Stool Sample Tests To Boost Hospital Revenue
Hospitals nationwide are aggressively expanding stool sample testing programs, a move projected to significantly increase revenue streams amidst tightening budgets.
This rapid adoption of advanced diagnostic tools for gastrointestinal (GI) conditions promises faster and more accurate diagnoses, but also raises concerns about potential overutilization and cost implications for patients and insurers.
Explosion in Stool Testing: The New Gold Rush?
Data reveals a surge in hospital-based stool testing, particularly for C. difficile infections, inflammatory bowel disease (IBD), and colorectal cancer screening. This trend is fueled by technological advancements and the perceived need to improve diagnostic accuracy.
According to a recent report by Kalorama Information, the market for stool-based diagnostics is projected to reach $4 billion by 2025. This indicates a substantial financial incentive for hospitals to invest in and promote these tests.
Who is Benefiting?
Hospitals stand to gain the most from increased stool sample testing. This includes enhanced revenue through direct billing for tests and downstream revenue from related treatments and procedures.
Diagnostic companies producing advanced testing kits are also experiencing a boom. Specific companies like Exact Sciences and BioMerieux are seeing increased demand for their products.
What Tests are Being Implemented?
The most common tests being implemented are PCR-based assays for infectious diseases. These tests offer rapid and highly sensitive detection of pathogens like C. difficile.
Fecal immunochemical tests (FIT) for colorectal cancer screening are also gaining popularity. These tests are non-invasive and can detect hidden blood in the stool, indicating the presence of polyps or cancer.
Where is this Happening?
This trend is observable across hospitals of all sizes throughout the United States. Major academic medical centers and community hospitals alike are expanding their stool testing capabilities.
Regional variations in testing practices are emerging. Some states have implemented stricter guidelines for antibiotic use and C. difficile testing, potentially influencing the demand for these tests.
When Did This Trend Start?
The significant increase in stool sample testing has been observed over the past five years. This is largely due to the availability of more sophisticated and user-friendly testing platforms.
The COVID-19 pandemic may have indirectly accelerated this trend. Hospitals prioritized diagnostic testing and invested in infrastructure that could be repurposed for stool sample analysis.
How Are These Tests Performed?
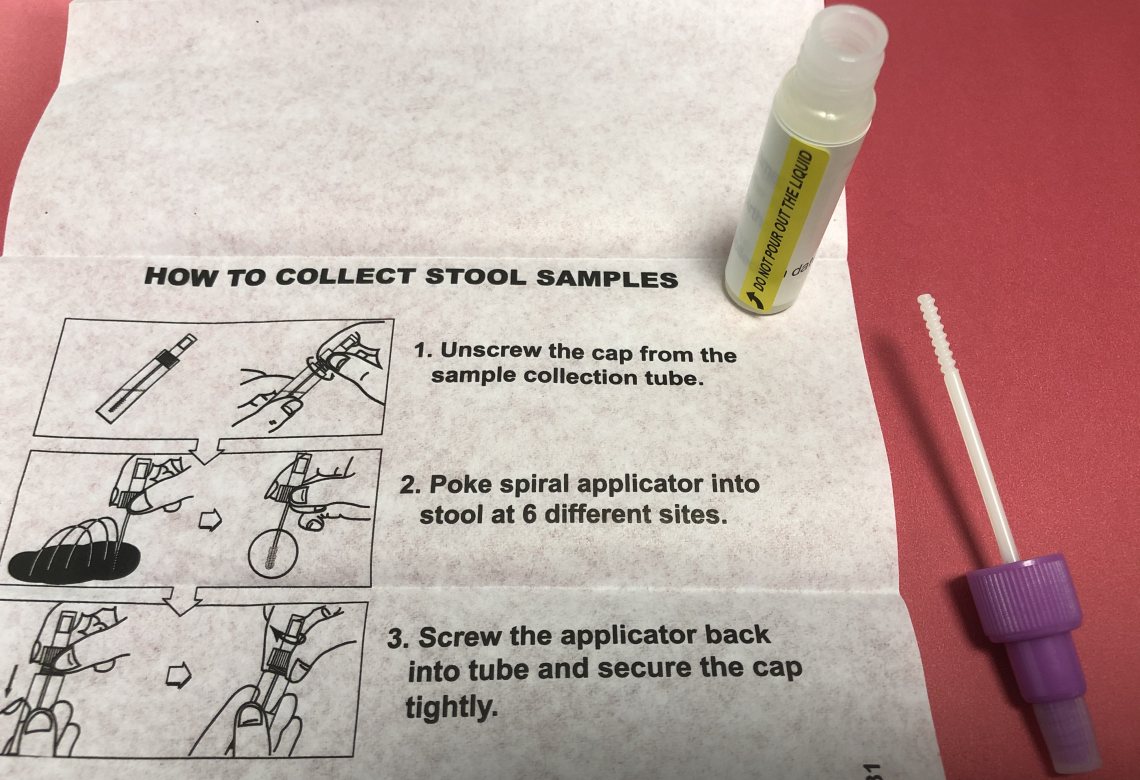
Patients typically collect stool samples at home using a provided kit. The samples are then sent to the hospital laboratory for analysis.
Advanced molecular techniques, like PCR, are used to identify specific pathogens or biomarkers. Laboratory technicians play a crucial role in ensuring the accuracy and reliability of the results.
Concerns and Potential Pitfalls
Increased stool testing raises concerns about potential overutilization. Unnecessary testing can lead to increased healthcare costs and patient anxiety.
The accuracy and clinical utility of some newer stool tests remain a subject of debate. Clinicians must carefully interpret the results in the context of the patient's overall clinical picture.
The increased volume of testing could strain laboratory resources. Hospitals must ensure that they have adequate staffing and equipment to handle the increased workload.
"We need to be vigilant about ensuring that these tests are used appropriately and that patients are receiving the best possible care," stated Dr. Emily Carter, Chief of Gastroenterology at a major hospital system.
There's also worry for the patient's wallet. Cost of stool sample tests vary widely, and patients could face unexpected bills if their insurance coverage is limited.
Next Steps and Ongoing Developments
Healthcare policymakers are closely monitoring the trend in stool sample testing. They will be assessing the impact on healthcare costs and patient outcomes.
Professional medical societies are developing guidelines for the appropriate use of stool tests. These guidelines aim to promote evidence-based practice and reduce unnecessary testing.
Ongoing research is focused on developing even more accurate and cost-effective stool-based diagnostic tools. This research could further transform the landscape of GI diagnostics.
Further analysis of the long-term effects of increased stool sample testing is warranted. This analysis should include assessment of patient outcomes, healthcare costs, and laboratory resource utilization.