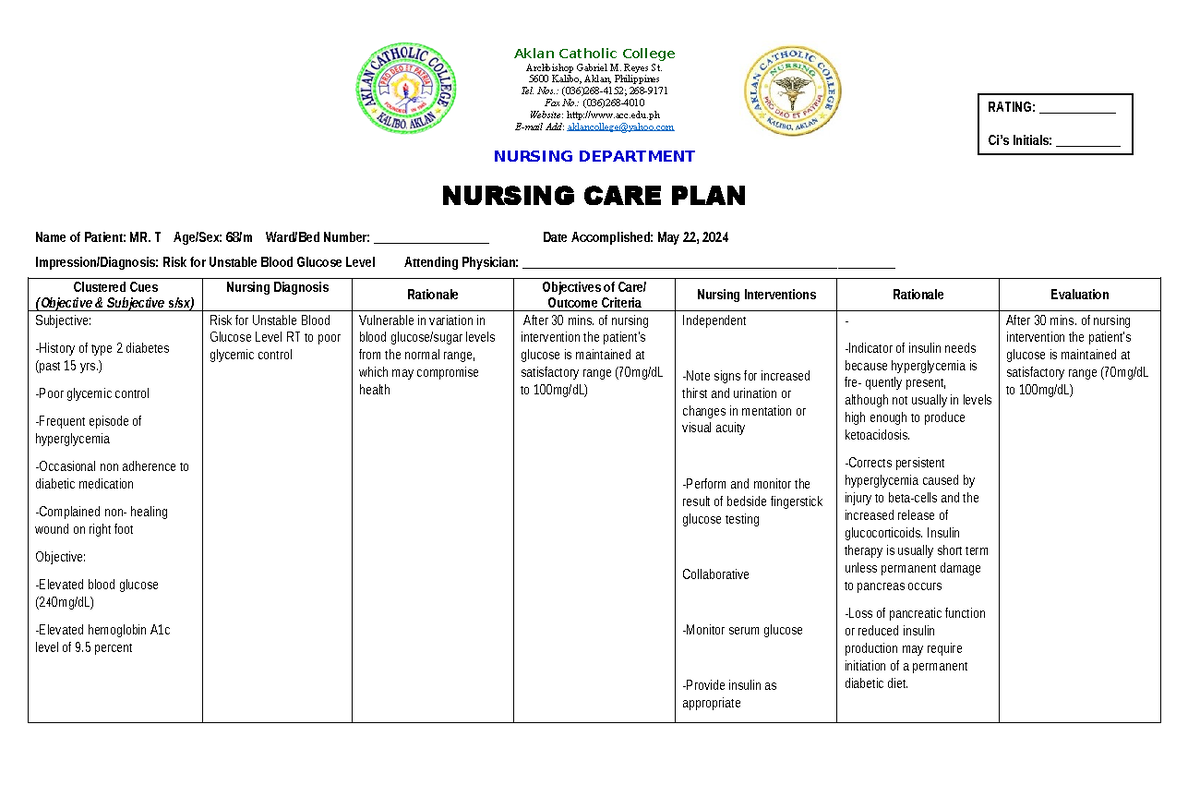
Risk For Unstable Blood Glucose Nursing Diagnosis

Hospitals nationwide are reporting a concerning rise in cases meeting the criteria for the nursing diagnosis, "Risk for Unstable Blood Glucose," particularly among patients with seemingly well-managed chronic conditions.
This surge highlights a potential systemic failure in current preventative strategies and necessitates immediate action to mitigate potentially life-threatening complications stemming from erratic blood sugar levels.
