Low Molecular Weight Heparin Vs Unfractionated

For decades, managing blood clots has relied on two primary types of heparin: unfractionated heparin (UFH) and low molecular weight heparin (LMWH). Both prevent blood from clotting, but recent data and evolving clinical practices are prompting re-evaluations of their respective roles in modern medicine.
This article examines the differences between UFH and LMWH, delving into their mechanisms, applications, benefits, and drawbacks. It will also explore how these factors influence clinical decision-making and patient outcomes in various medical scenarios. Understanding the nuances of these anticoagulants is critical for healthcare professionals and patients alike.
Understanding Heparin: The Basics
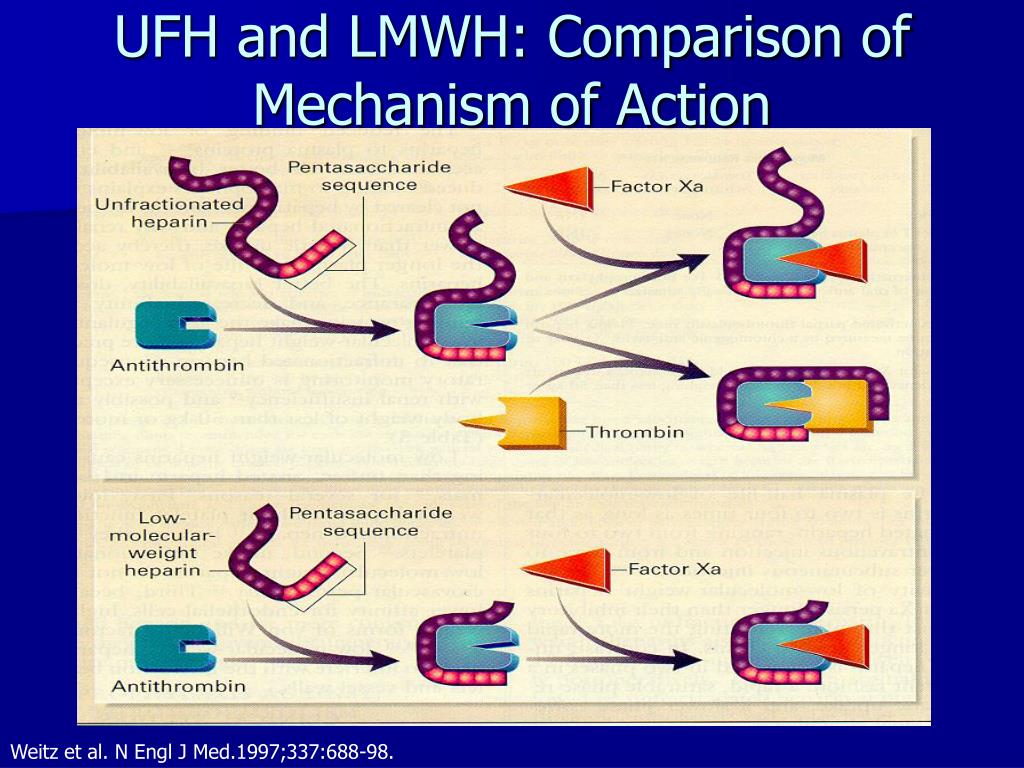
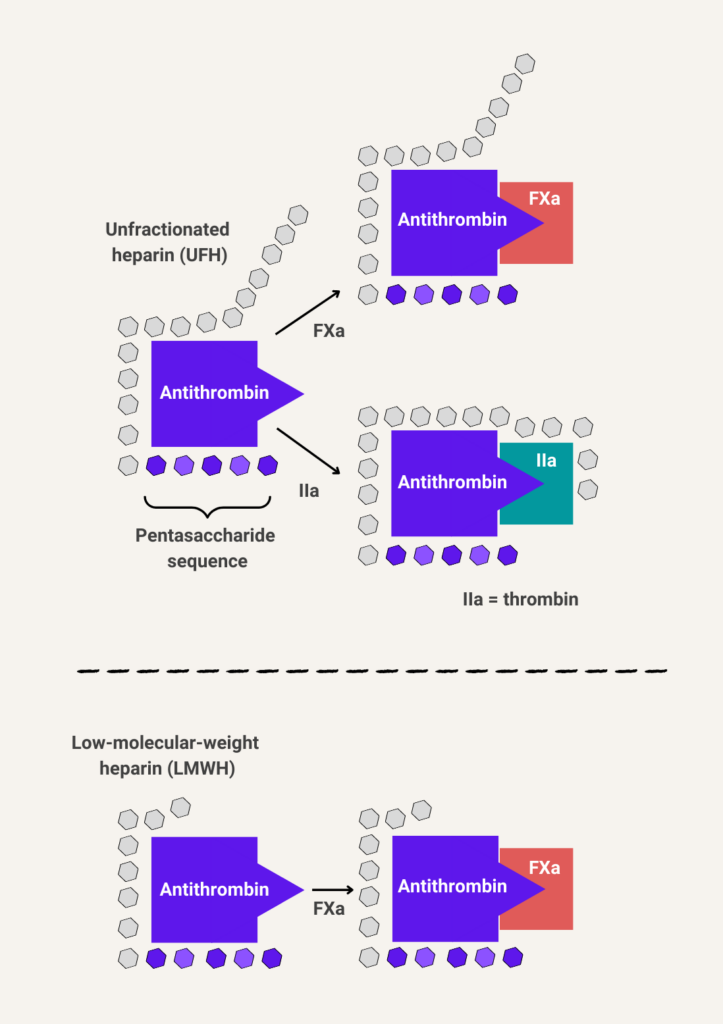
Heparin, in its various forms, works by inhibiting certain clotting factors in the blood. This prevents the formation of dangerous blood clots that can lead to serious health complications. Both UFH and LMWH achieve this by binding to antithrombin, a naturally occurring protein in the blood that inactivates clotting factors.
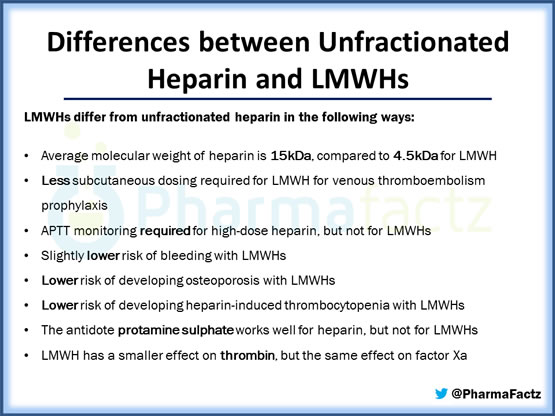
The key difference lies in their molecular structure. UFH is a mixture of heparin chains with varying lengths and molecular weights, while LMWH consists of shorter, more uniform chains.
UFH: The Established Anticoagulant
Unfractionated Heparin has been a cornerstone of anticoagulation therapy for many years. Its use is well-established in a variety of clinical settings, including the treatment of deep vein thrombosis (DVT), pulmonary embolism (PE), and during certain surgical procedures.
One significant advantage of UFH is its short half-life. This allows for rapid reversal of its effects if necessary, which is crucial in emergency situations or when bleeding complications arise. Protamine sulfate is the antidote used to reverse UFH's anticoagulant activity.
