Risk For Impaired Skin Integrity Care Plan
Hospitals and long-term care facilities are increasingly focusing on proactive measures to prevent skin breakdown in patients, leading to widespread adoption of the "Risk for Impaired Skin Integrity" care plan. This plan, a structured approach to identifying and mitigating factors that contribute to pressure ulcers and other skin damage, is becoming a standard of care across the nation. It aims to significantly reduce patient suffering, healthcare costs, and potential legal ramifications.
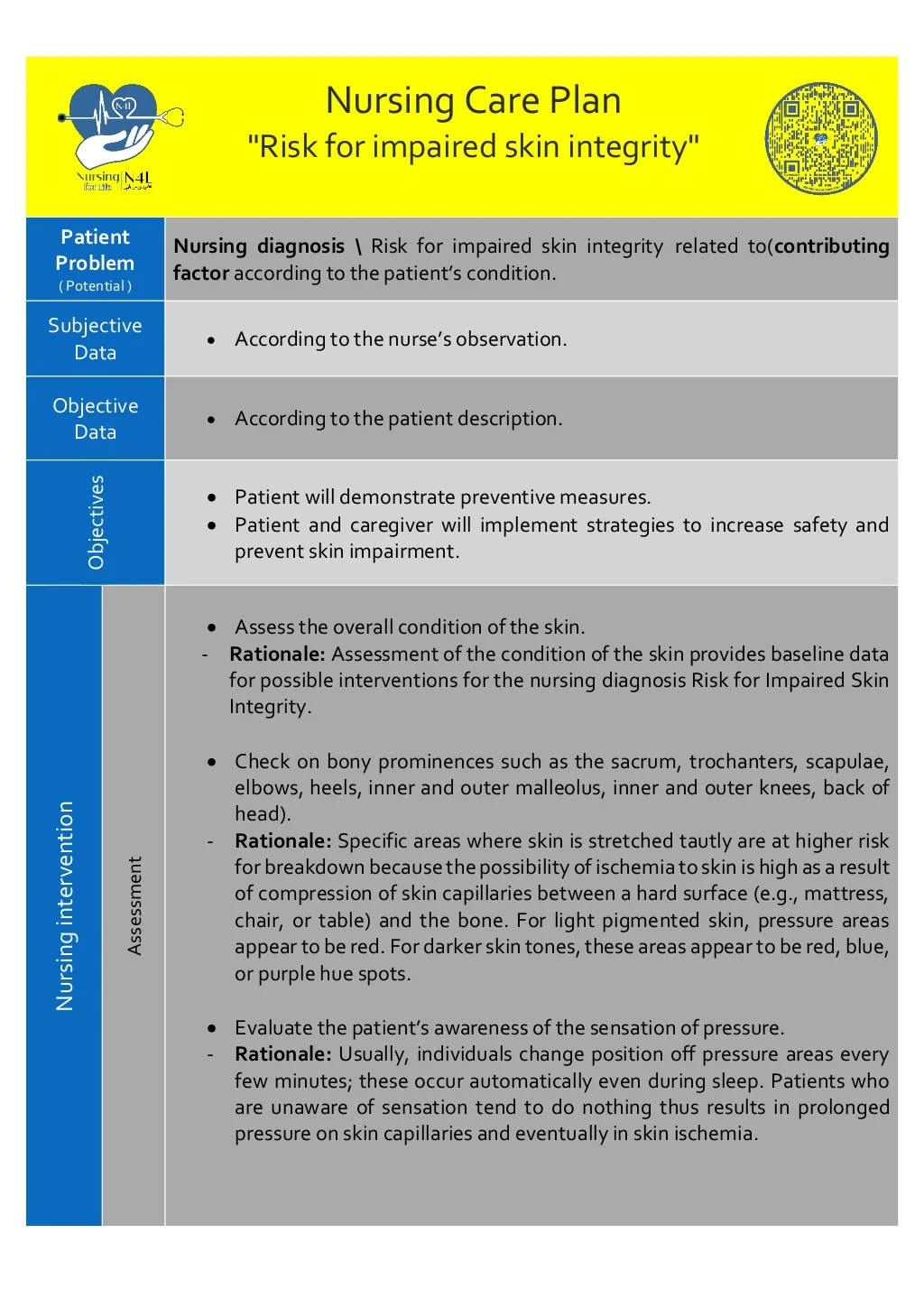
The Risk for Impaired Skin Integrity care plan focuses on early identification and intervention to minimize the potential for skin breakdown.
What is the Risk for Impaired Skin Integrity Care Plan?