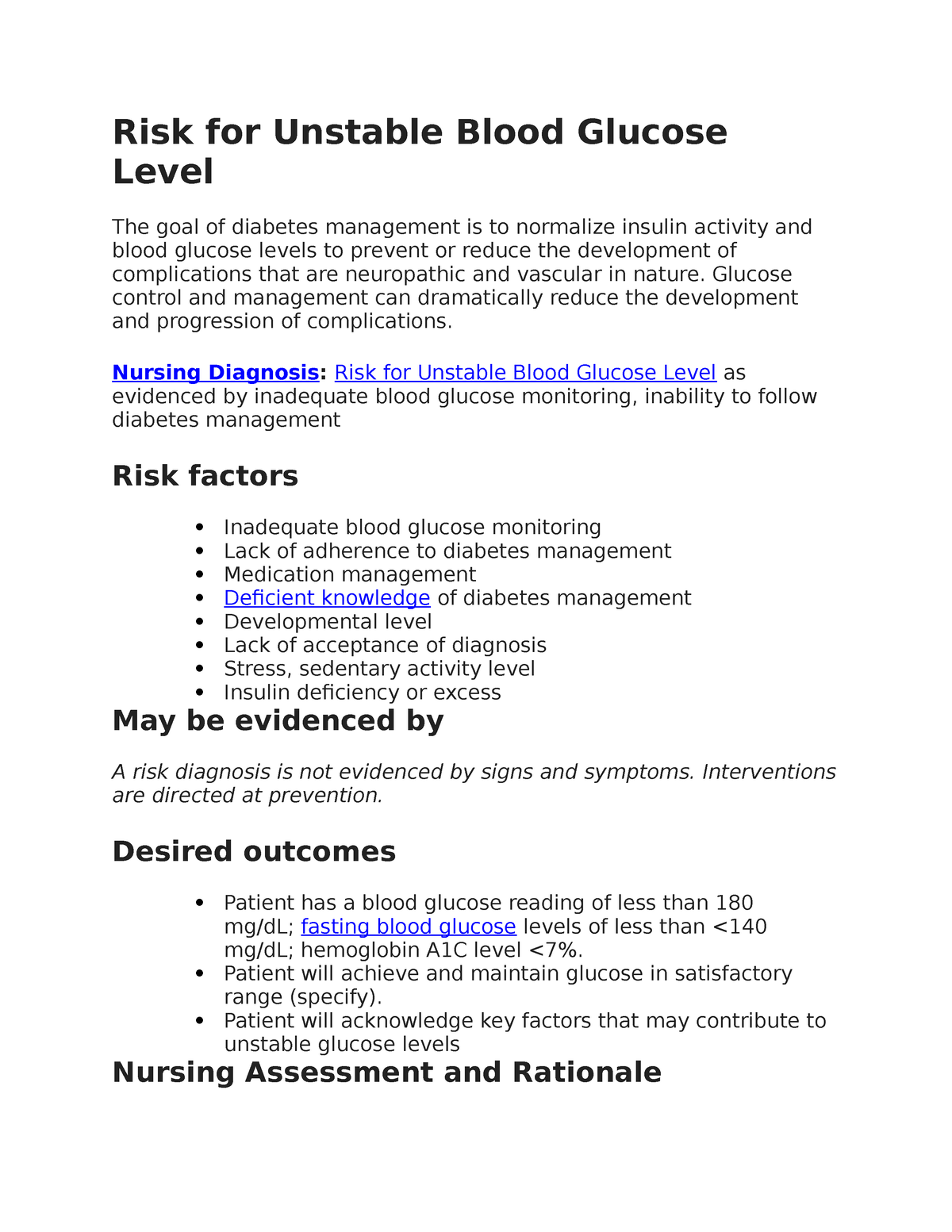
Alarming Increase in "Risk for Unstable Blood Glucose" Diagnoses
The American Nurses Association (ANA) reports a 15% increase in documented "Risk for Unstable Blood Glucose" nursing diagnoses across acute care settings in the past quarter. This alarming trend affects diverse patient populations, including those with previously stable Type 2 diabetes.
Dr. Emily Carter, a leading endocrinologist at Massachusetts General Hospital, stated, "We're seeing patients present with hyperglycemic and hypoglycemic episodes despite adherence to their prescribed medications and dietary plans."
This unanticipated instability poses a significant challenge to healthcare providers and demands a reevaluation of current preventative measures.
