Nursing Diagnosis For Peripheral Arterial Disease
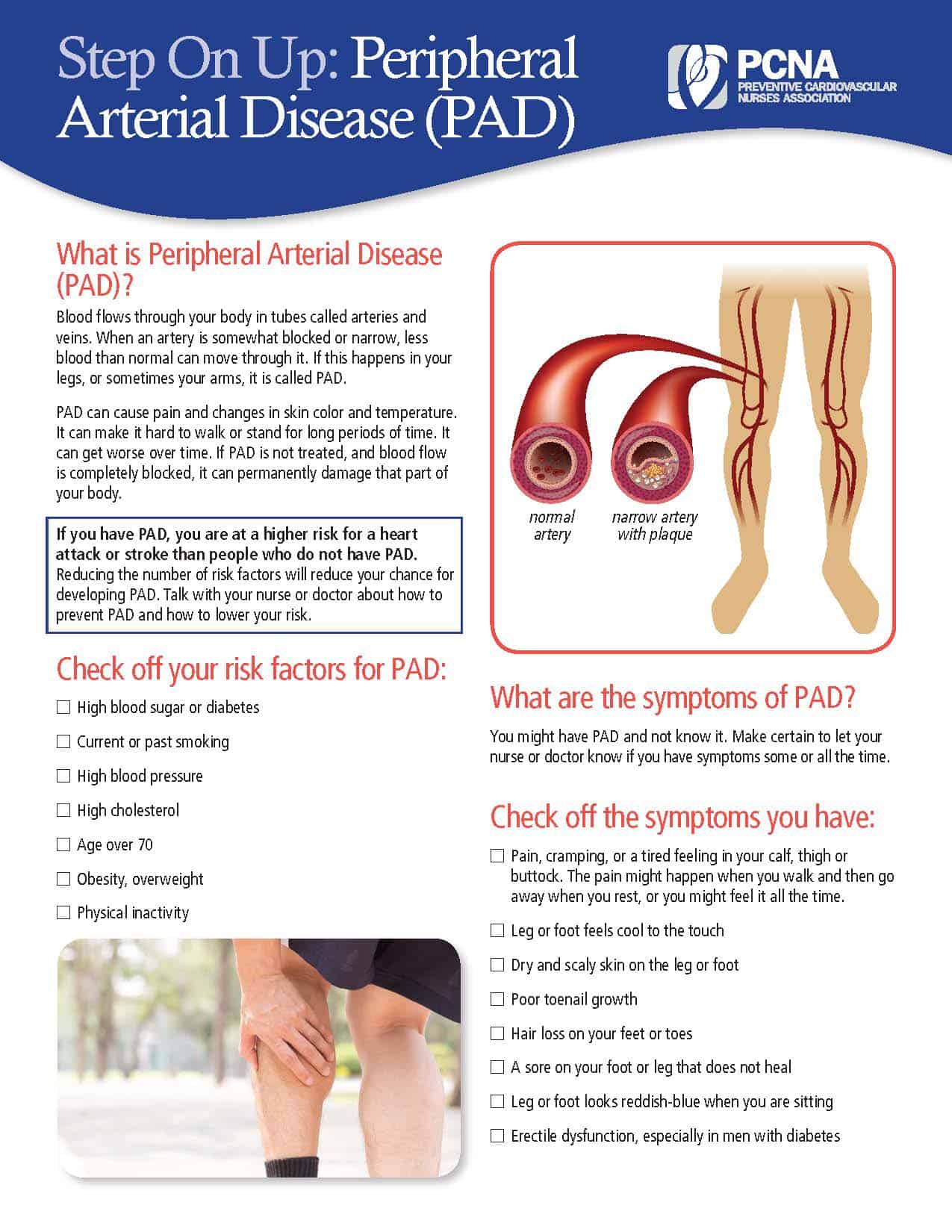
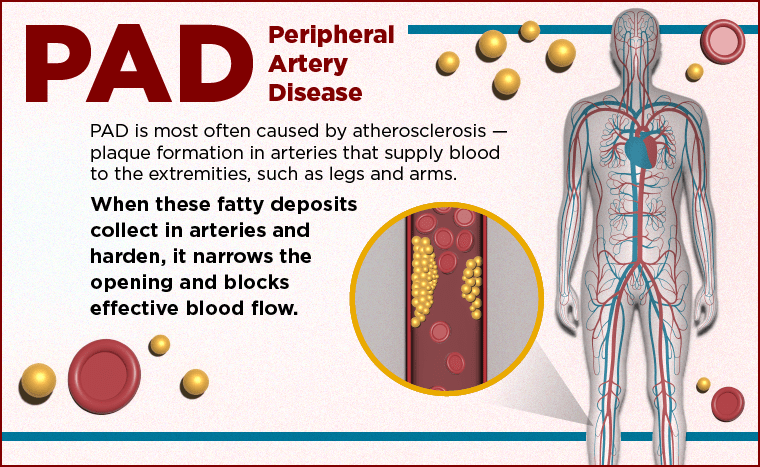
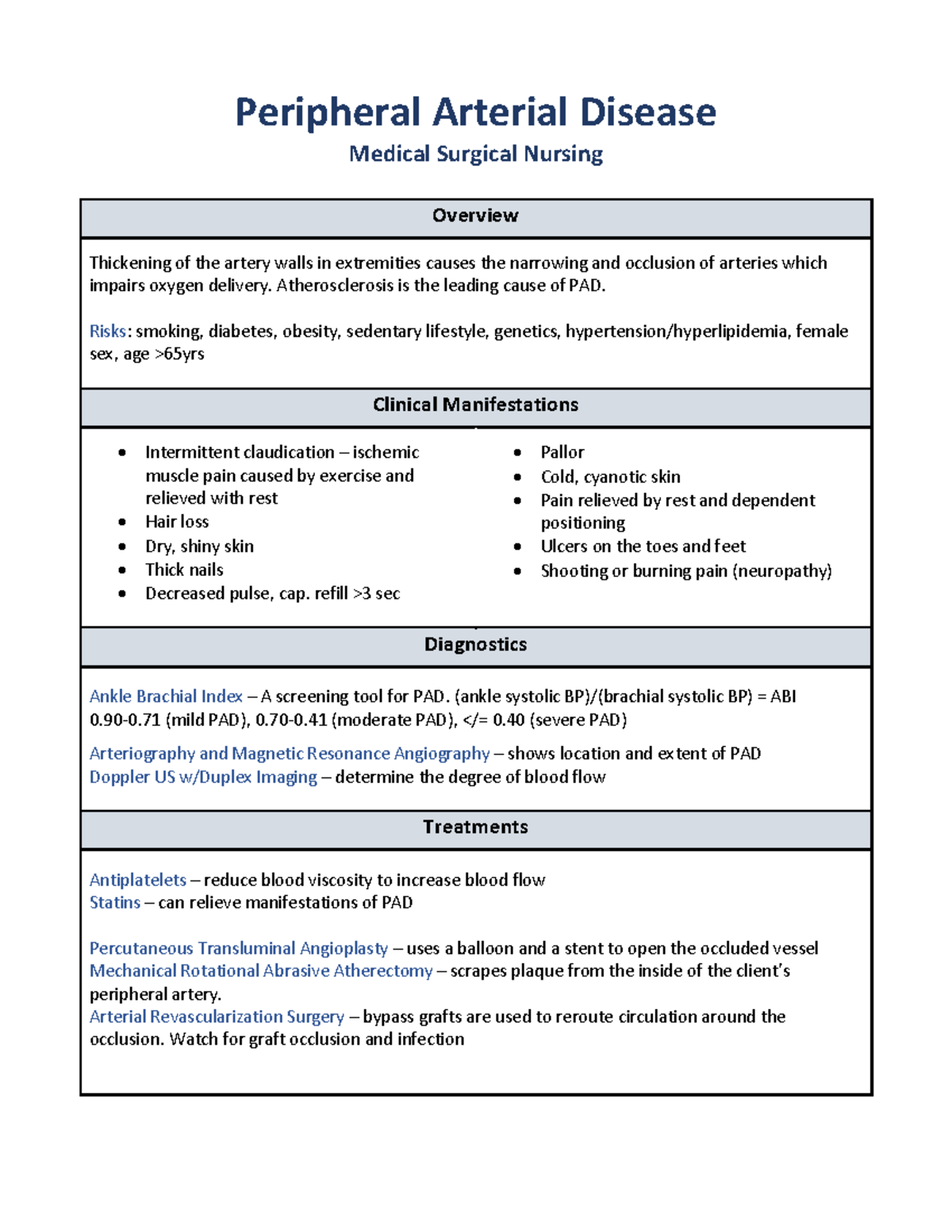
The insidious creep of Peripheral Arterial Disease (PAD) often goes unnoticed, a silent threat that can culminate in devastating consequences like amputation and stroke. Accurate and timely diagnosis is crucial, yet the process extends beyond mere clinical observation; it requires a nuanced understanding of the patient's individual circumstances, facilitated by effective nursing diagnoses.
