Seroma After Inguinal Hernia Repair With Mesh

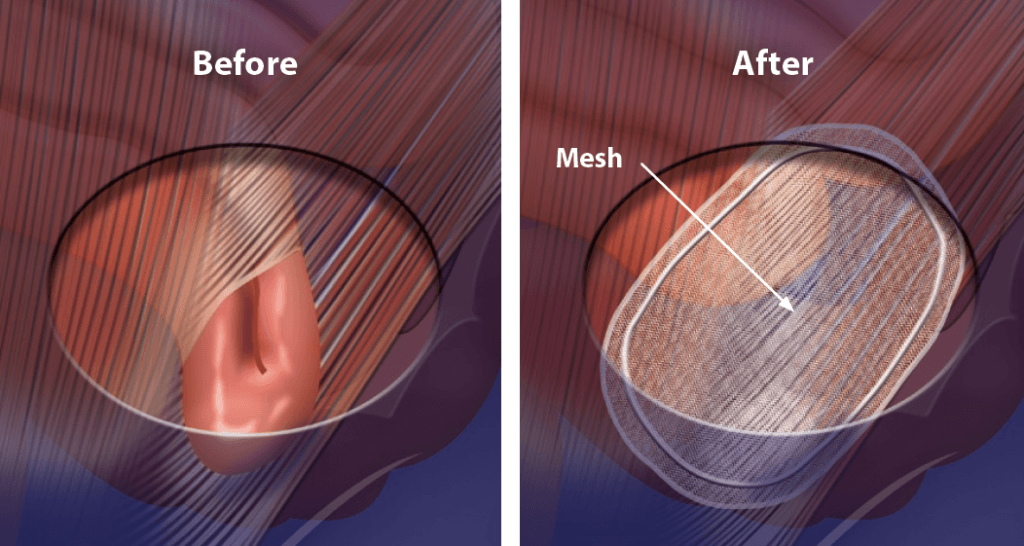
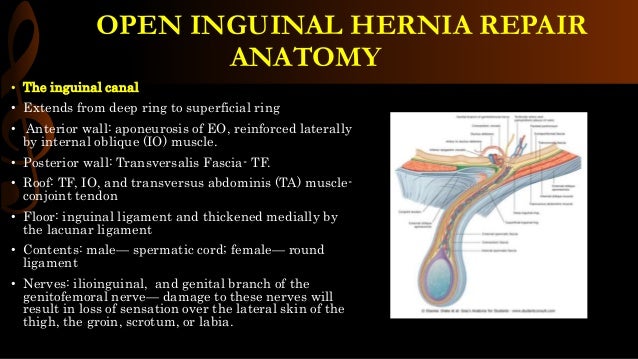
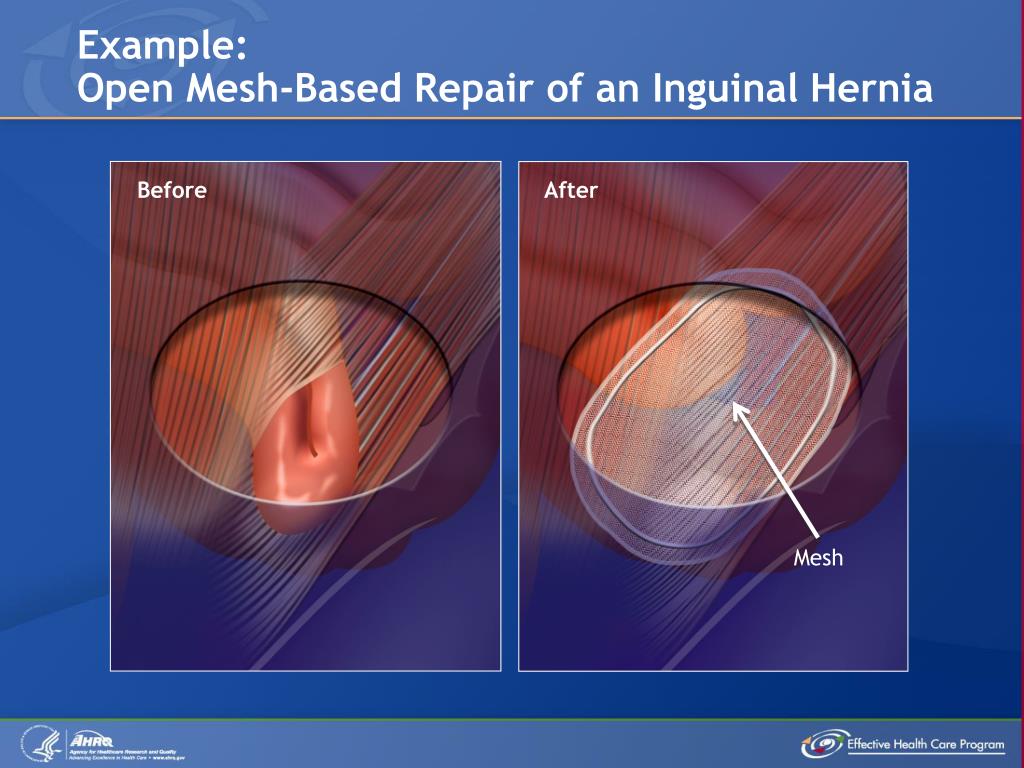
Inguinal hernia repair, a common surgical procedure, often utilizes mesh to strengthen the abdominal wall. However, a potential complication, seroma formation, can arise post-operatively, causing patient discomfort and potentially requiring further intervention.
