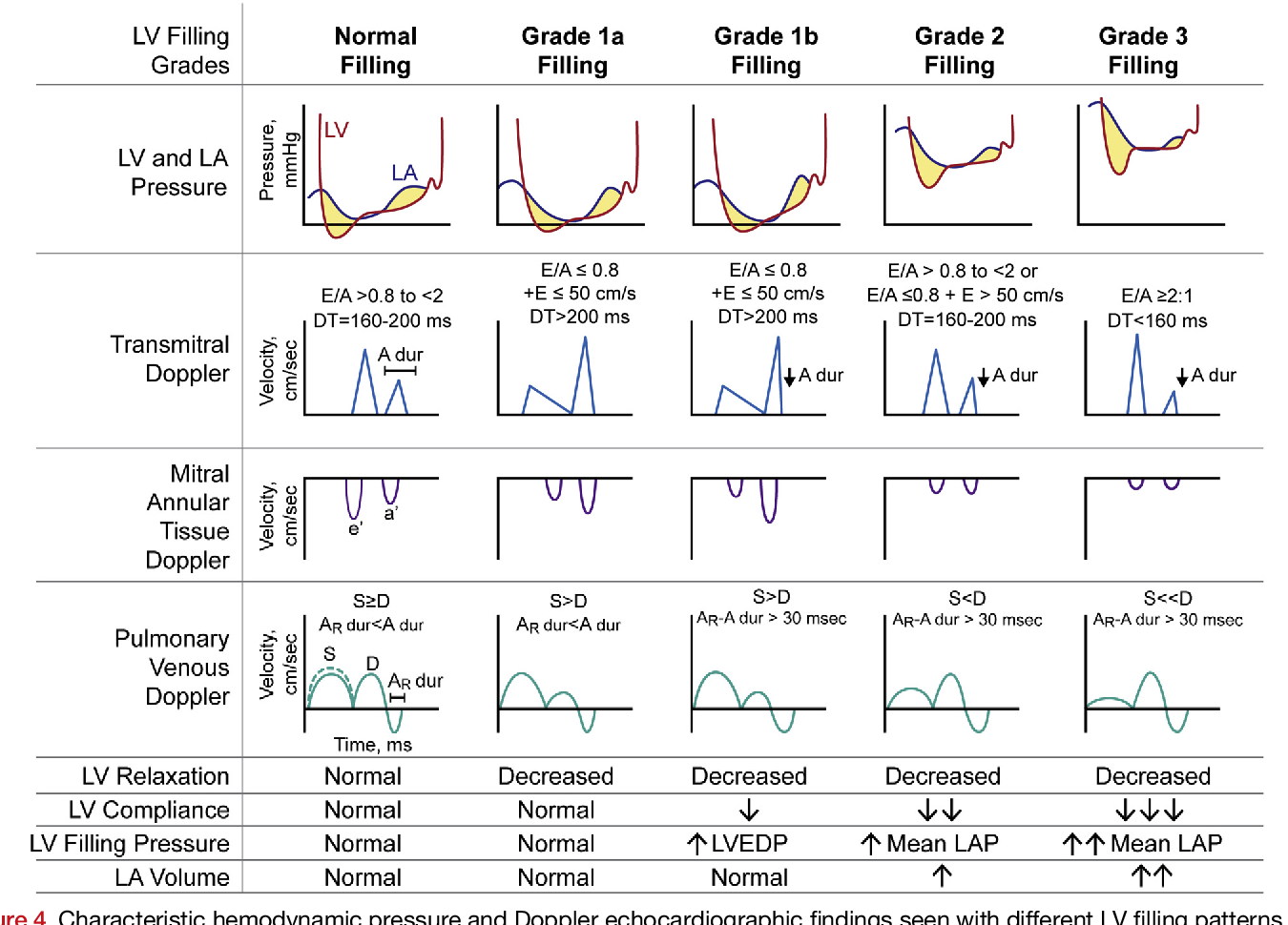
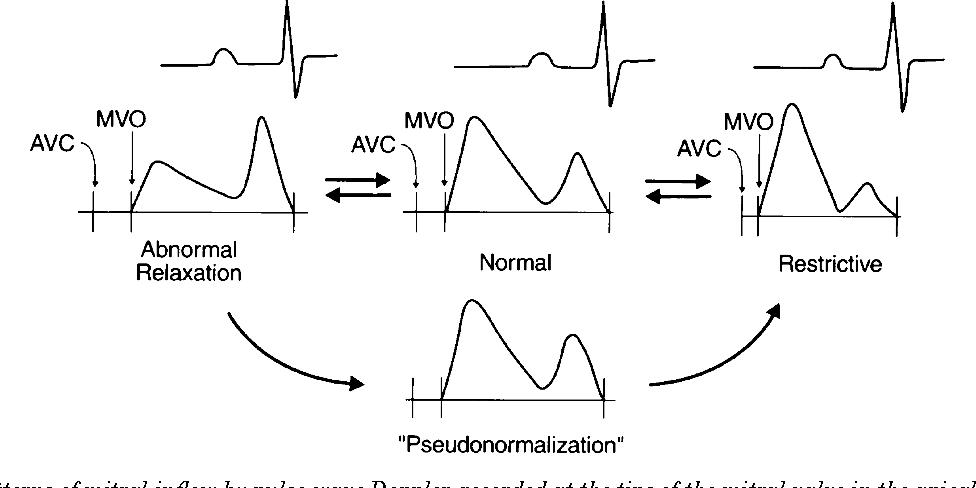
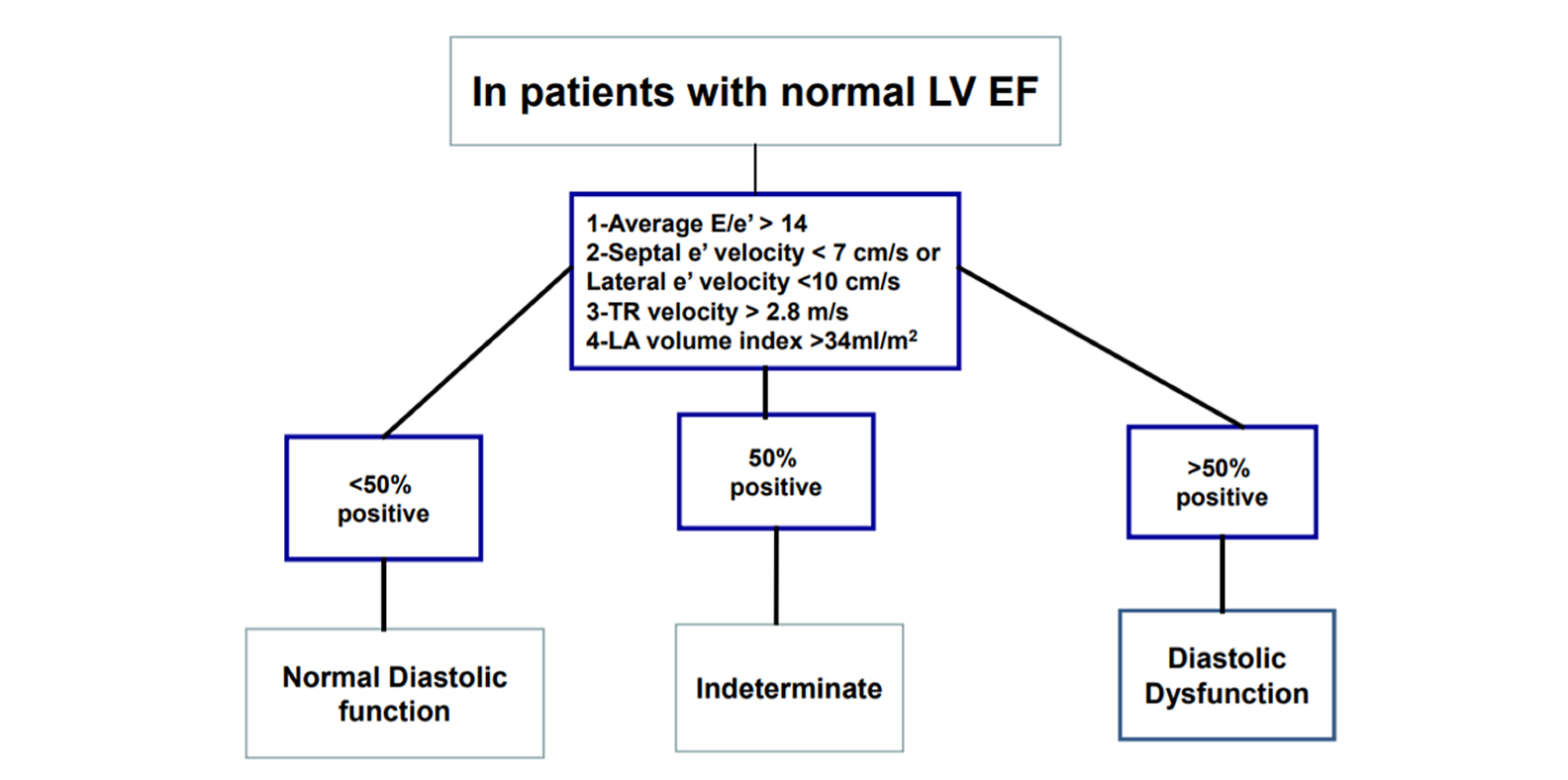
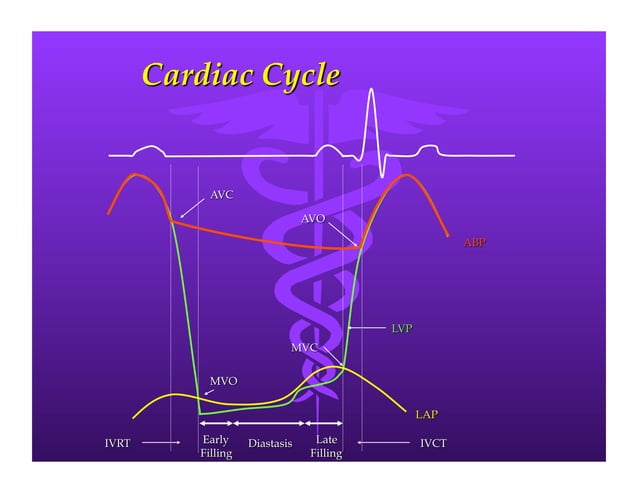
Echocardiography is the primary diagnostic tool used to assess left ventricular diastolic function.
This non-invasive imaging technique allows doctors to visualize the heart and measure its ability to relax and fill with blood.
However, interpreting echocardiogram results can be challenging, leading to variability in diagnoses.
The Impact on Healthcare Systems
The increased number of LVDD diagnoses is putting a strain on hospital resources, including diagnostic equipment and cardiology specialists.
Longer wait times for echocardiograms and consultations are becoming increasingly common.
