Sympathetic Nervous System And Blood Pressure

The silent surge of stress, the body's unseen alarm system, is increasingly recognized as a key player in the global hypertension epidemic. Millions unknowingly walk a tightrope, their sympathetic nervous system (SNS) subtly elevating their blood pressure, inching them closer to cardiovascular disease. The intricate dance between stress response and blood pressure regulation is now under intense scrutiny, prompting new research and potential therapeutic avenues.
This article delves into the complex interplay between the SNS and blood pressure, examining the mechanisms involved, the health implications, and the emerging strategies for managing this critical connection. Understanding this relationship is crucial for both healthcare professionals and individuals seeking to proactively safeguard their cardiovascular health.
The Sympathetic Nervous System: Your Body's Alarm
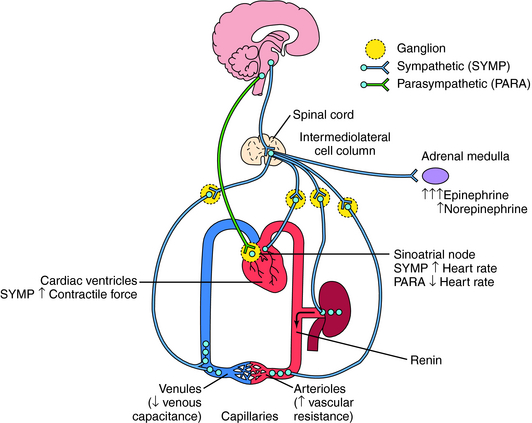
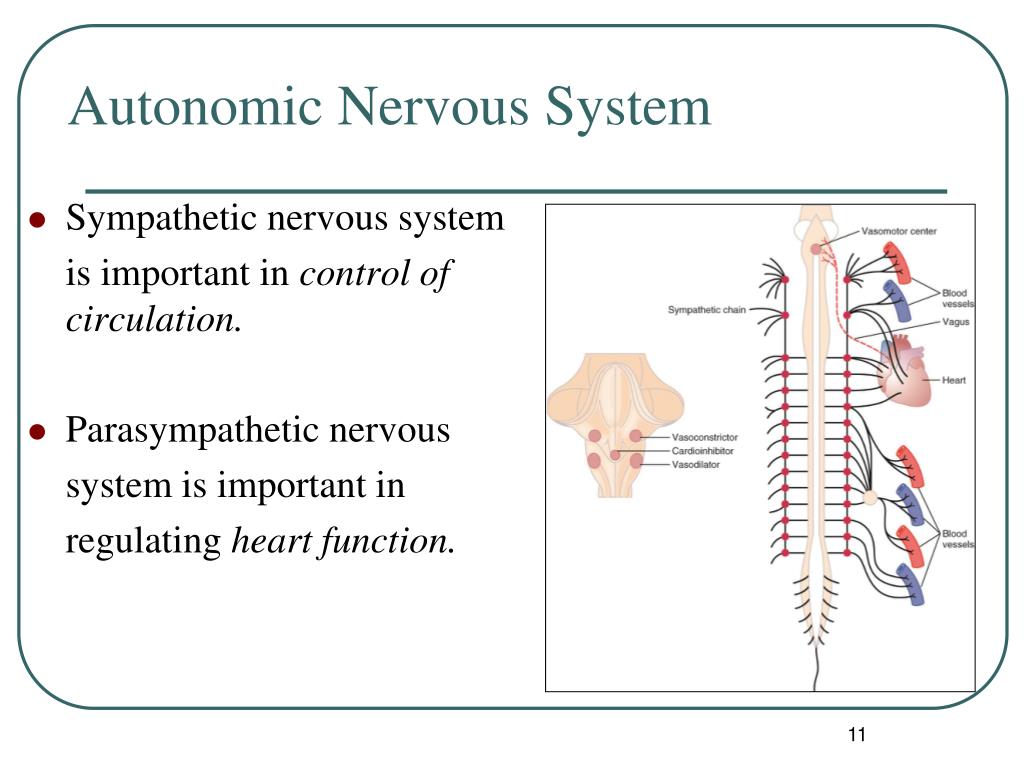
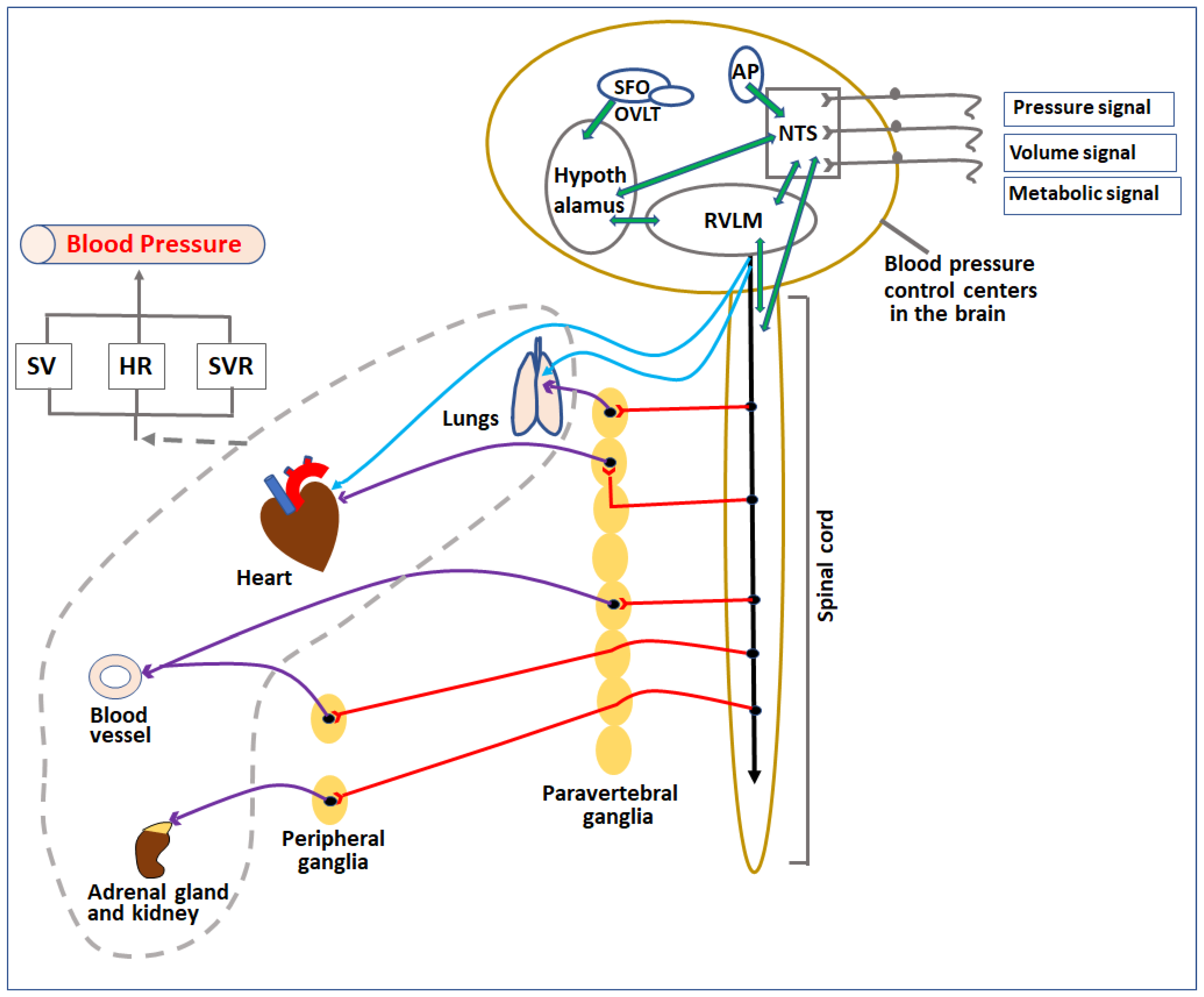