However, UFH also has some limitations. Its unpredictable anticoagulant response requires frequent monitoring of blood clotting parameters, such as the activated partial thromboplastin time (aPTT). This monitoring adds to the cost and complexity of treatment.
LMWH: A Modern Alternative
Low Molecular Weight Heparin offers several advantages over UFH. Its more predictable anticoagulant response allows for fixed-dose administration, eliminating the need for routine blood monitoring in many cases. This simplifies treatment and reduces the burden on both patients and healthcare providers.
LMWH also has a longer half-life than UFH. This permits once- or twice-daily subcutaneous injections, making it more convenient for outpatients. This is particularly beneficial for individuals receiving extended anticoagulation therapy.
Despite these advantages, LMWH is not without its drawbacks. Its effects are less easily reversed than those of UFH. Protamine sulfate is only partially effective in neutralizing LMWH's anticoagulant activity.
Key Differences Summarized
To summarize, UFH requires frequent lab monitoring, has a shorter half-life, and its effects are readily reversible with protamine. LMWH has a longer half-life, predictable response (less monitoring), but only partially reversible.
Specific Advantages of UFH:
Rapid reversibility allows for prompt intervention in case of bleeding.
Cost-effective in certain settings, particularly when intensive monitoring is already required.
Specific Advantages of LMWH:
Convenient outpatient administration reduces hospital stays.
Reduced need for lab monitoring frees up resources.
Lower risk of heparin-induced thrombocytopenia (HIT) in some studies.