This situation is also impacting the cost of healthcare, as more patients require ongoing monitoring and treatment.
Challenges in Treatment
There is no specific cure for LVDD, and treatment focuses on managing symptoms and addressing underlying conditions.
Medications such as diuretics, ACE inhibitors, and beta-blockers are commonly prescribed to control blood pressure and reduce fluid retention.
Lifestyle modifications, including diet and exercise, also play a crucial role in managing the condition.
Calls for Action
Healthcare professionals and policymakers are urging for immediate action to address the LVDD crisis.
Recommendations include developing standardized diagnostic criteria, increasing funding for research, and improving access to specialized cardiology services.
“We need a coordinated effort to ensure that patients with LVDD receive timely and appropriate care,” emphasizes Dr. Carter.
Next Steps and Ongoing Developments
The CDC is currently conducting a comprehensive review of LVDD diagnostic practices and coding guidelines.
A task force comprised of leading cardiologists and healthcare experts has been formed to develop updated recommendations for diagnosis and treatment.
The findings of this review are expected to be released in the coming months, potentially leading to significant changes in how LVDD is managed.
The surge in LVDD diagnoses demands a swift and coordinated response to mitigate its impact on healthcare systems and patient outcomes.
Ongoing research and revised guidelines are crucial for ensuring accurate diagnoses and effective management of this growing health concern.