Nursing Interventions For Ineffective Airway Clearance
In hospitals and homes alike, the silent struggle for breath unfolds daily. Patients battling conditions that obstruct their airways face a daunting challenge, one that can rapidly escalate from discomfort to life-threatening respiratory distress. The effectiveness of nursing interventions in these critical moments often determines the patient's trajectory toward recovery or further decline.
This article delves into the essential nursing interventions aimed at addressing ineffective airway clearance, a condition where individuals are unable to clear secretions or obstructions from their respiratory tract to maintain a clear airway. We will explore evidence-based practices, highlighting the importance of assessment, specific techniques, and ongoing monitoring. The goal is to provide a comprehensive overview of the crucial role nurses play in ensuring patients can breathe freely and safely.
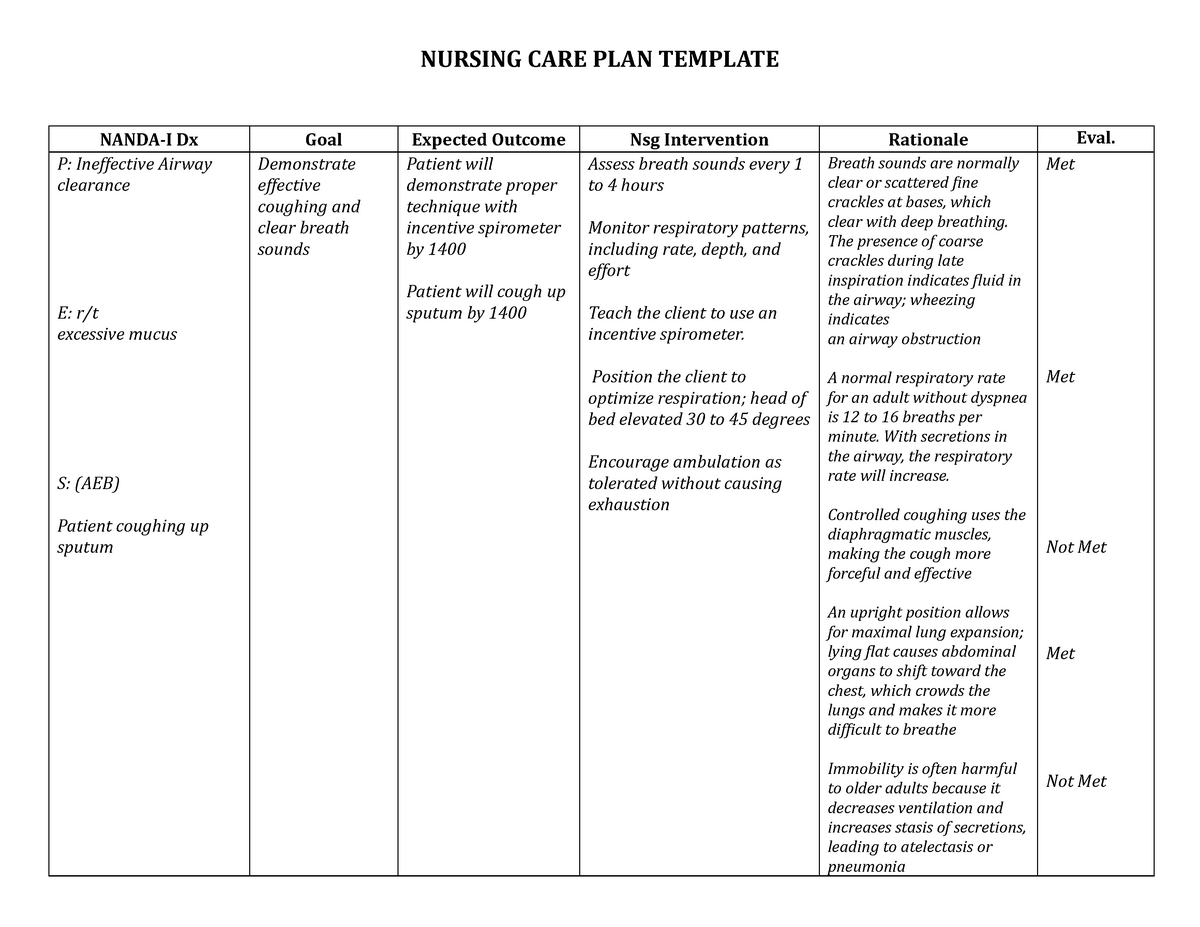
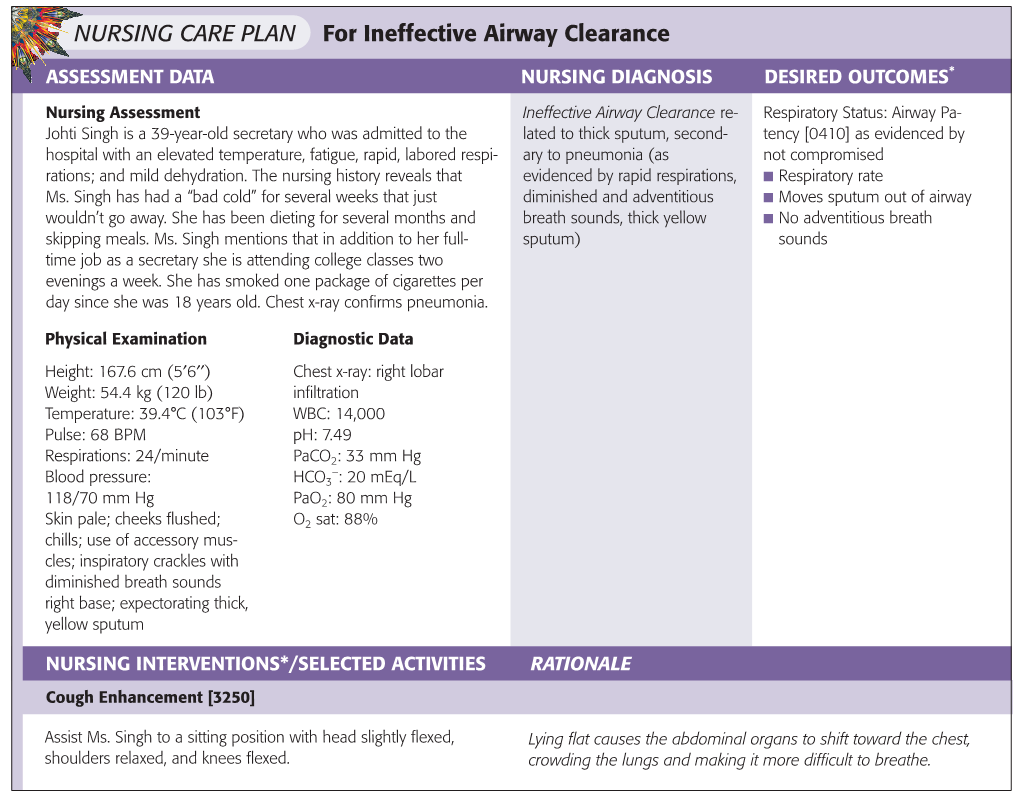
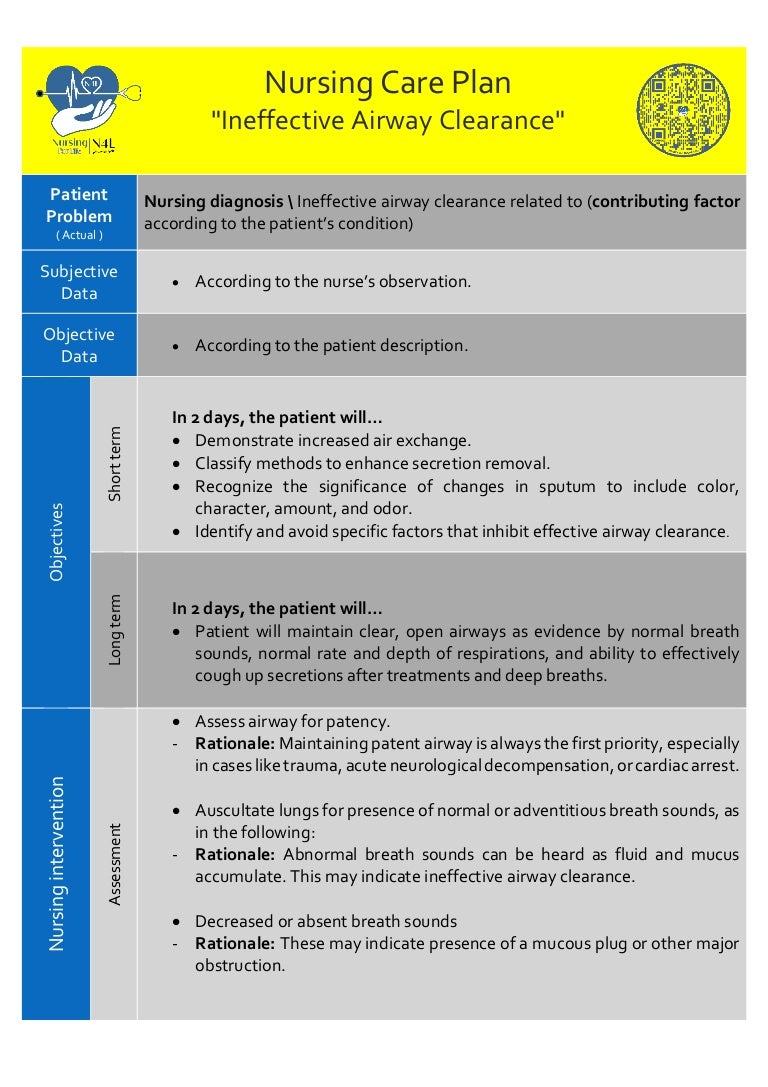
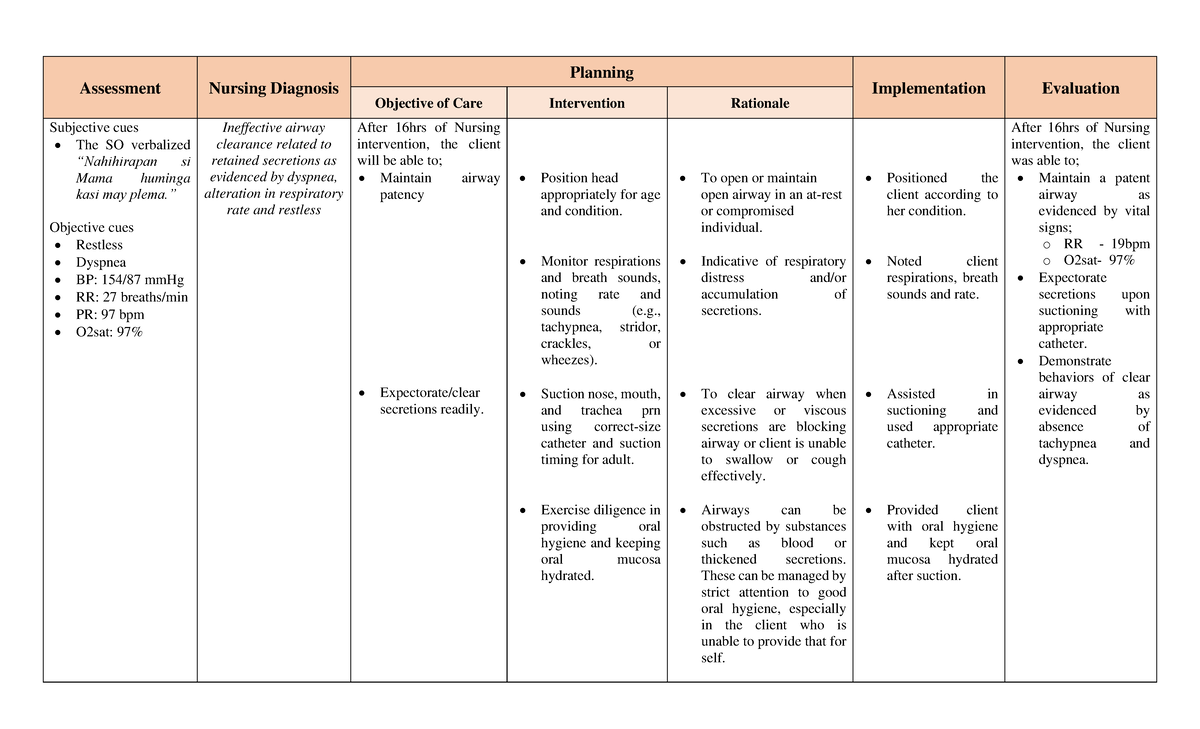
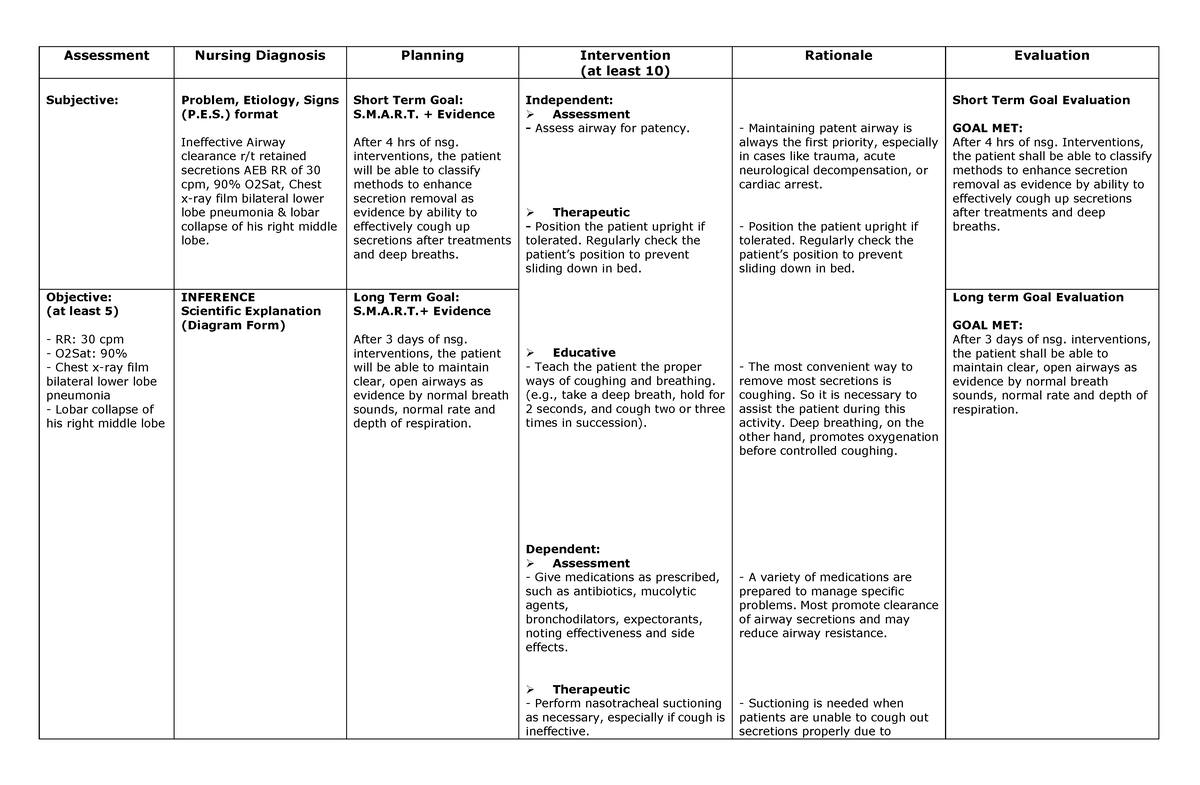
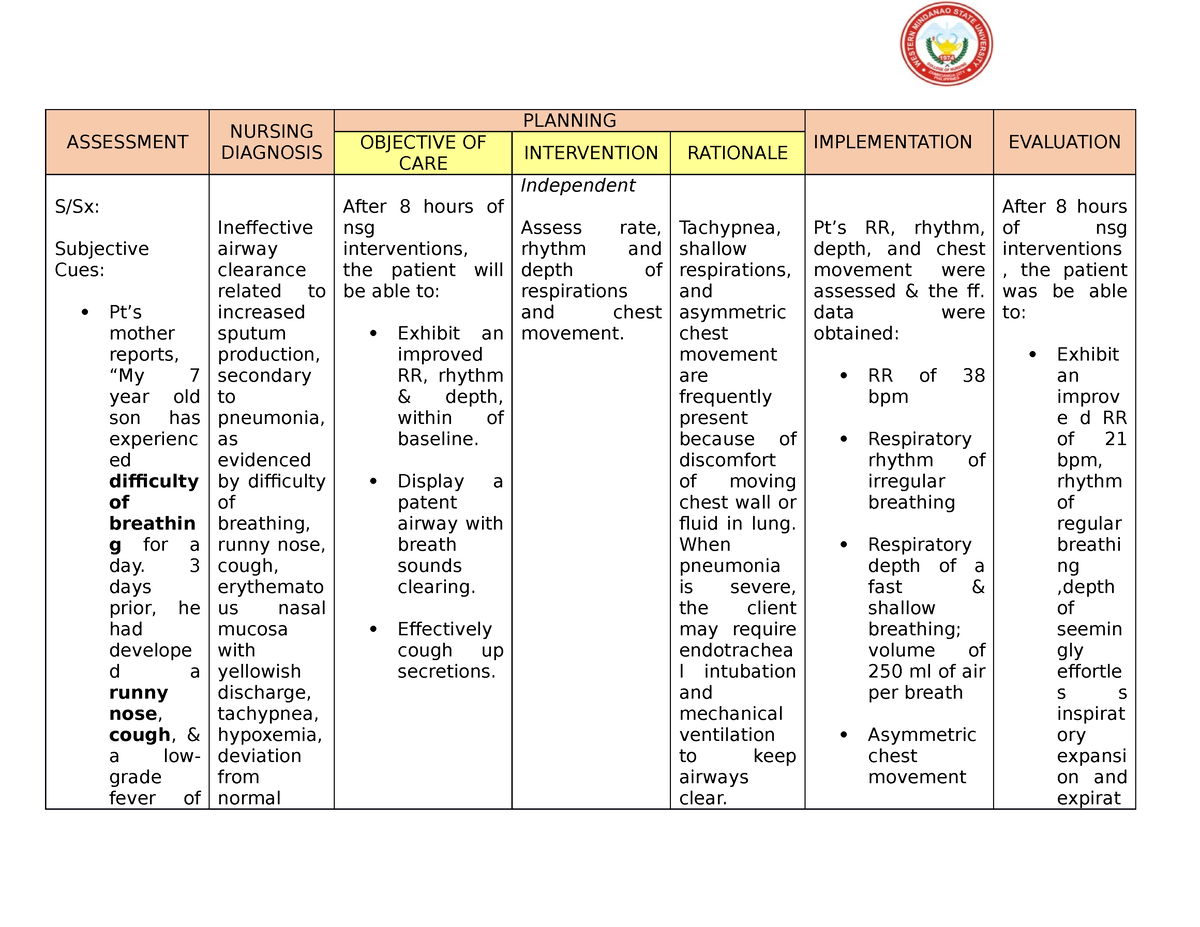
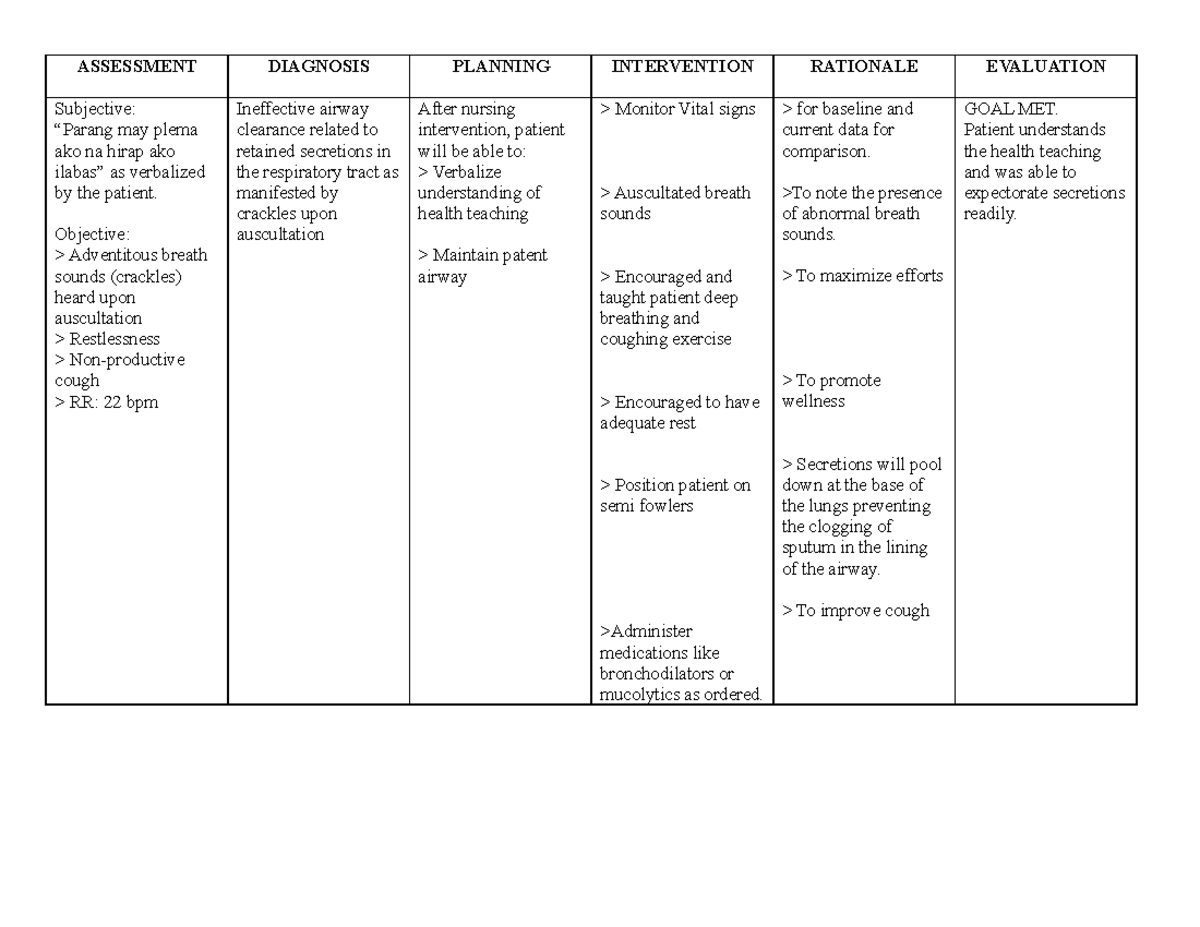