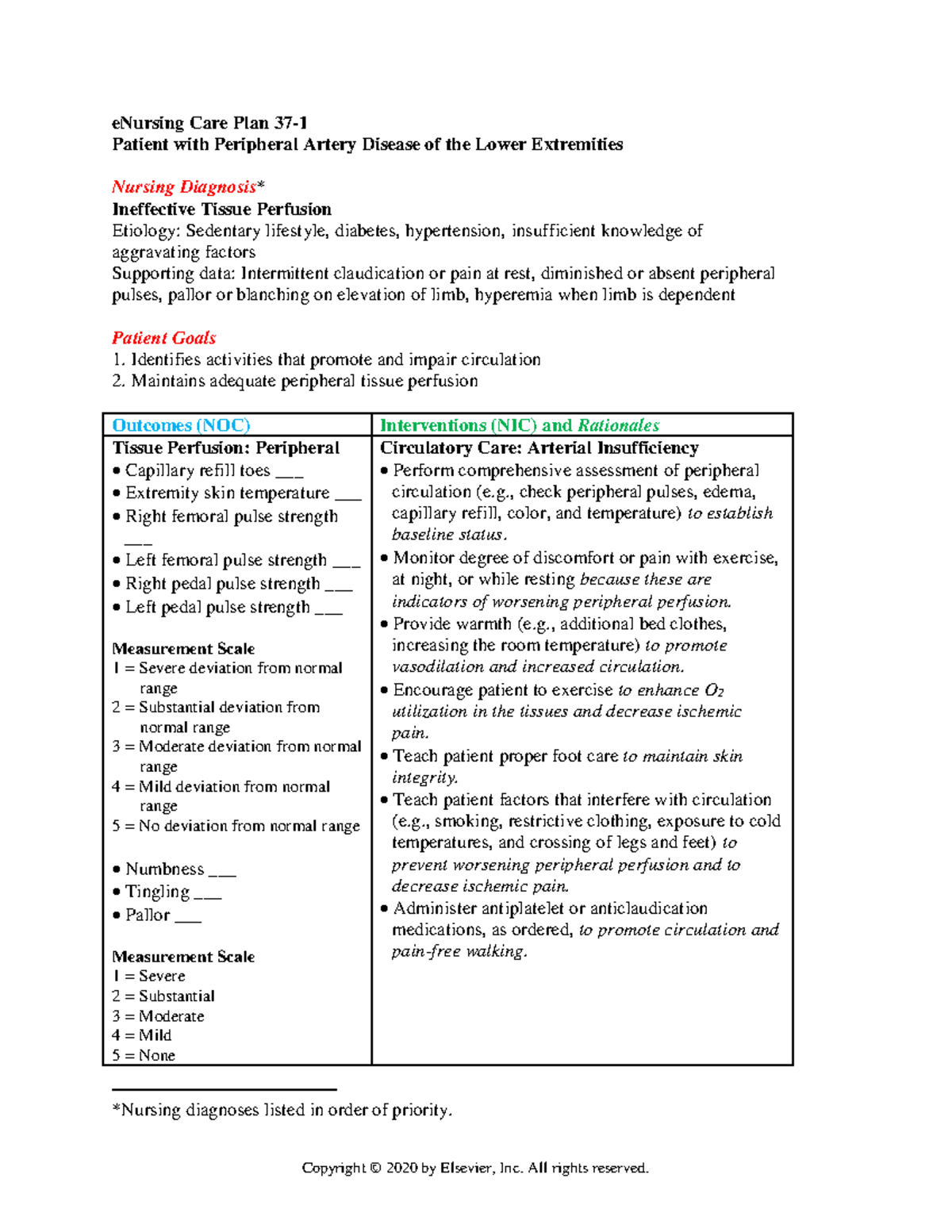
Nursing diagnoses, focusing on patient responses to health conditions rather than the disease itself, are instrumental in tailoring care plans for PAD patients. This approach addresses not just the physical manifestations of PAD, such as reduced blood flow and pain, but also the psychological and social challenges that significantly impact a patient's quality of life and adherence to treatment. By understanding the common nursing diagnoses associated with PAD, healthcare