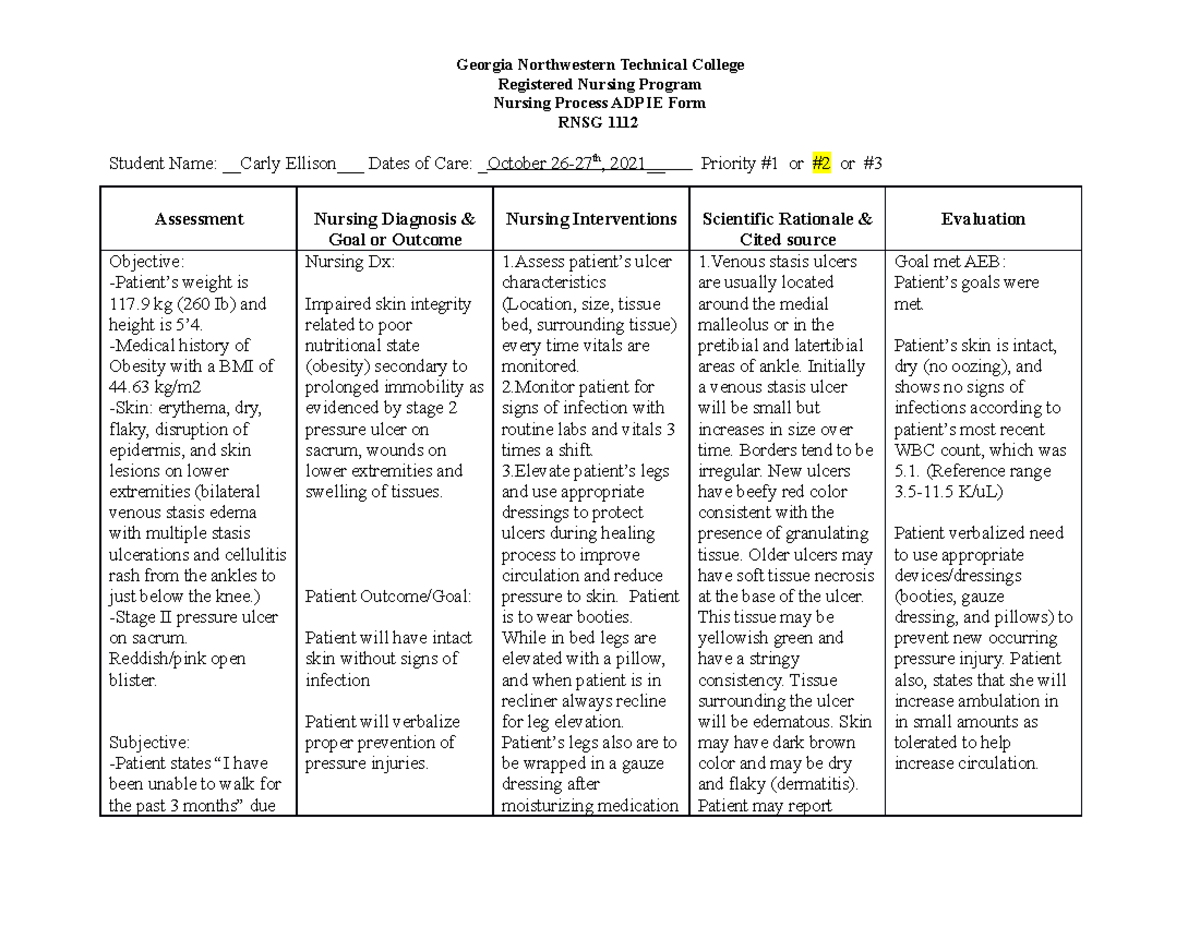
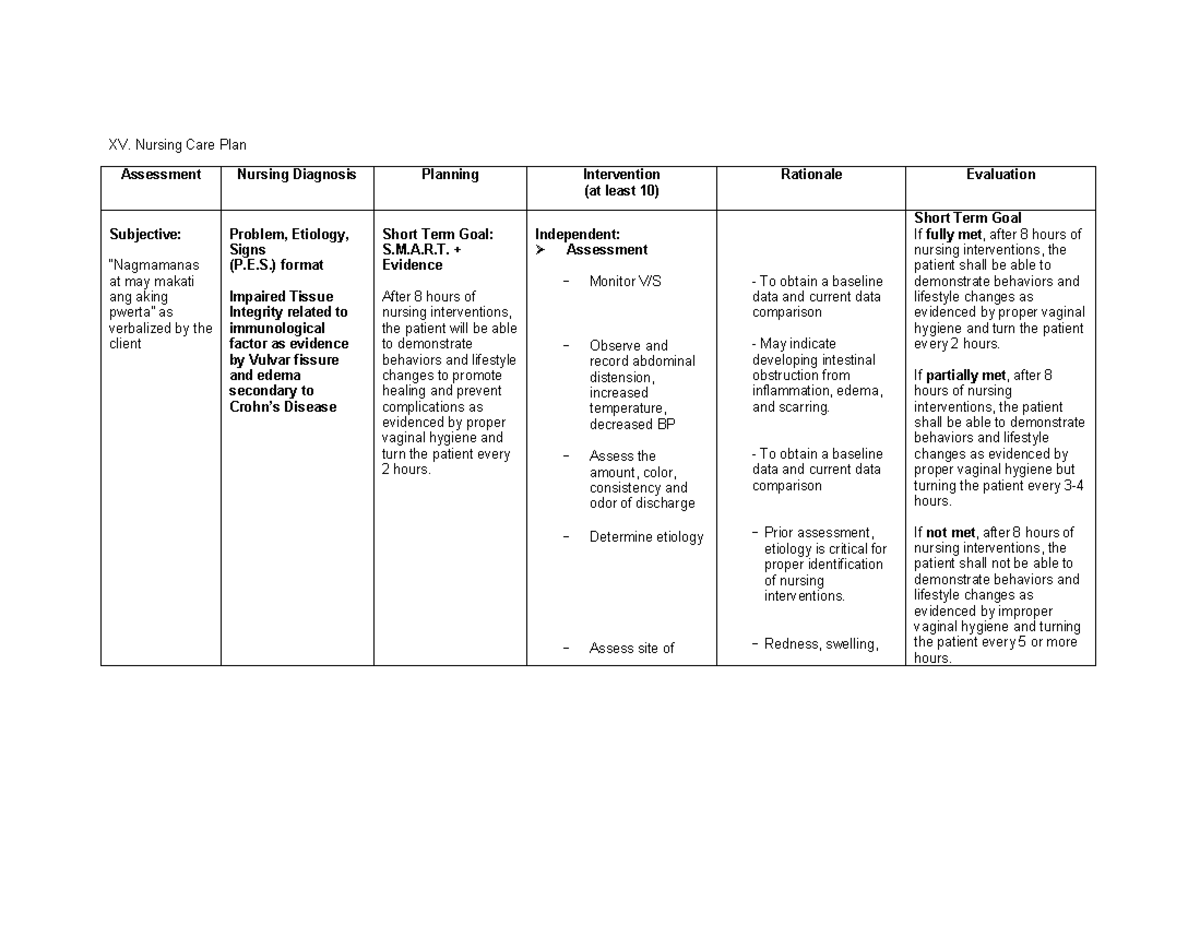
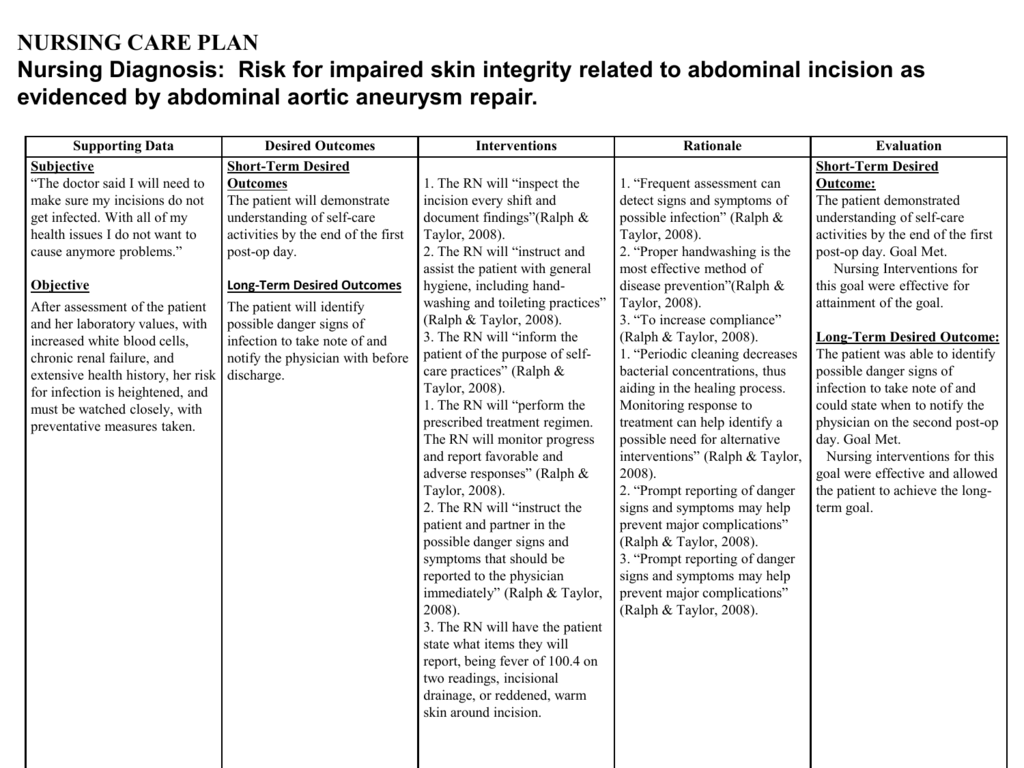
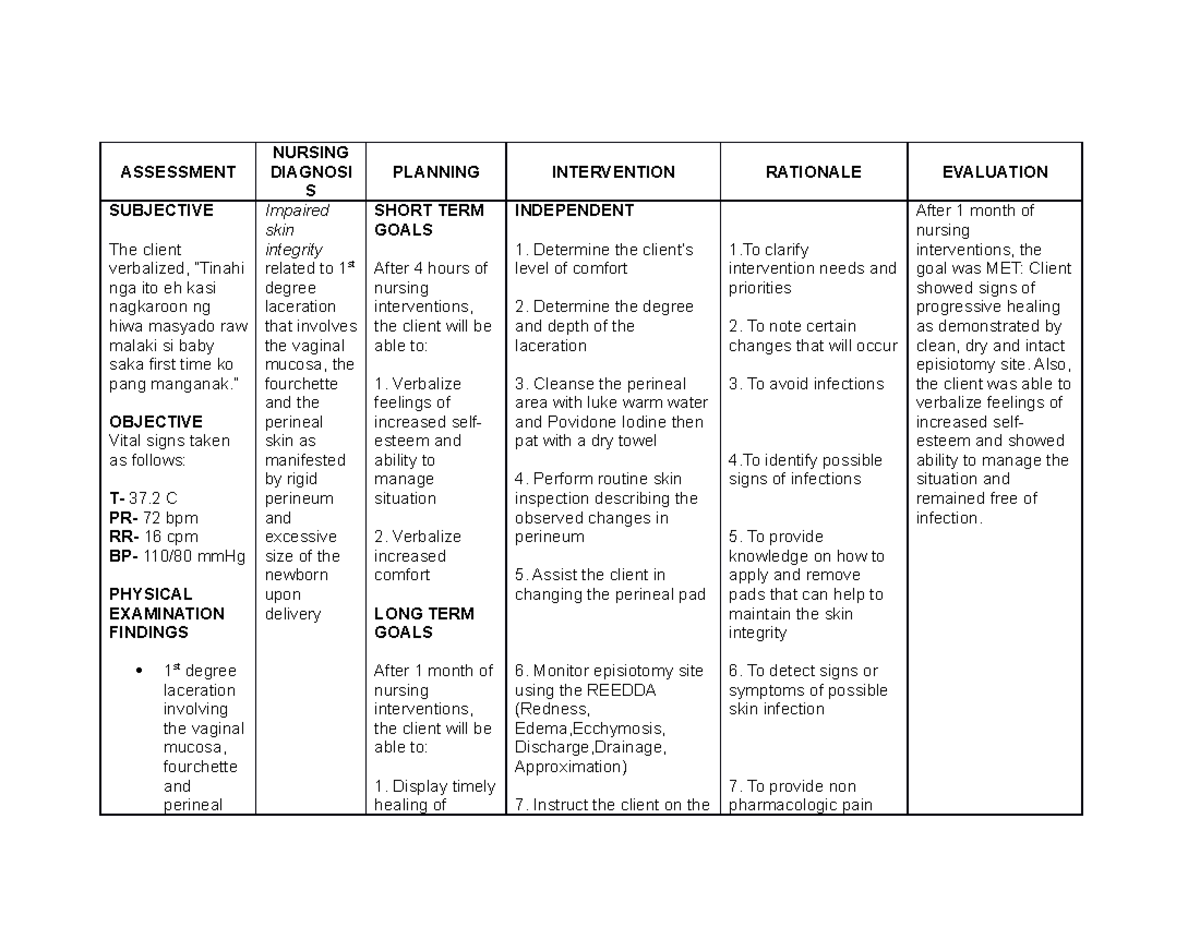
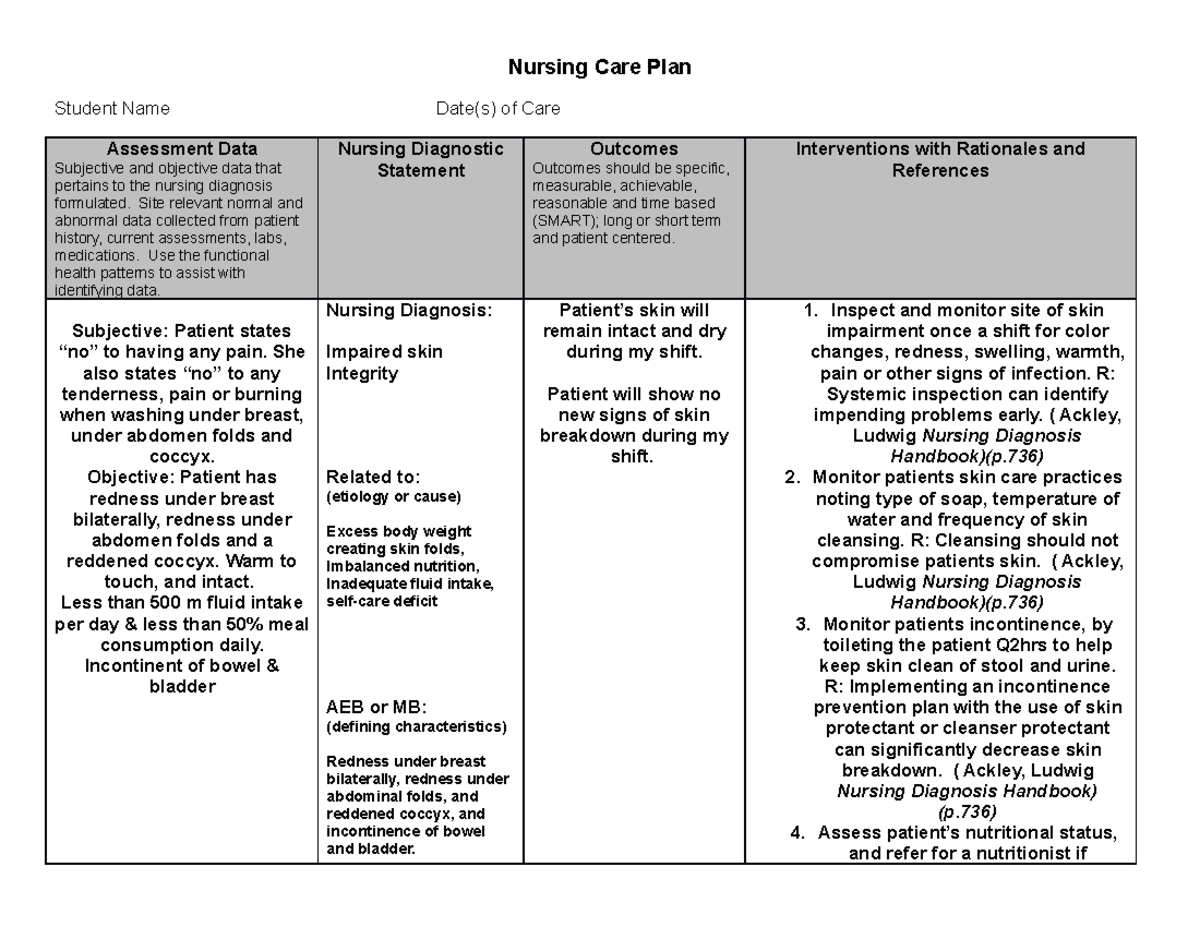
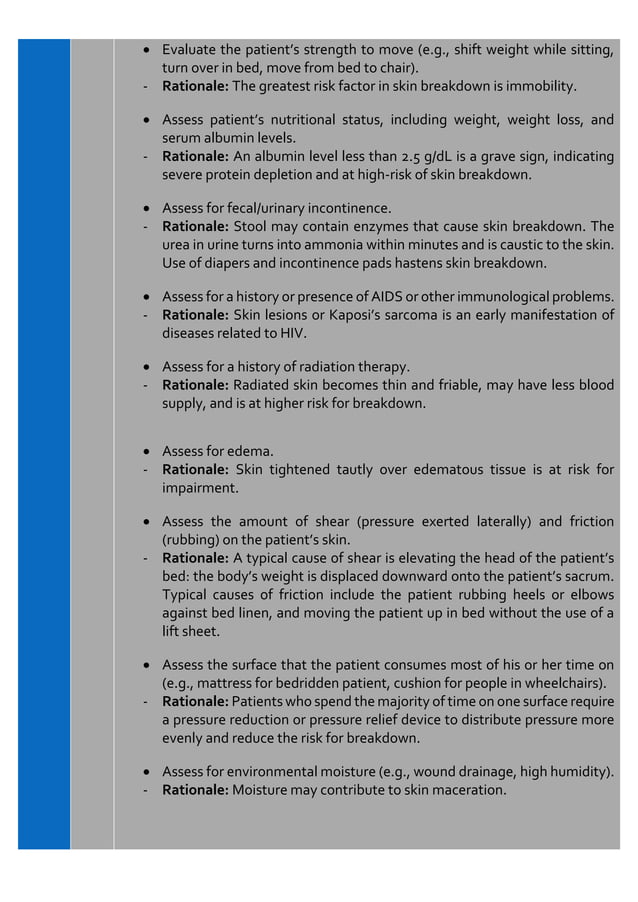
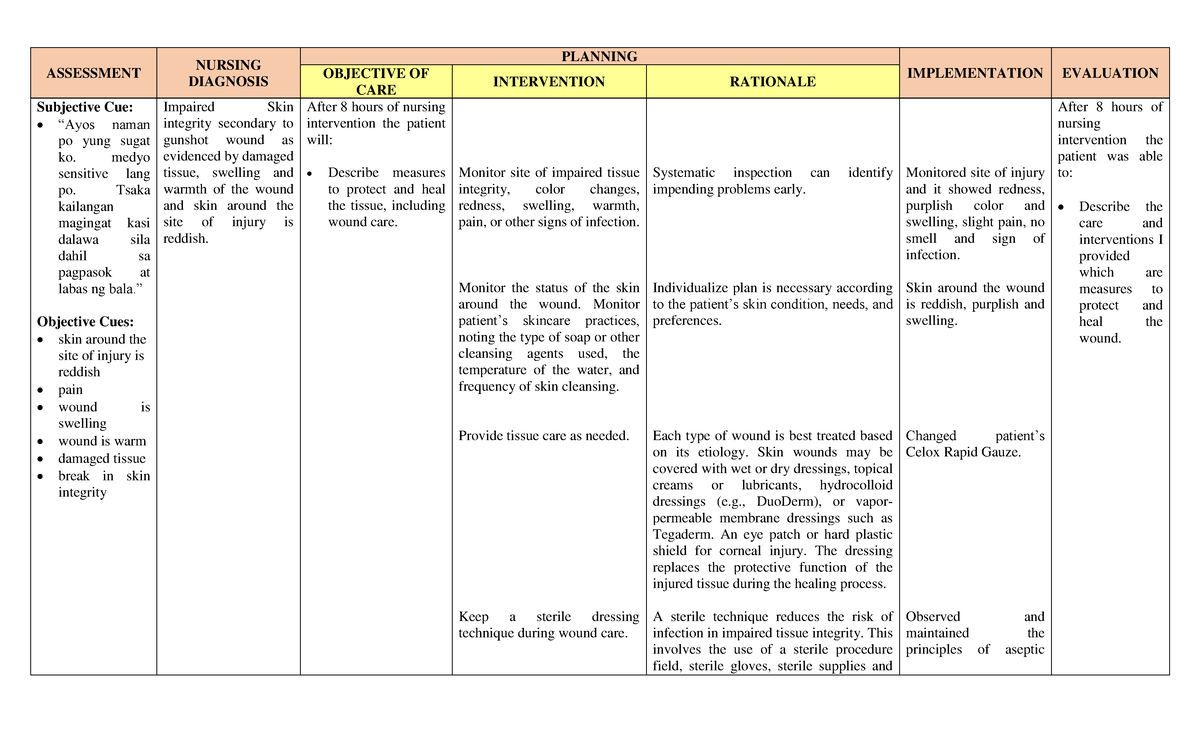