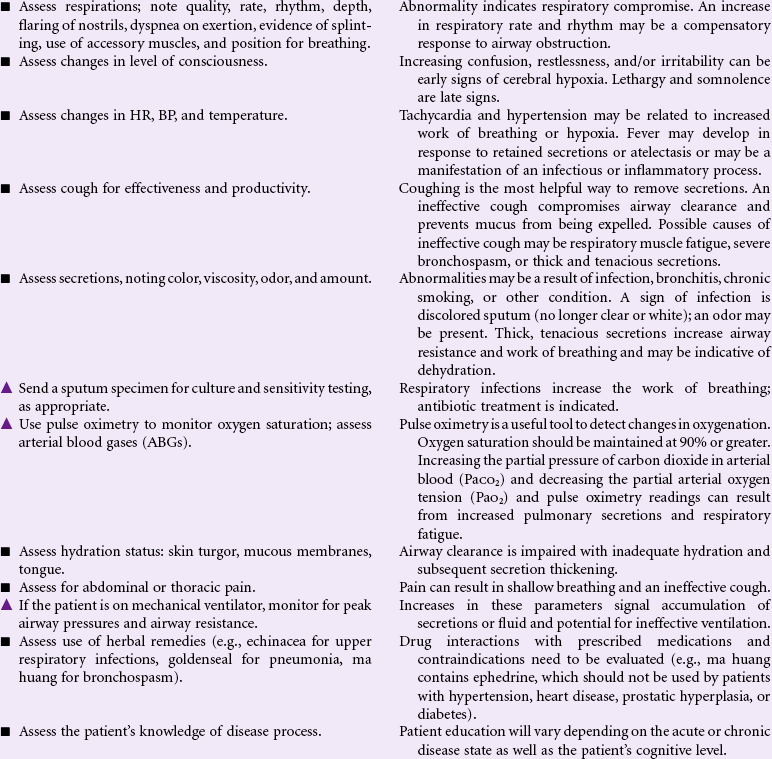
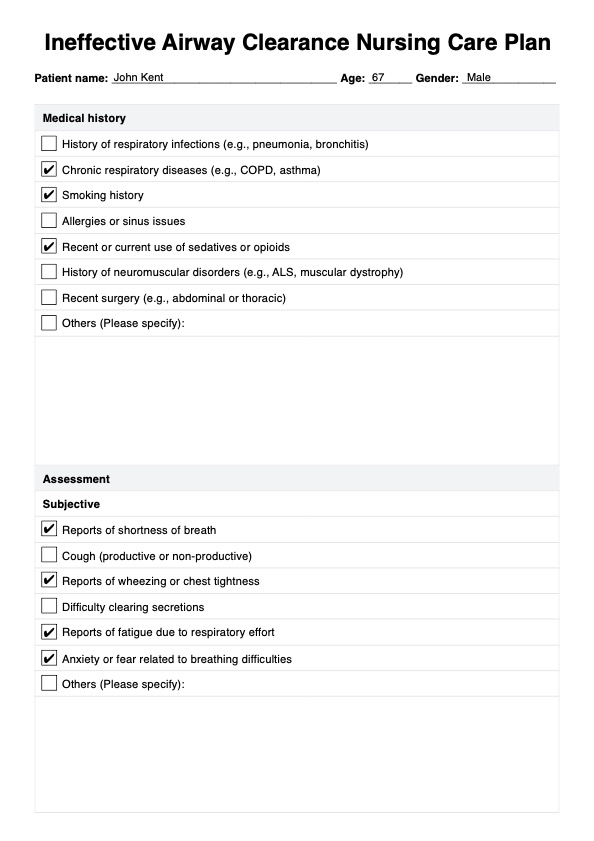
Assessment: The Foundation of Effective Intervention
Thorough and continuous assessment is the cornerstone of managing ineffective airway clearance. Nurses must vigilantly monitor vital signs, including respiratory rate, oxygen saturation, and heart rate. Auscultation of lung sounds is crucial to identify abnormal sounds like wheezing, crackles, or rhonchi, indicating potential airway obstruction.
Observing the patient's effort of breathing is equally important. Look for signs of increased work of breathing such as nasal flaring, intercostal retractions, and the use of accessory muscles. The patient's cough, both its strength and effectiveness, should be assessed, along with the quantity and characteristics of any sputum produced.
A patient's mental status can also provide clues. Restlessness, anxiety, or confusion can indicate hypoxemia. A comprehensive assessment provides the data needed to develop an individualized plan of care.
Airway Clearance Techniques: A Multifaceted Approach
Several techniques can be employed to assist patients in clearing their airways. Coughing and deep breathing exercises are often the first line of defense. Encouraging patients to take slow, deep breaths and then forcefully cough can help mobilize secretions.
Hydration plays a crucial role in thinning secretions, making them easier to expectorate. Nurses should encourage adequate fluid intake, unless contraindicated by the patient's medical condition. Humidification, through the use of humidifiers or nebulizers, can also help to moisten the airway and thin secretions.