Contributing Factors Under Investigation
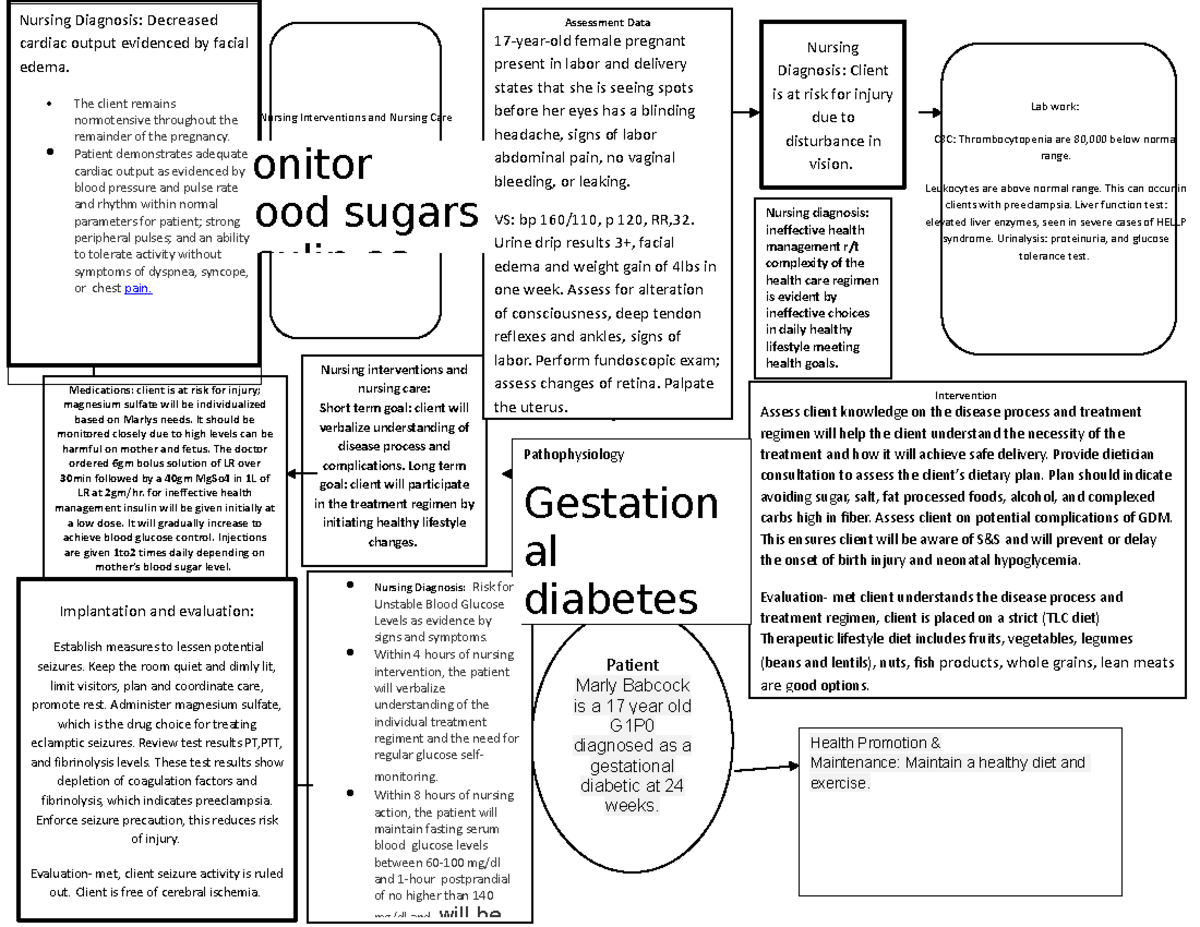
Initial investigations point towards a confluence of factors contributing to this growing problem. These include increased patient stress levels, medication interactions, and subtle changes in dietary habits, all potentially exacerbated by recent societal events.