This article examines the incidence, management, and potential impact of seromas following inguinal hernia repair with mesh, drawing on surgical literature and expert insights. Understanding this complication is crucial for both surgeons and patients.
What is a Seroma?
A seroma is a collection of serous fluid that develops under the skin, typically at the surgical site.
Following inguinal hernia repair with mesh, the body's inflammatory response can lead to fluid accumulation in the space created during the dissection and mesh placement.
The fluid is usually clear or slightly yellow and consists of plasma and inflammatory cells.
Incidence and Risk Factors
The reported incidence of seroma formation after inguinal hernia repair with mesh varies in the literature.
Studies suggest rates ranging from 3% to over 20%, influenced by factors such as surgical technique, mesh type, and patient characteristics. Some studies even suggests lower or higher percentages, depending on the variables.
Risk factors may include larger hernia size, extensive dissection, lymphatic disruption during surgery, and patient-specific factors like obesity or use of antiplatelet medications.
Diagnosis and Symptoms
Seromas typically present as a soft, fluctuant swelling at the surgical site.
Patients may experience discomfort, pressure, or a feeling of fullness in the groin area.
Diagnosis is often clinical, based on physical examination. Ultrasound imaging can be used to confirm the presence of fluid collection and rule out other complications such as hematoma or infection. Sometimes a needle aspiration might be required for confirmation.
Management Strategies
Many seromas are small and resolve spontaneously without intervention.
Conservative management includes observation, pain control with over-the-counter medications, and wearing supportive underwear.
Larger, symptomatic seromas may require aspiration (needle drainage) to relieve pressure and discomfort. Multiple aspirations might be needed.
When is Surgical Intervention Necessary?
Surgical intervention is rarely required, but may be considered for persistent, symptomatic seromas that do not respond to aspiration or if infection is suspected.
In such cases, surgical drainage and possible mesh removal might be necessary.
The decision to surgically intervene is made on a case-by-case basis, weighing the benefits and risks.
Prevention Strategies
Surgeons employ various techniques to minimize the risk of seroma formation.
These include meticulous surgical technique to minimize tissue trauma, careful ligation of lymphatic vessels, and avoiding excessive dead space during closure.
Some surgeons advocate for the use of fibrin sealant or other hemostatic agents to reduce fluid accumulation. The use of certain types of mesh may also reduce the possibility of seroma.
Impact on Patients and Recovery
Seroma formation can prolong the recovery period and impact a patient's quality of life.
While most seromas are benign and self-limiting, they can cause anxiety and discomfort.
Patients should be educated about the possibility of seroma formation and instructed on how to monitor their surgical site for signs of complications. Proper wound care is crucial for healing.
Expert Perspectives
Dr. Emily Carter, a general surgeon specializing in hernia repair, emphasizes the importance of patient education. "Informing patients about the possibility of seroma formation helps manage their expectations and encourages early reporting of any concerning symptoms," she stated.
Dr. David Lee, a leading researcher in surgical mesh technology, notes, "Ongoing research focuses on developing mesh materials that minimize inflammatory response and reduce the risk of post-operative complications, including seromas."
According to the American College of Surgeons, a comprehensive understanding of potential complications is essential for optimal patient outcomes following inguinal hernia repair.
Looking Ahead
Continued research and innovation in surgical techniques and mesh technology are aimed at minimizing the incidence of seroma formation.
Focus on personalized surgical approaches and patient-specific risk assessment will further improve outcomes.
Efforts to raise patient awareness and improve post-operative management strategies are crucial for addressing this common complication.
"Seroma formation is a recognized complication, but proactive management and patient education can mitigate its impact," says Dr. Sarah Chen, a prominent hernia specialist.
By staying informed and working closely with their healthcare providers, patients undergoing inguinal hernia repair can navigate this potential challenge effectively. Early detection and prompt management are key to a smooth recovery.