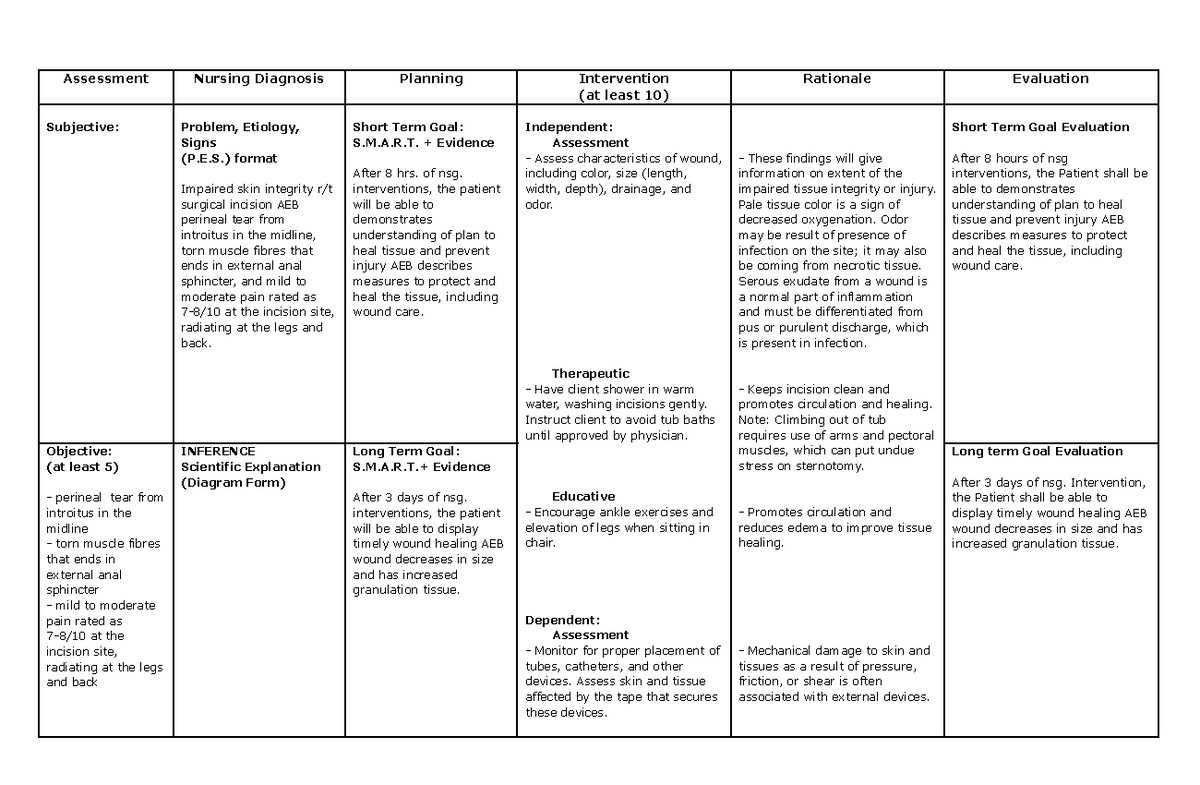
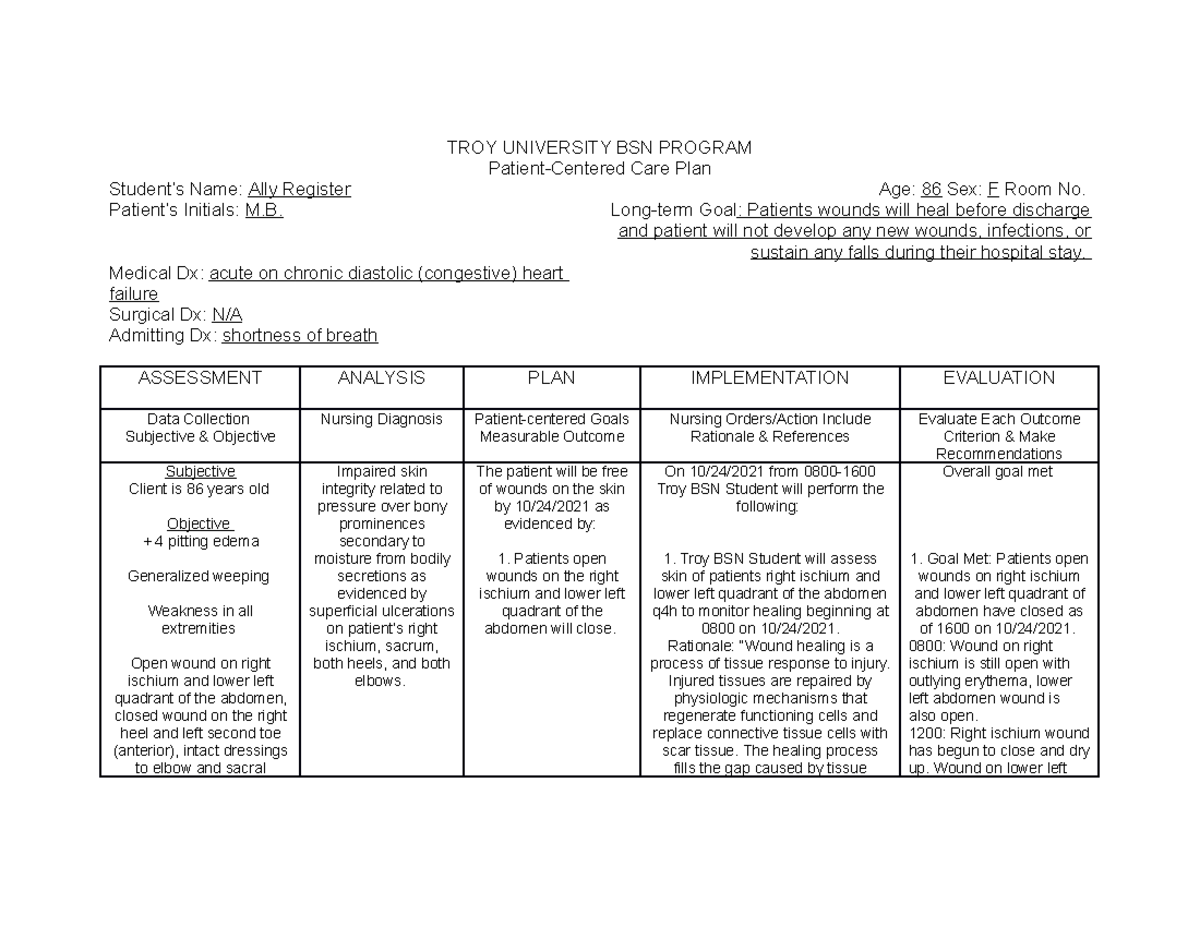
At its core, the care plan is a systematic assessment of a patient's vulnerability to skin damage. This involves evaluating factors like mobility, nutrition, hydration, sensory perception, moisture