professionals can provide holistic, patient-centered care that improves outcomes and enhances well-being.
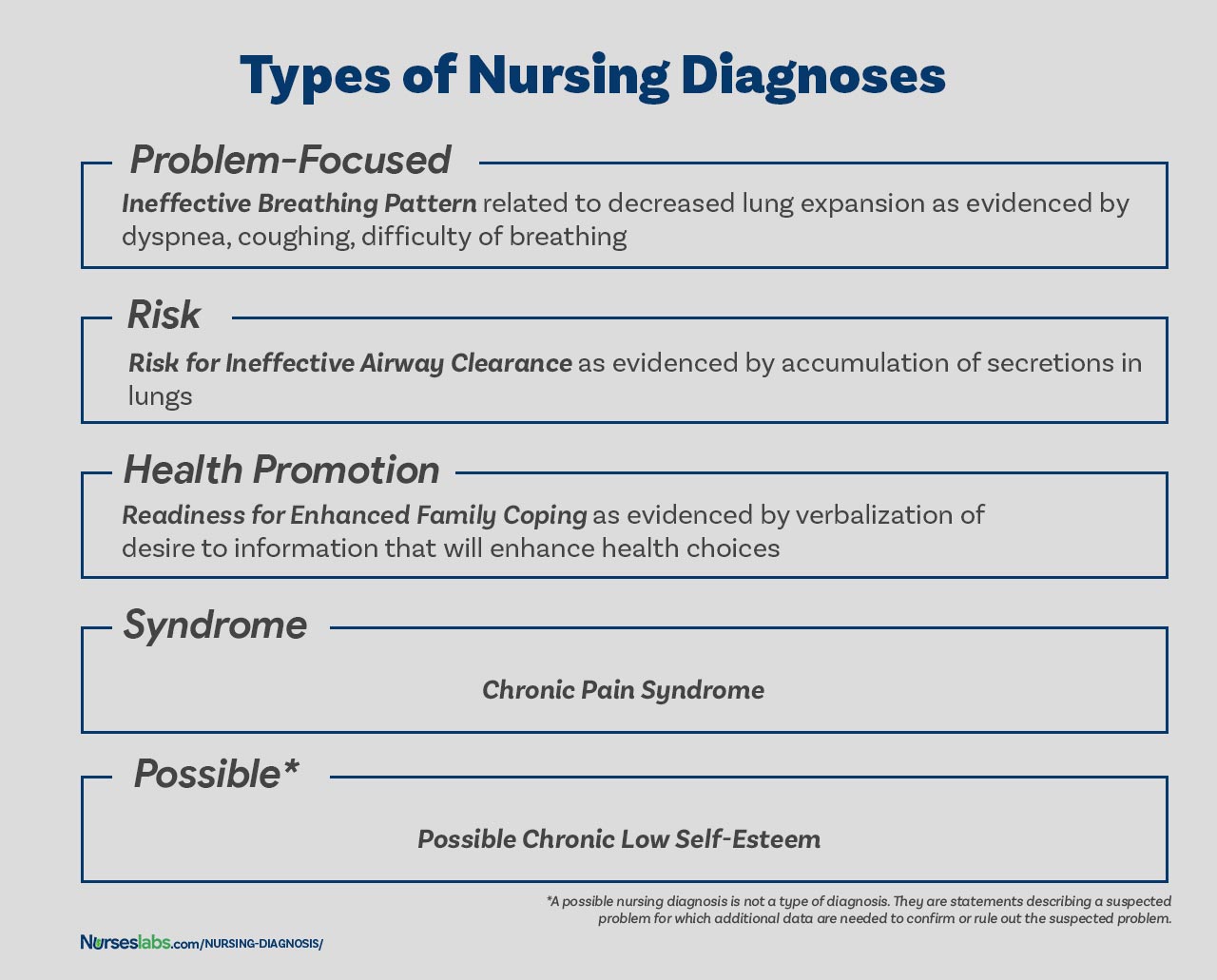
Common Nursing Diagnoses in Peripheral Arterial Disease
Several nursing diagnoses frequently emerge in the care of patients with PAD, each reflecting different facets of the disease's impact. These diagnoses guide nurses in formulating individualized care plans that address the unique needs of each patient.
Impaired Tissue Perfusion
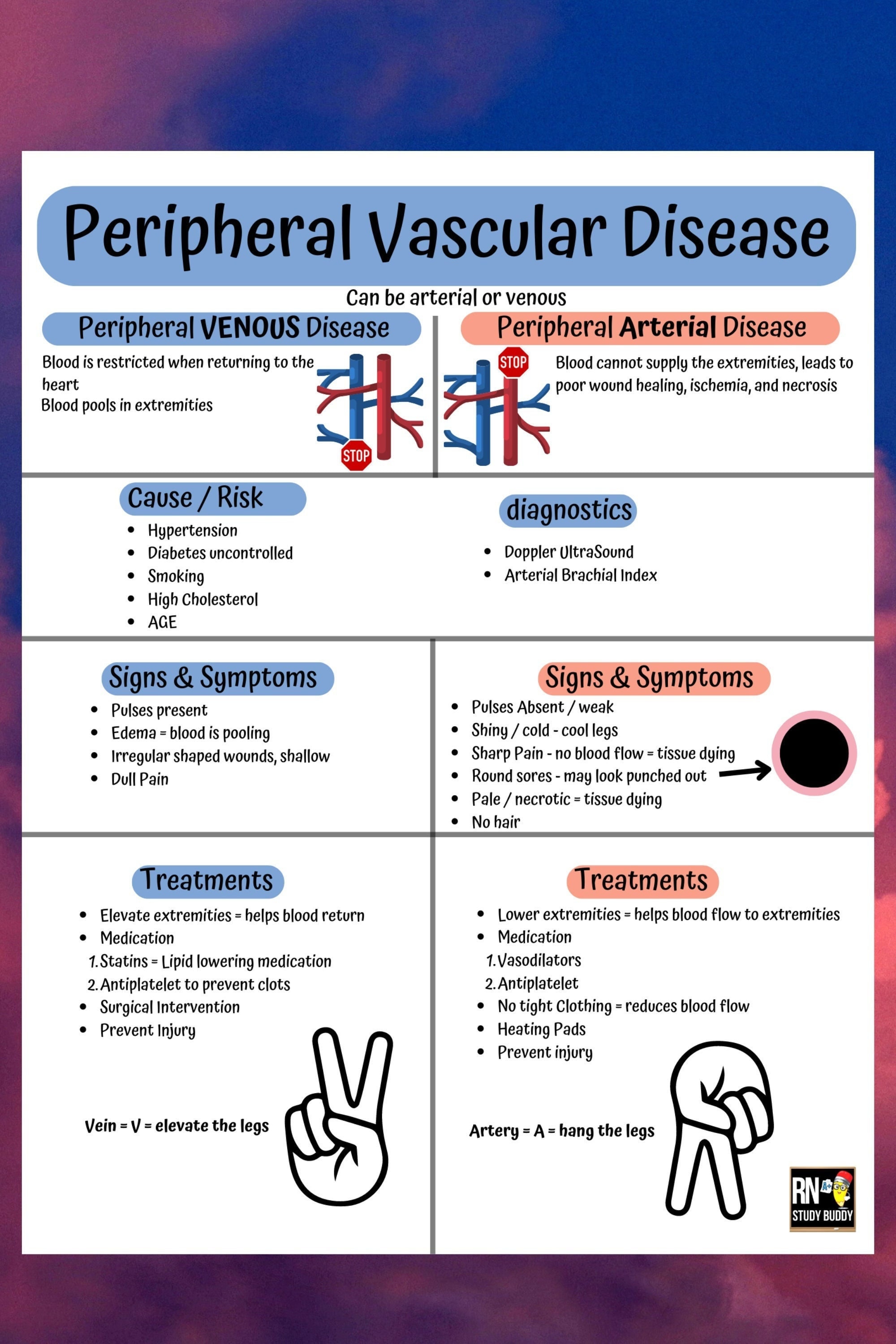