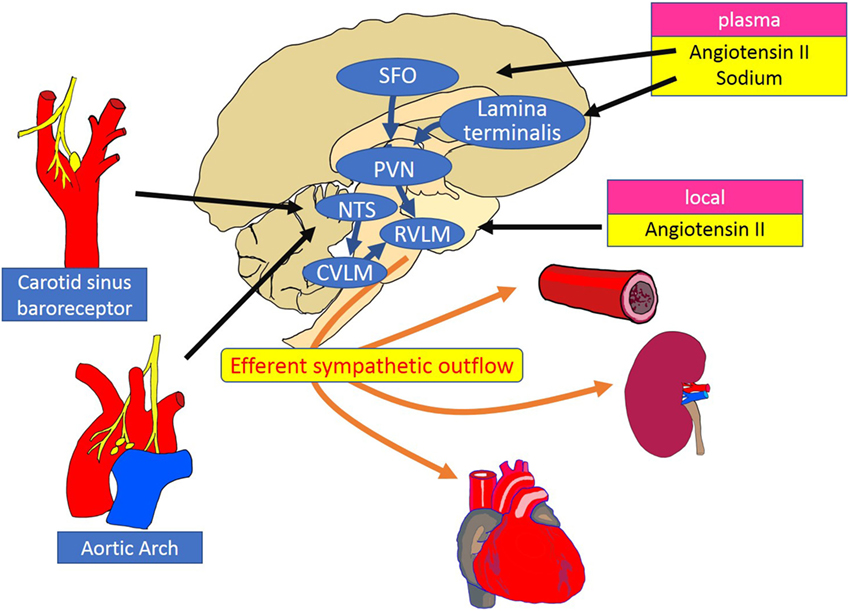
The SNS is a crucial component of the autonomic nervous system, responsible for the body's "fight-or-flight" response. It's designed to protect us from immediate threats by preparing the body for action.
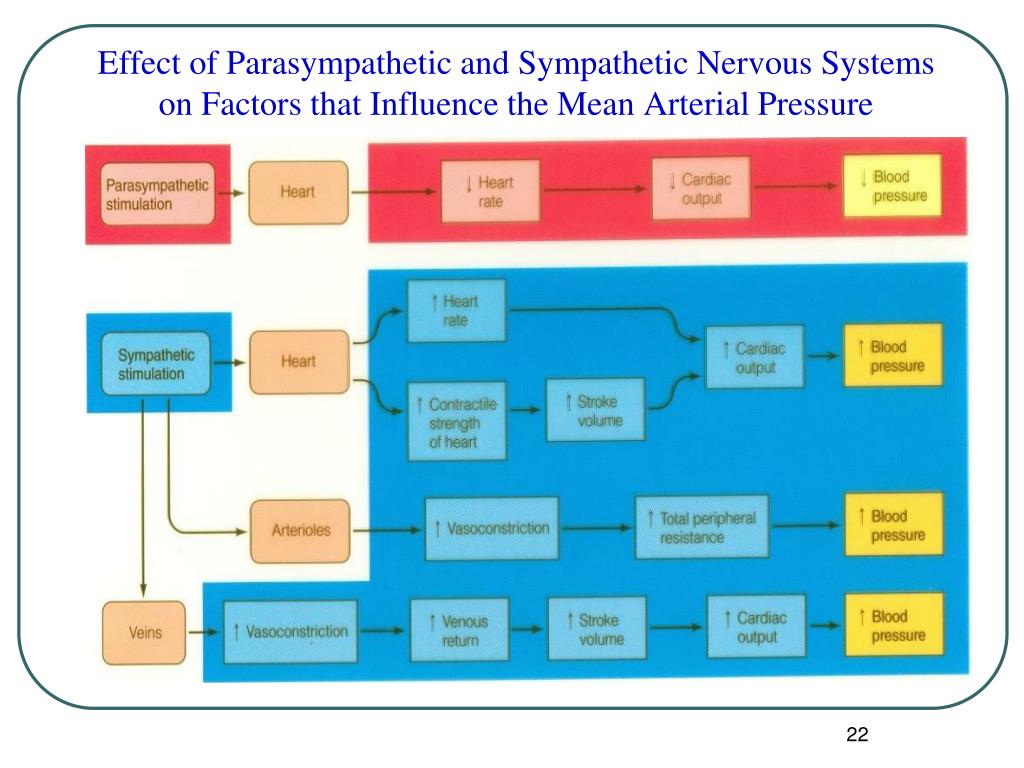
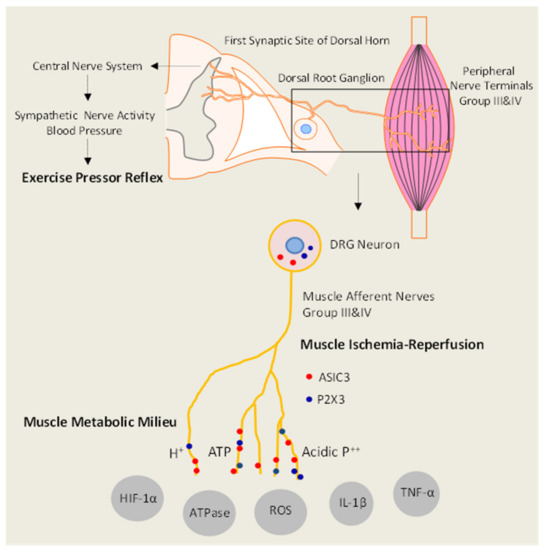
This system kicks into gear by releasing hormones like adrenaline and noradrenaline, causing a cascade of physiological changes. These include increased heart rate, faster breathing, and, importantly, constricted blood vessels.