Postural drainage, often used in conjunction with chest physiotherapy, utilizes gravity to help drain secretions from specific lung segments. The patient is positioned in various ways to facilitate drainage. Chest percussion and vibration, performed by a trained professional, can further loosen secretions.
Suctioning is a critical intervention for patients unable to clear their airway effectively on their own. Nasotracheal suctioning and oropharyngeal suctioning are common techniques. Proper technique is essential to minimize the risk of complications such as mucosal trauma, hypoxia, and vagal stimulation.
Pharmacological Interventions: Adjuncts to Airway Clearance
Medications can play a significant role in managing ineffective airway clearance. Bronchodilators, such as albuterol, can help to relax the muscles in the airways and improve airflow. These are often administered via nebulizer or metered-dose inhaler.
Mucolytics, like acetylcysteine (Mucomyst), can help to break down the bonds in mucus, making it easier to cough up. However, they should be used with caution as they can sometimes irritate the airway. Corticosteroids, either inhaled or systemic, can help to reduce inflammation in the airways.
Antibiotics are indicated if the ineffective airway clearance is due to a respiratory infection. The choice of antibiotic will depend on the specific pathogen identified. Pain management is also important, as pain can inhibit effective coughing and deep breathing.
Positioning and Mobilization: Promoting Lung Expansion
Proper positioning can significantly impact airway clearance. Elevating the head of the bed promotes lung expansion and reduces pressure on the diaphragm. Turning patients frequently, at least every two hours, can help to prevent the pooling of secretions in dependent lung regions.
Mobilization, even simple activities like sitting in a chair or ambulating, can improve lung expansion and promote secretion clearance. Encouraging patients to move around as tolerated is an important part of their care. For patients on mechanical ventilation, proning (placing the patient on their stomach) can sometimes improve oxygenation and ventilation.
Special Considerations: Pediatric and Geriatric Patients
Pediatric and geriatric patients present unique challenges when it comes to managing ineffective airway clearance. Infants and children have smaller airways, making them more susceptible to obstruction. Gentle suctioning techniques and careful monitoring are essential.
Older adults may have decreased cough strength and impaired mucociliary clearance. Hydration and humidification are particularly important in this population. Care must be taken to avoid overhydration in patients with underlying heart failure.
Both pediatric and geriatric patients may have difficulty communicating their needs, requiring nurses to be particularly attentive to subtle signs of respiratory distress. Family involvement can be invaluable in providing support and identifying changes in the patient's condition.
Monitoring and Evaluation: Ensuring Ongoing Effectiveness
Continuous monitoring is essential to evaluate the effectiveness of nursing interventions. Regularly assess respiratory rate, oxygen saturation, and lung sounds. Document the frequency and characteristics of cough and sputum production.
Adjust the plan of care as needed based on the patient's response to interventions. If the patient is not improving, consider escalating care, such as increasing the frequency of suctioning or administering additional medications. Communication with the healthcare team is critical to ensure optimal patient outcomes.
Patient education is an ongoing process. Teach patients and their families about effective coughing techniques, the importance of hydration, and how to recognize signs of respiratory distress. Empowering patients to participate in their own care can improve adherence to the plan and promote long-term airway clearance.
The Future of Airway Clearance: Innovations and Research
The field of airway clearance is constantly evolving, with new technologies and techniques emerging. High-frequency chest wall oscillation vests are becoming increasingly common, providing a non-invasive way to loosen secretions. Mechanical insufflation-exsufflation devices (cough assist devices) can help patients with weak cough muscles to clear their airways.
Research is ongoing to identify the most effective strategies for managing ineffective airway clearance in various patient populations. Studies are exploring the role of specific medications, the optimal frequency of suctioning, and the benefits of different positioning techniques.
Ultimately, the goal is to provide individualized, evidence-based care that optimizes airway clearance and improves patient outcomes. Nurses play a vital role in this process, utilizing their skills and knowledge to ensure that every patient can breathe easier.