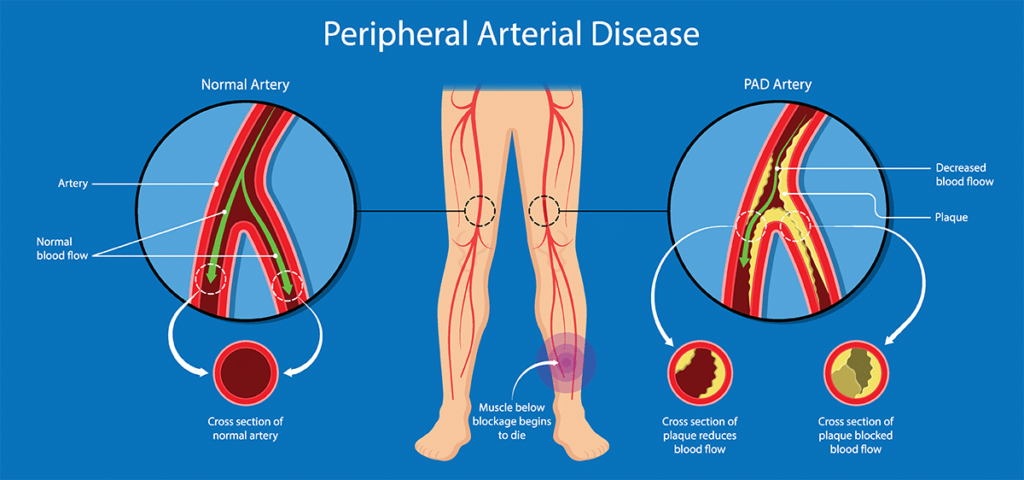
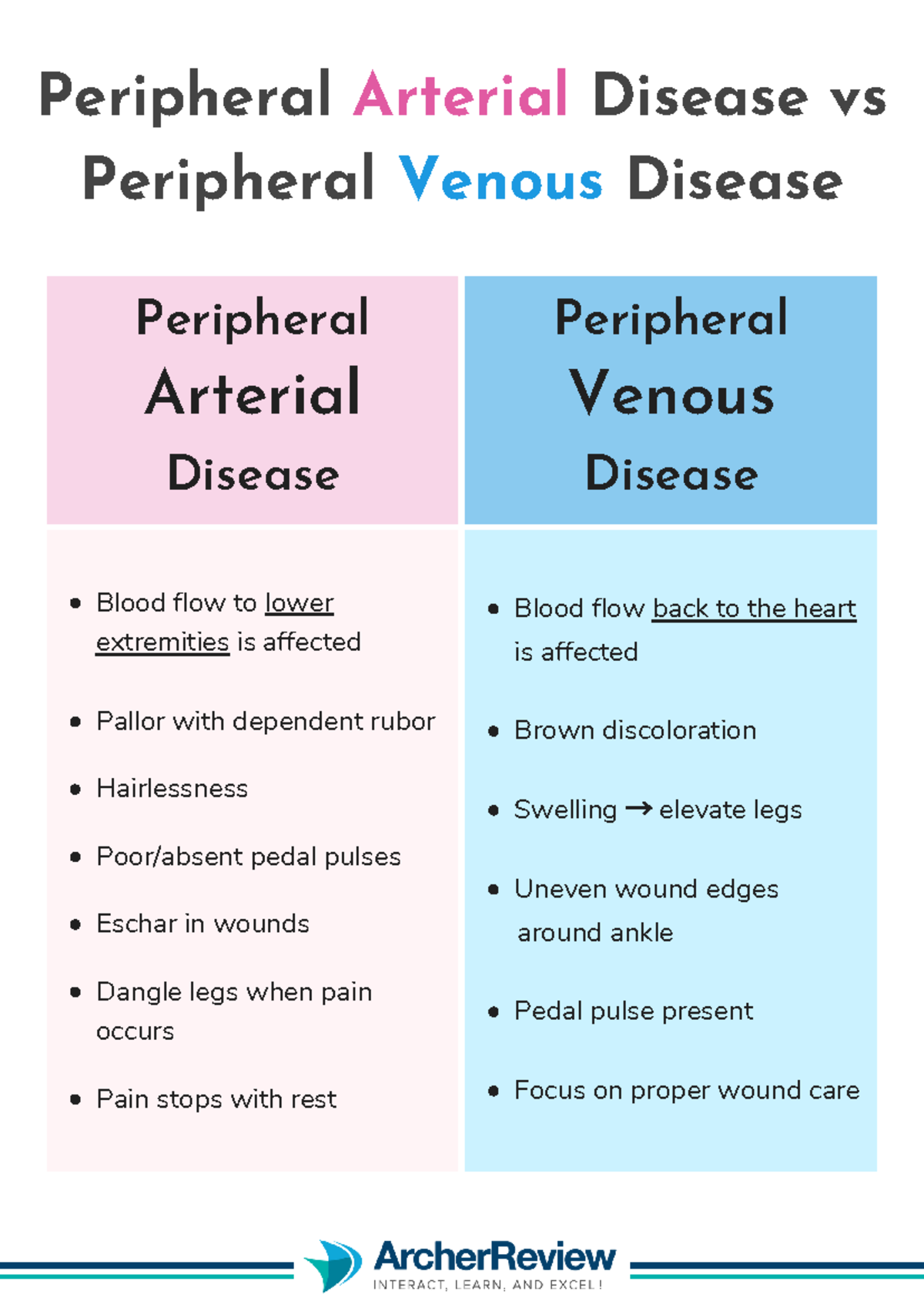
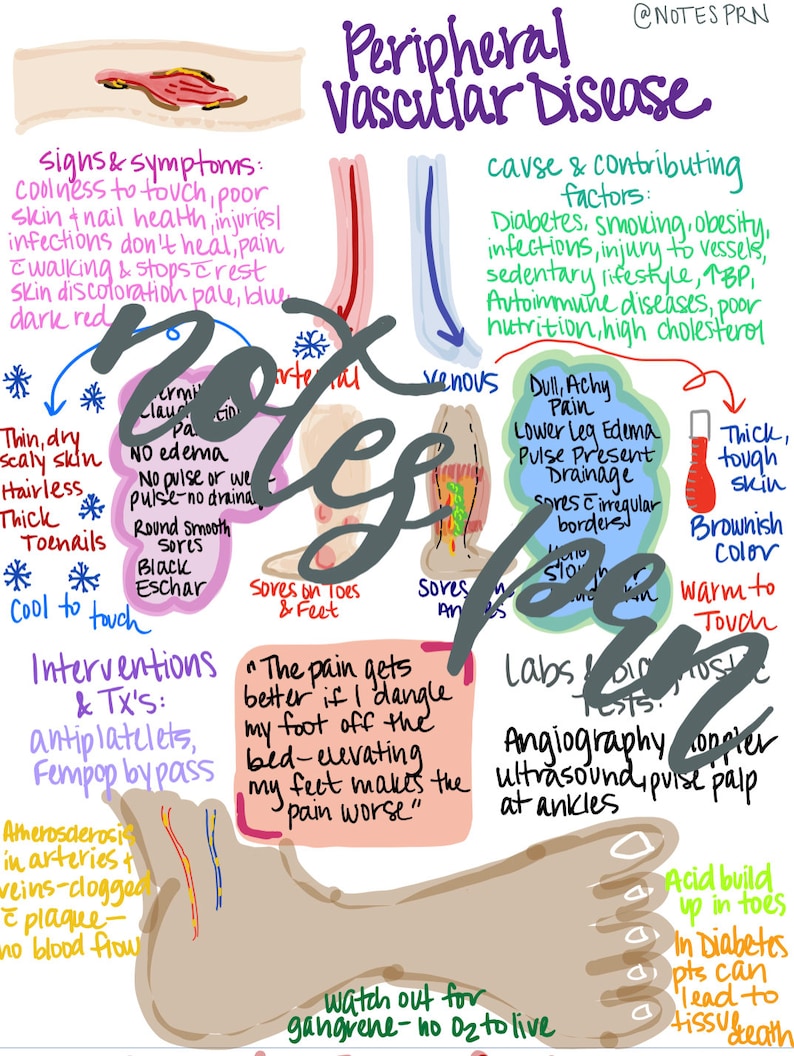
This is perhaps the most fundamental nursing diagnosis in PAD. It reflects the compromised blood flow to the extremities, leading to symptoms such as pain, coolness, pallor, and delayed wound healing.
The compromised blood flow results from arterial blockages caused by atherosclerosis. Assessing the degree of impairment and its impact on daily activities is crucial.
Chronic Pain
PAD often presents with intermittent claudication, a characteristic pain experienced in the legs during exercise that subsides with rest. This pain can significantly limit mobility and affect quality of life.
Nurses must differentiate between acute and chronic pain and employ appropriate pain management strategies.
Risk for Infection
Reduced blood flow impairs the body's natural defenses, increasing the risk of infection, particularly in the lower extremities. Even minor injuries can easily progress to serious infections.