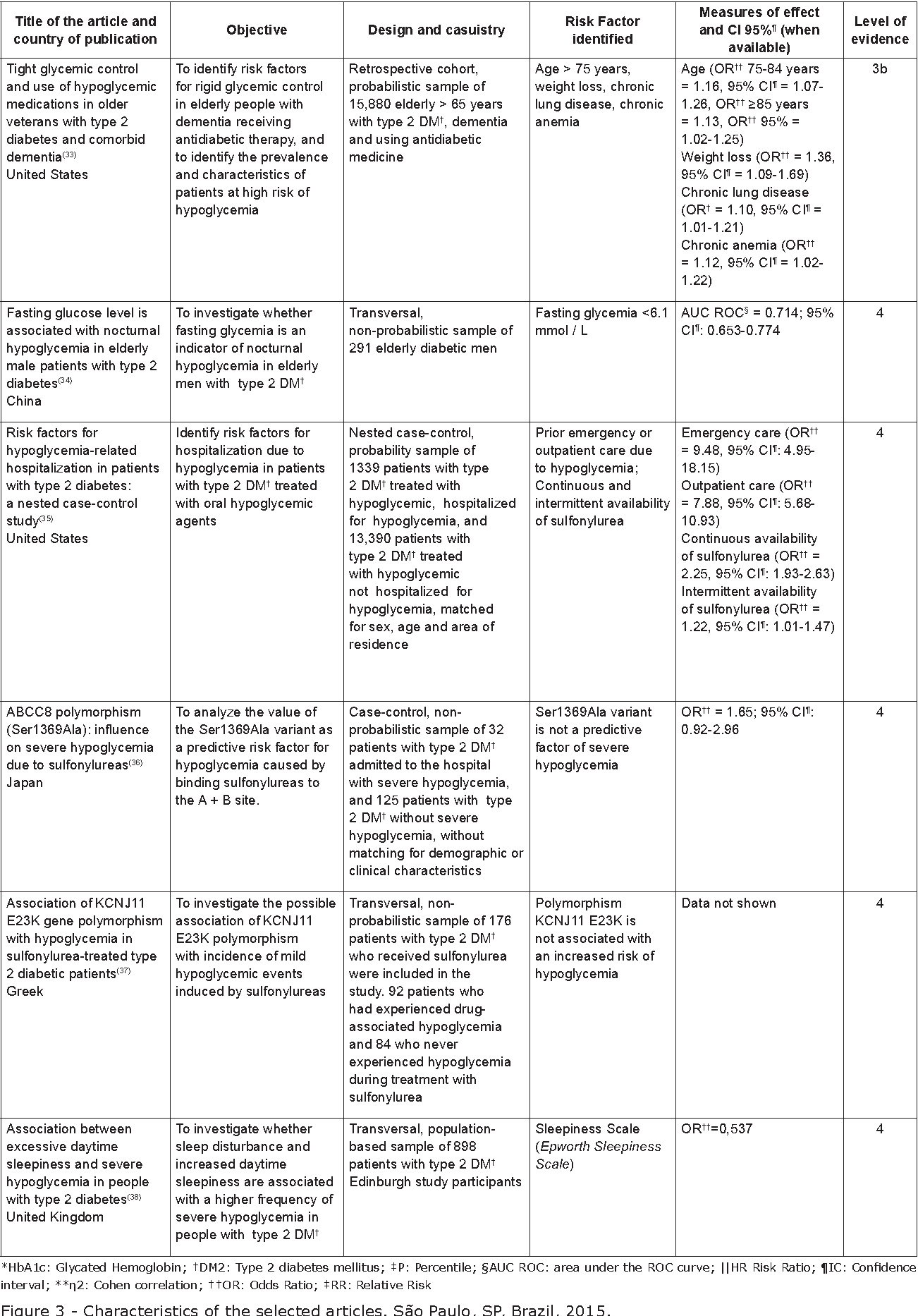
Preliminary data from a study conducted by the National Institutes of Health (NIH) suggests a correlation between heightened anxiety levels during the past year and increased blood glucose fluctuations.
The study emphasizes the crucial role of mental health in glycemic control, particularly in vulnerable populations.