Clinical Applications and Guidelines
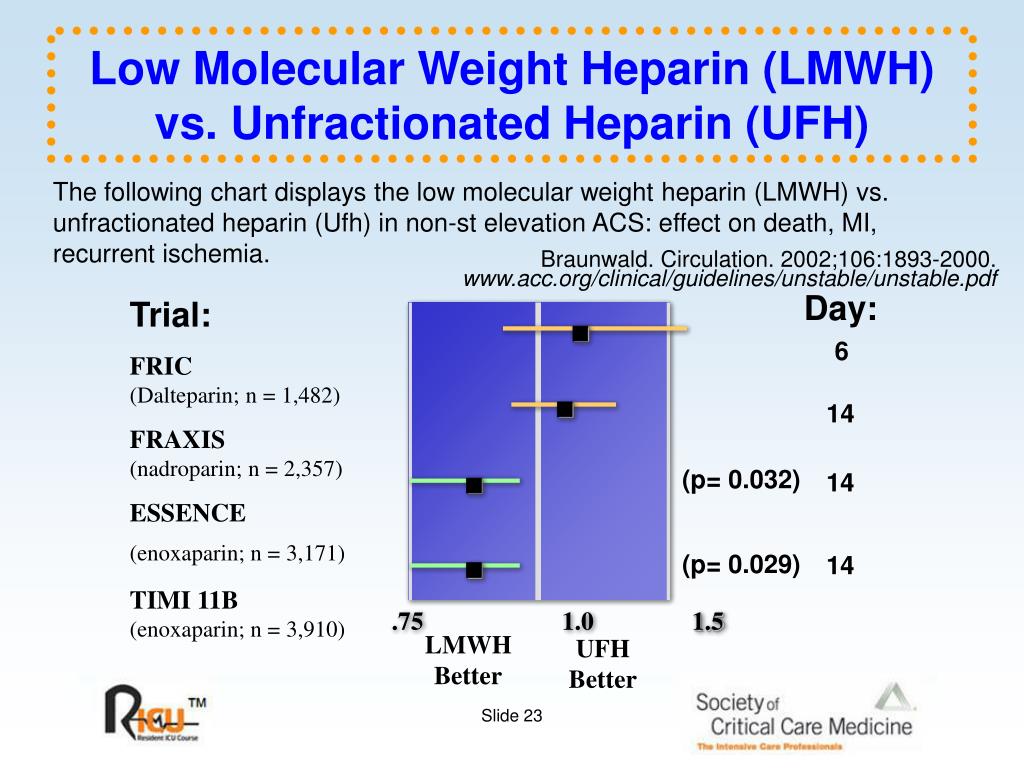
Both UFH and LMWH have established roles in various clinical scenarios. However, the choice between the two often depends on the specific clinical context, patient characteristics, and institutional preferences. Treatment guidelines from organizations like the American College of Chest Physicians (ACCP) and the American Heart Association (AHA) provide recommendations for the use of these anticoagulants.
For example, LMWH is often preferred for the initial treatment of DVT and PE in outpatient settings due to its convenience and ease of administration. UFH is often favored when rapid reversal is critical, such as in patients undergoing surgery or with a high risk of bleeding.
Recent guidelines also address the use of direct oral anticoagulants (DOACs), which offer an alternative to both UFH and LMWH in certain situations. DOACs are oral medications with predictable anticoagulant effects and do not typically require routine monitoring.
The Future of Heparin Therapy
While DOACs have gained increasing popularity, heparin remains an important anticoagulant option. Ongoing research is focused on further optimizing the use of UFH and LMWH, as well as developing new heparin-based therapies. This includes exploring novel reversal agents for LMWH and investigating the potential of modified heparins with improved safety profiles.
The landscape of anticoagulation therapy continues to evolve. Healthcare professionals must stay informed about the latest evidence and guidelines to provide the best possible care for their patients.
Human Angle: Patient Experience
Many patients have experienced the difference between the two medications. One such example is Sarah, a 62-year-old woman who developed a DVT after a hip replacement. Initially treated with UFH in the hospital, she transitioned to LMWH for continued anticoagulation at home.
Sarah found the LMWH injections much easier to manage than the frequent blood tests required with UFH. This improved her quality of life and allowed her to focus on her recovery. Her experience underscores the importance of considering patient preferences and convenience when choosing an anticoagulant.
Conclusion
Unfractionated heparin and low molecular weight heparin remain essential tools in the fight against blood clots. While LMWH has gained popularity due to its ease of use, UFH retains a critical role in situations requiring rapid reversibility. As medical science advances, understanding the specific advantages and disadvantages of each anticoagulant is crucial for informed clinical decision-making and improved patient outcomes.