This is especially important for patients with diabetes. Diligent foot care and preventive measures are essential.
Impaired Physical Mobility
Pain and discomfort associated with PAD can significantly restrict physical activity. This can lead to deconditioning, further limiting mobility and overall functionality.
Encouraging gradual increases in activity and providing assistive devices can improve mobility.
Knowledge Deficit
Many patients lack a comprehensive understanding of PAD, its risk factors, and its management. This can lead to poor adherence to treatment plans and lifestyle modifications.
Education regarding medication adherence, smoking cessation, and proper foot care is vital.
Ineffective Health Management
PAD requires a long-term commitment to lifestyle changes, including diet, exercise, and medication adherence. Some patients struggle to effectively manage their health condition.
Addressing barriers to adherence and providing ongoing support are crucial.
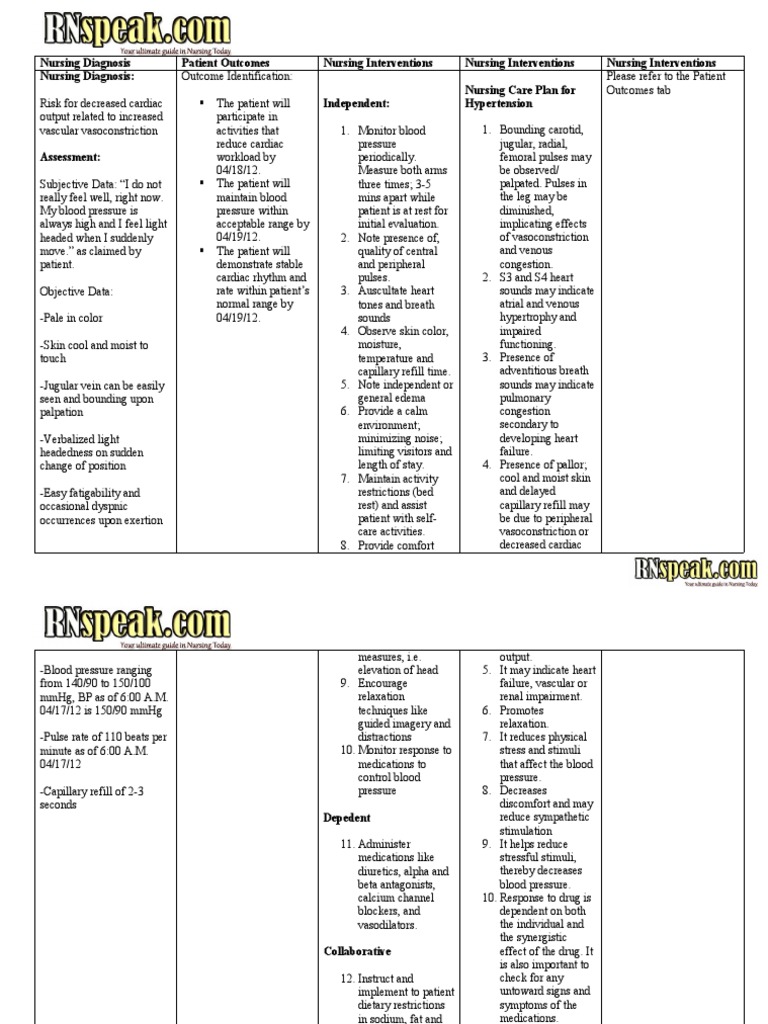
Assessment and Diagnostic Reasoning
Accurate assessment is foundational to the identification of appropriate nursing diagnoses. This involves a thorough patient history, physical examination, and diagnostic testing.