Impact on Patient Outcomes
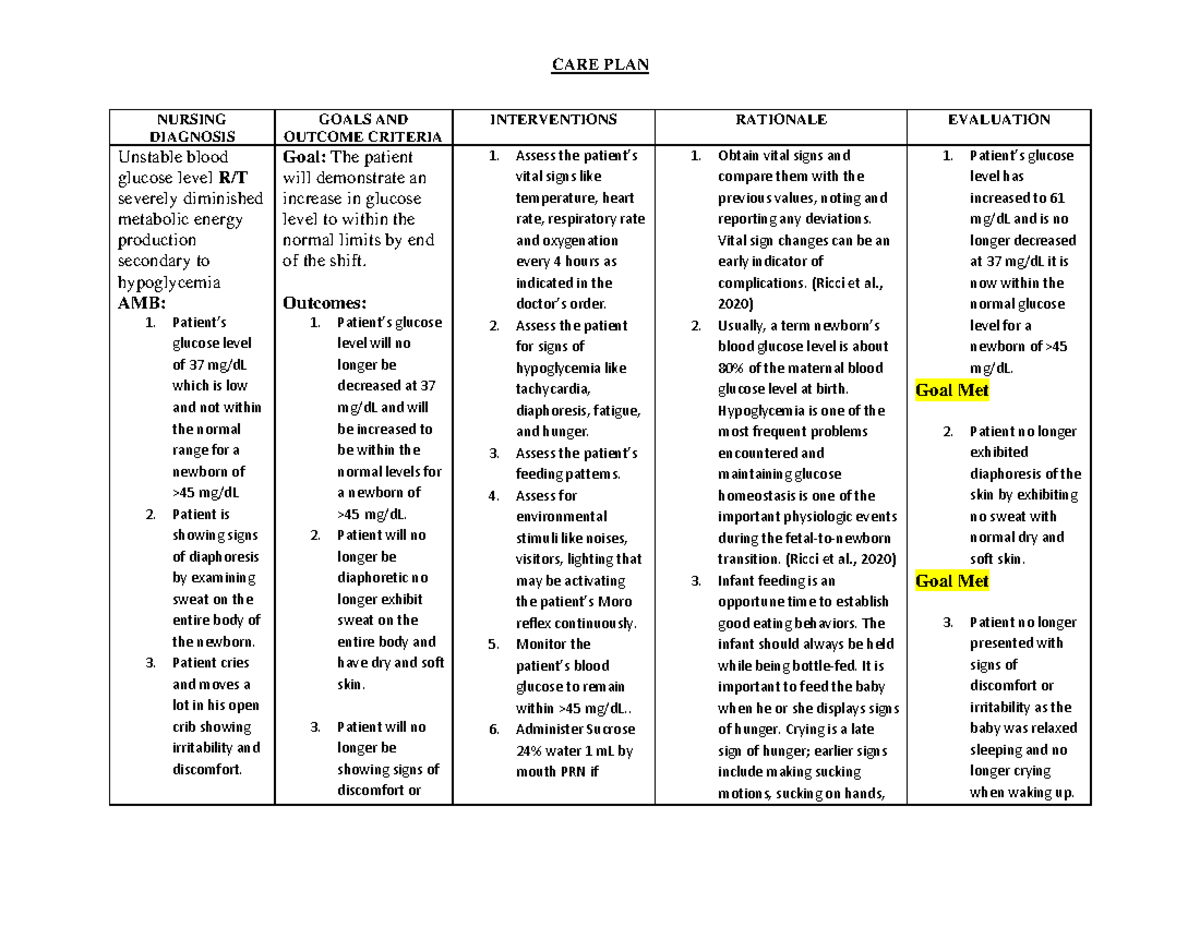
Unstable blood glucose levels can lead to a cascade of adverse health outcomes. These include increased risk of infection, delayed wound healing, and potential cardiovascular complications.
In severe cases, extreme fluctuations can result in diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), both requiring intensive medical intervention.
The rise in "Risk for Unstable Blood Glucose" diagnoses directly translates to increased hospital readmission rates and a greater burden on healthcare resources.