exposure, and overall health status, according to the National Pressure Injury Advisory Panel (NPIAP).
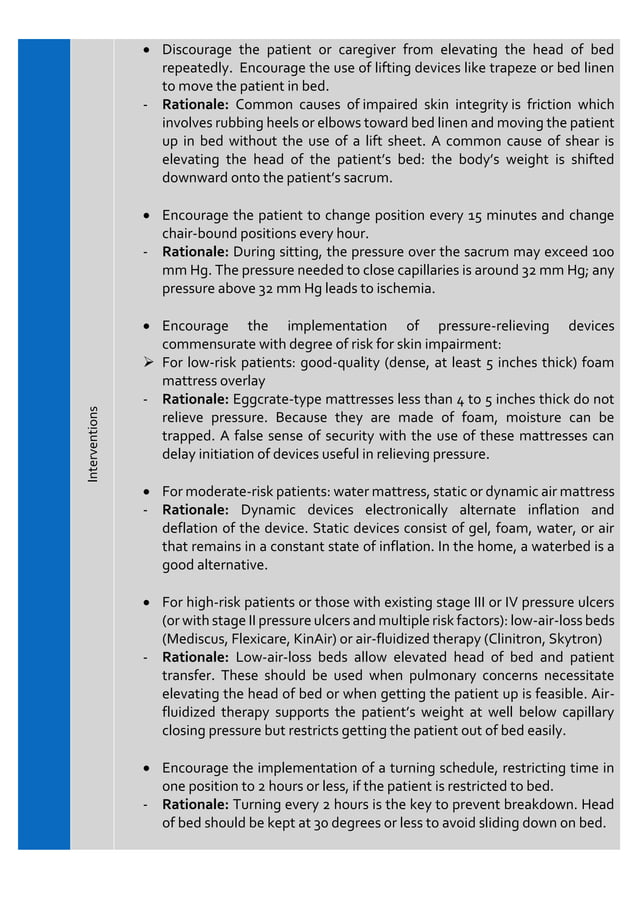
Based on this assessment, a personalized plan is developed to address identified risks. Interventions typically include regular skin inspections, pressure redistribution strategies, meticulous skin hygiene, and nutritional support.
The goal is to proactively manage these risk factors and prevent the development of pressure ulcers, also known as bedsores, and other skin-related complications.
Key Elements of the Care Plan
Several elements are crucial for the successful implementation of a Risk for Impaired Skin Integrity care plan.
Comprehensive Assessment
The foundation of the plan lies in a thorough and accurate assessment of the patient's risk factors. This assessment must be conducted upon admission and regularly reassessed throughout the patient's stay. This is outlined in guidance from the Centers for Medicare & Medicaid Services (CMS).
Tools like the Braden Scale are commonly used to standardize the assessment process and ensure consistency across different healthcare settings.