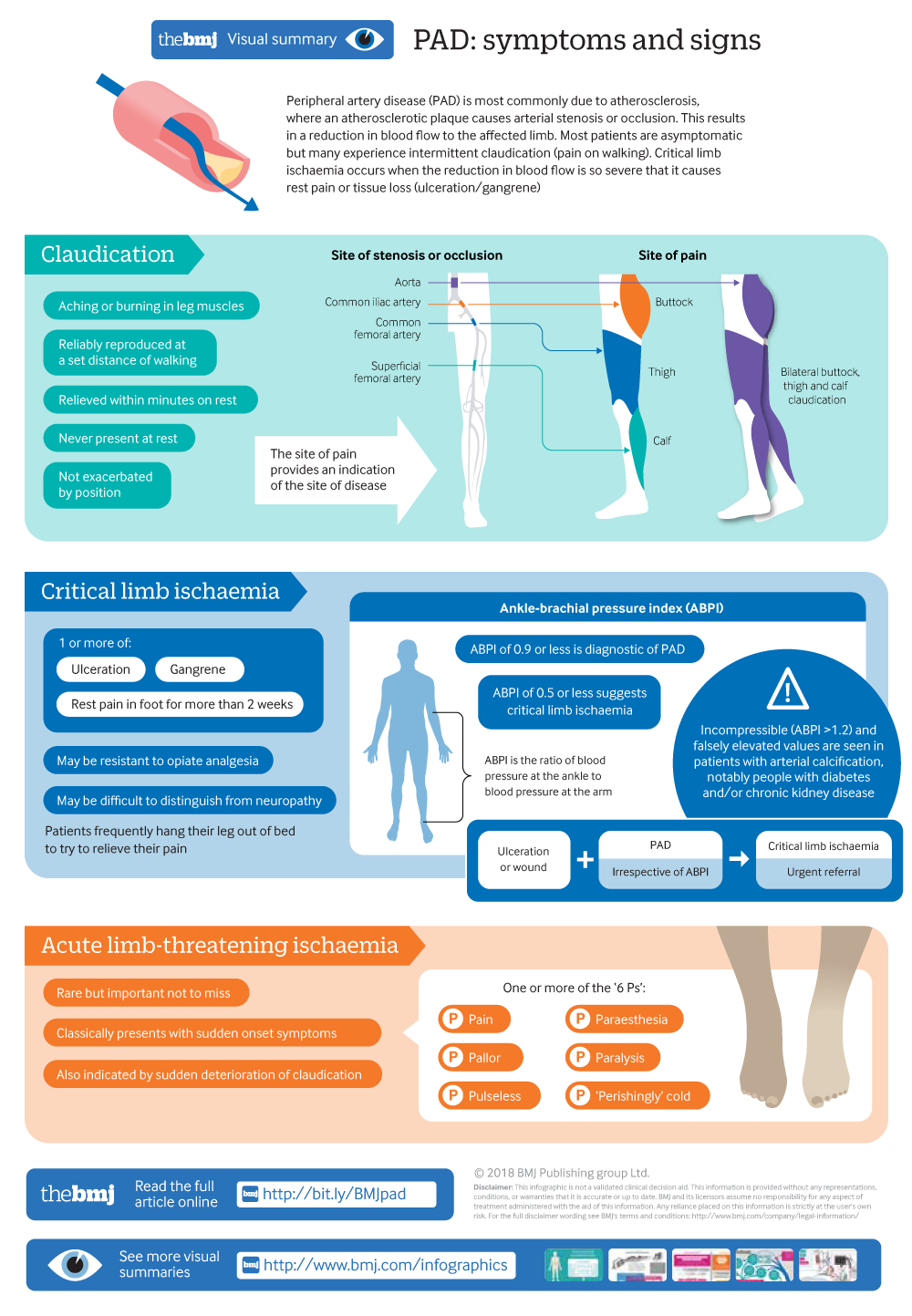
Key assessment findings include: ankle-brachial index (ABI) measurements, pulse assessment, skin temperature and color, and patient reports of pain and functional limitations.
The nursing process relies on critical thinking to analyze assessment data. This entails differentiating between signs and symptoms, identifying patterns, and recognizing potential complications.
For example, persistent leg pain at rest, along with non-healing ulcers, might indicate critical limb ischemia, a severe form of PAD requiring immediate intervention.
Nursing Interventions and Care Planning
Based on the identified nursing diagnoses, nurses develop individualized care plans that address the patient's specific needs. These plans incorporate a range of interventions aimed at improving tissue perfusion, managing pain, preventing infection, promoting mobility, and enhancing knowledge.
Examples of nursing interventions include: positioning to promote blood flow, administering pain medication as prescribed, providing meticulous wound care, educating patients on proper foot hygiene, and encouraging participation in supervised exercise programs.
Collaborative care is paramount, involving physicians, vascular surgeons, physical therapists, and other healthcare professionals. Open communication and shared decision-making are essential for optimal patient outcomes.
The Role of Patient Education
Patient education is a cornerstone of effective PAD management. Empowering patients with knowledge about their condition, its risk factors, and its treatment options promotes self-management and improves adherence to recommended lifestyle changes.
This includes educating patients on smoking cessation, healthy dietary choices, regular exercise, and proper foot care. Regular monitoring and follow-up appointments are also critical to detect and address any complications early.
"Effective patient education is not just about providing information; it's about empowering individuals to take control of their health and make informed decisions about their care," says Dr. Jane Smith, a leading vascular nurse specialist.
Future Directions in Nursing Diagnosis for PAD
The field of nursing diagnosis is constantly evolving, with ongoing research aimed at refining existing diagnoses and developing new ones that better reflect the complexities of PAD. Advances in technology, such as telehealth and wearable sensors, offer opportunities to remotely monitor patients and detect early signs of complications.
Furthermore, there is a growing emphasis on incorporating patient-reported outcomes into the diagnostic process, ensuring that care is truly patient-centered and tailored to individual needs and preferences. By embracing innovation and prioritizing patient engagement, nurses can continue to play a vital role in improving the lives of individuals living with PAD.
Ultimately, the effective application of nursing diagnoses in PAD requires a commitment to holistic care, evidence-based practice, and ongoing professional development. By embracing these principles, nurses can make a significant difference in the lives of patients affected by this debilitating condition.
![Nursing Diagnosis For Peripheral Arterial Disease PVD vs PAD [+ Free Cheat Sheet] | Lecturio Nursing](https://cdn.lecturio.com/assets/Nursing_CS_Assessment-of-Peripheral-Arterial-Disease.jpg)