Revised Nursing Protocols and Intervention Strategies
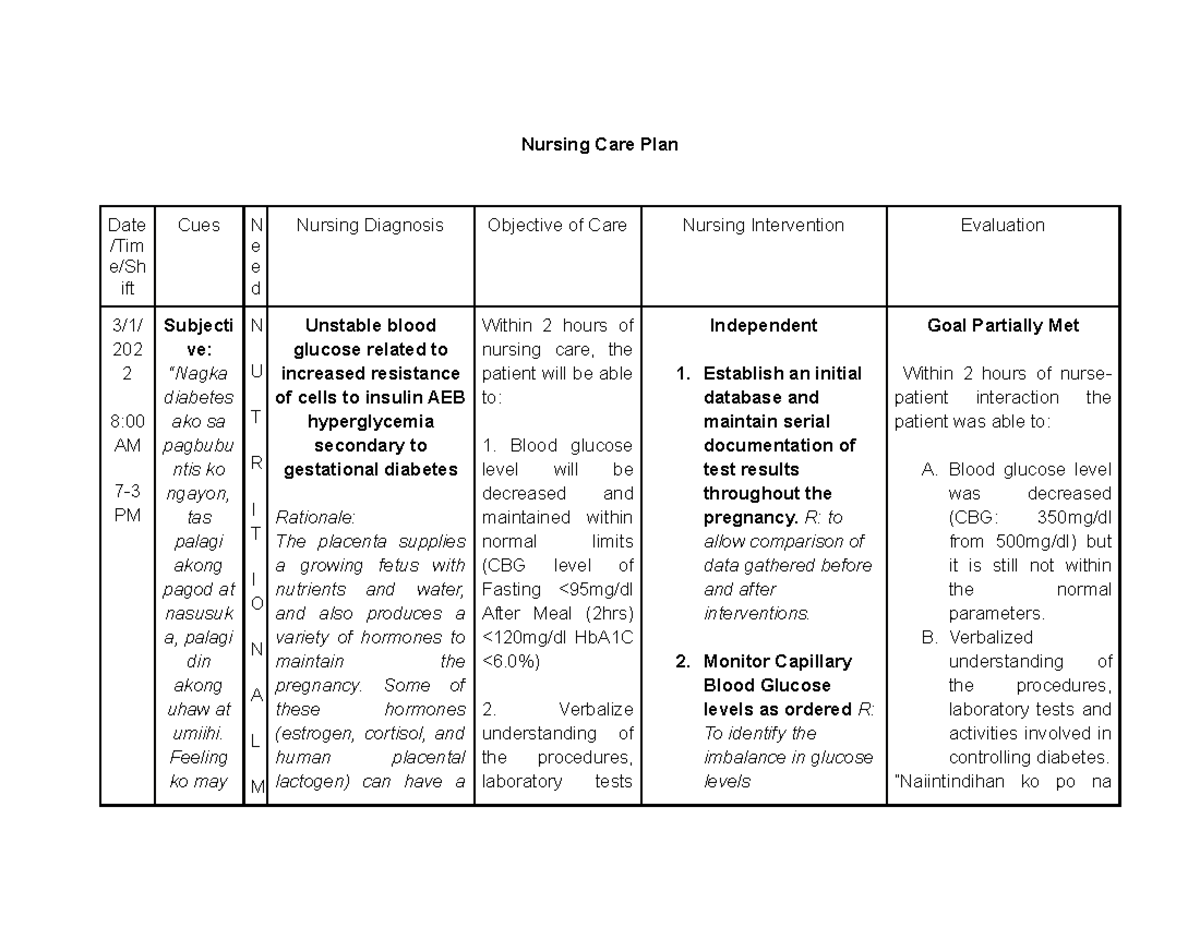
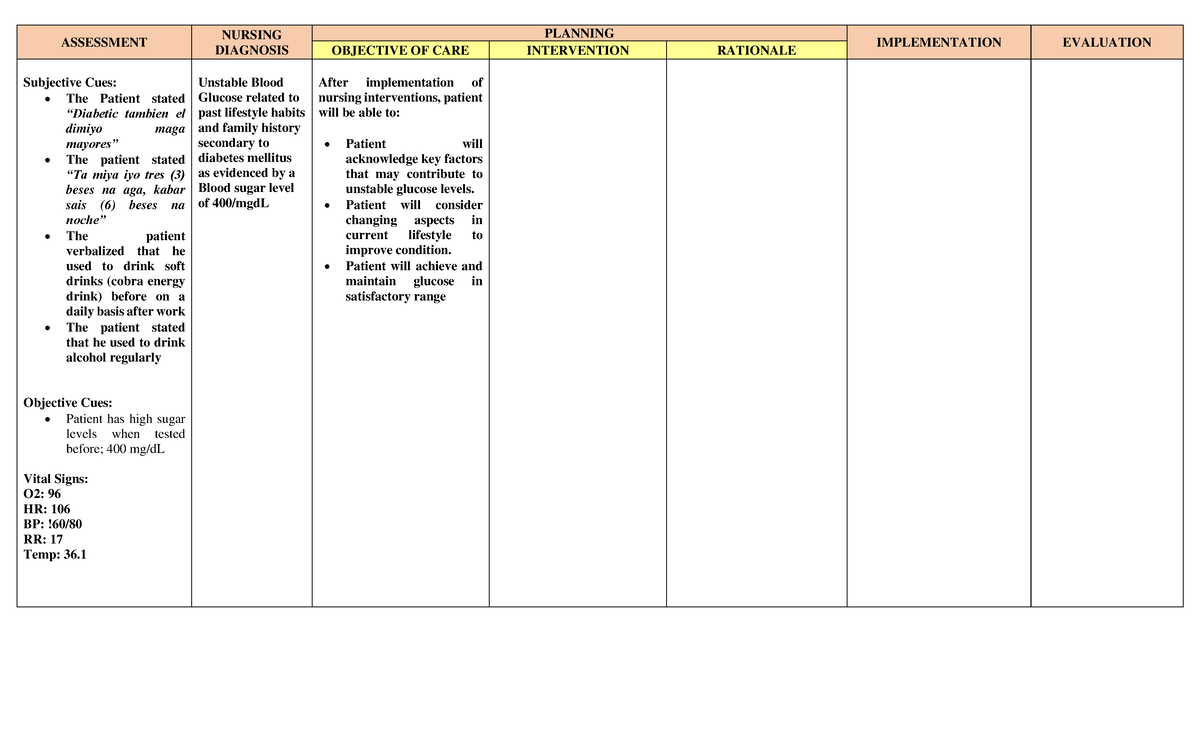
In response to the escalating crisis, several hospitals are implementing revised nursing protocols. These include more frequent blood glucose monitoring, enhanced patient education, and individualized care plans tailored to address specific risk factors.
Johns Hopkins Hospital has implemented a new algorithm for insulin administration based on continuous glucose monitoring (CGM) data, showing promising results in stabilizing blood sugar levels.
Sarah Johnson, RN, a diabetes educator at UCLA Medical Center, emphasizes the importance of patient empowerment. "We need to equip patients with the knowledge and skills to proactively manage their blood glucose levels at home."
The Role of Technology in Monitoring and Management
The integration of technology, particularly continuous glucose monitoring (CGM) systems and telemedicine, is gaining traction. These tools provide real-time data and facilitate remote monitoring, enabling timely interventions to prevent severe fluctuations.
Many healthcare providers are now advocating for wider access to CGM technology, especially for individuals at high risk of developing unstable blood glucose levels.
However, concerns regarding data privacy and affordability remain significant barriers to widespread adoption.
Call to Action for Healthcare Professionals
Healthcare professionals are urged to remain vigilant in identifying patients at risk for unstable blood glucose. A thorough assessment of risk factors, including medication history, lifestyle factors, and mental health status, is crucial.
Open communication with patients and collaboration among healthcare team members are essential for developing and implementing effective management strategies.
Furthermore, increased funding for research on innovative approaches to glycemic control is needed to address this growing public health concern.
Next Steps and Ongoing Developments
The Centers for Disease Control and Prevention (CDC) is currently collaborating with the ANA and other stakeholders to develop national guidelines for the prevention and management of unstable blood glucose.
A summit on "Risk for Unstable Blood Glucose" is scheduled for next month in Washington, D.C., bringing together experts from various disciplines to discuss strategies for addressing this critical issue.
Ongoing research is focused on identifying genetic and environmental factors that contribute to glucose dysregulation, paving the way for personalized interventions and preventative strategies.