Pressure Redistribution
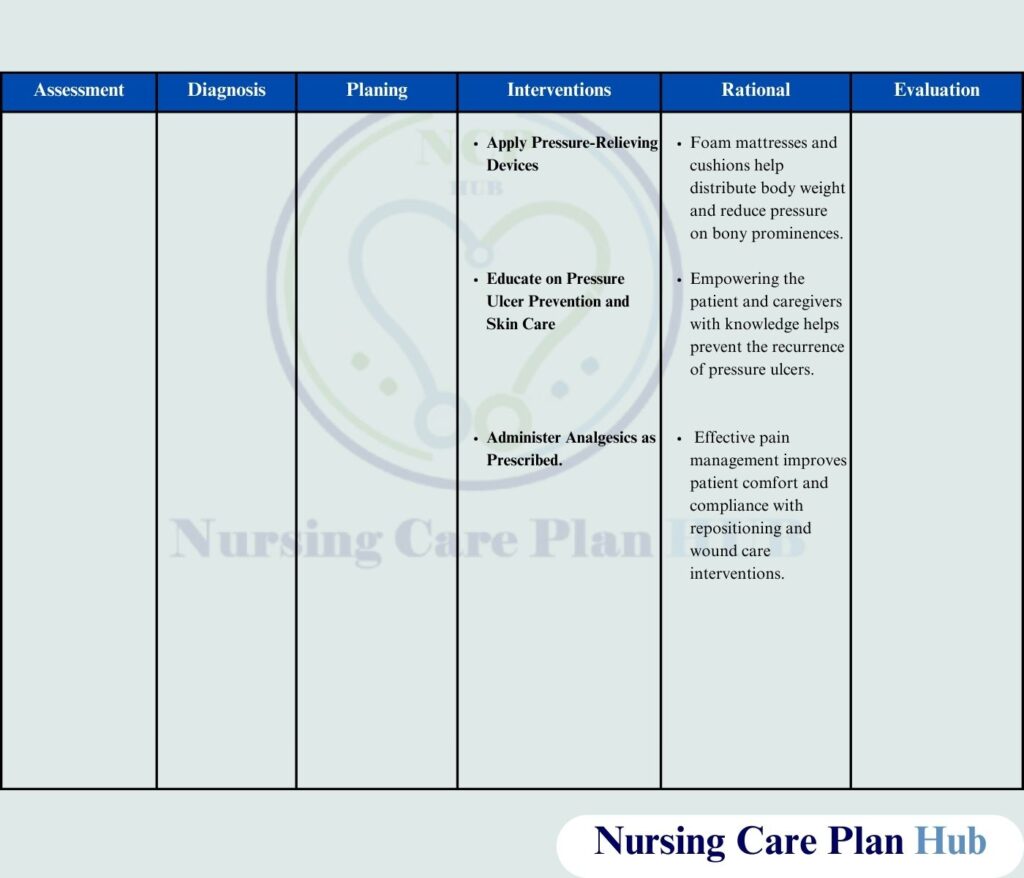
Reducing pressure on vulnerable areas of the body is a critical component of the plan. This often involves the use of specialized mattresses, cushions, and positioning devices. Repositioning patients at regular intervals, as frequently as every two hours, is also a crucial intervention.
Skin Hygiene and Moisture Management
Maintaining clean, dry skin is essential for preventing skin breakdown. This includes gentle cleansing with appropriate products and diligent moisture management to prevent maceration, which softens the skin and makes it more susceptible to damage.
Nutritional Support
Adequate nutrition and hydration are vital for maintaining skin integrity and promoting healing. Healthcare providers often consult with registered dietitians to develop individualized nutritional plans that meet the patient's specific needs.
Impact on Patients and Healthcare Facilities
The widespread adoption of the Risk for Impaired Skin Integrity care plan has the potential to significantly impact both patients and healthcare facilities.
For patients, the primary benefit is a reduced risk of developing painful and debilitating pressure ulcers. Effective prevention strategies can improve comfort, quality of life, and overall health outcomes.
Furthermore, patients experiencing skin breakdown can encounter extended hospital stays, infections, and surgical interventions, all of which impact their well-being.
For healthcare facilities, the care plan can lead to decreased healthcare costs associated with treating pressure ulcers. Treating existing ulcers is far more expensive than preventing them in the first place.
Additionally, reducing the incidence of pressure ulcers can improve patient satisfaction scores and minimize the risk of legal claims related to negligence.
Challenges and Future Directions
Despite the benefits, there are challenges associated with implementing the Risk for Impaired Skin Integrity care plan.
These include ensuring adequate staffing levels to provide consistent care, educating healthcare providers on best practices, and maintaining adherence to the plan's protocols.
The NPIAP also emphasizes the need for ongoing research to refine prevention strategies and develop new technologies to support skin integrity.
Moving forward, experts are exploring the use of telehealth and remote monitoring to provide personalized care and support to patients in their homes.
This approach can help extend the reach of the care plan and prevent skin breakdown in vulnerable populations beyond the confines of traditional healthcare settings.
The ongoing evolution of the Risk for Impaired Skin Integrity care plan reflects a growing recognition of the importance of proactive, patient-centered care.
By prioritizing prevention and addressing individual risk factors, healthcare providers can help protect patients from the devastating consequences of skin breakdown and promote overall well-being.