The blood vessel constriction raises blood pressure, ensuring that muscles receive the oxygen and nutrients they need to escape danger or confront a challenge. While essential for acute survival, chronic activation of the SNS can have detrimental effects on cardiovascular health.
The Link to Blood Pressure: A Delicate Balance Disrupted
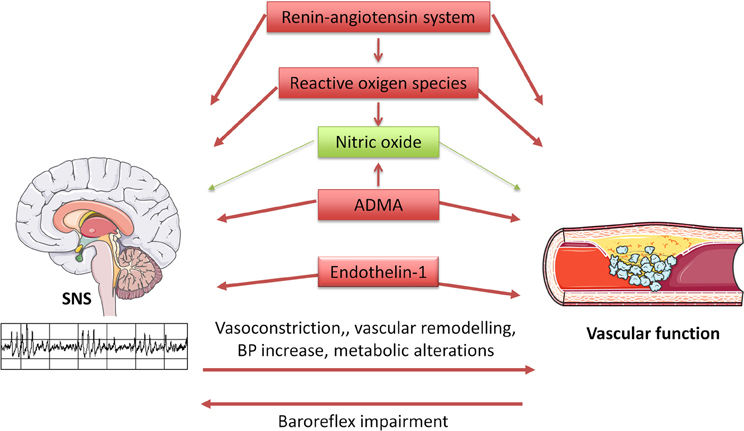
When the SNS is constantly activated, either by chronic stress, anxiety, or underlying medical conditions, the sustained release of adrenaline and noradrenaline can lead to persistent elevation of blood pressure. This is where the danger lies.
Hypertension, or high blood pressure, puts excessive strain on the heart and blood vessels. Over time, this can damage the heart, kidneys, brain, and eyes, significantly increasing the risk of heart attack, stroke, and other life-threatening conditions.
Dr. Anya Sharma, a leading cardiologist at the National Heart Institute, emphasizes, "The sympathetic nervous system is not just a responder to stress; it's an active regulator of blood pressure. Chronic activation can reprogram the body's blood pressure set point, leading to sustained hypertension, even in the absence of immediate stress."
Factors Influencing SNS Activity and Blood Pressure
Several factors can influence SNS activity and, consequently, blood pressure. Lifestyle choices play a significant role.
Poor diet, lack of exercise, smoking, and excessive alcohol consumption can all contribute to increased SNS activity and elevated blood pressure. Stress, both acute and chronic, is a well-established trigger.
Genetic predisposition also matters. Some individuals are genetically more susceptible to overactivity of the SNS in response to stressors, making them more prone to developing hypertension.
Underlying medical conditions, such as sleep apnea, thyroid disorders, and kidney disease, can also contribute to SNS activation and high blood pressure. Certain medications can also have a similar effect.
Identifying the Role of the SNS in Hypertension
Determining the extent to which the SNS contributes to an individual's hypertension can be challenging. Traditional blood pressure measurements only provide a snapshot in time.
Ambulatory blood pressure monitoring (ABPM), which measures blood pressure at regular intervals over a 24-hour period, can offer a more comprehensive picture. This can help identify patterns of blood pressure variability and detect "white coat hypertension," where blood pressure is elevated only in a clinical setting.
More advanced techniques, such as measuring plasma catecholamine levels (adrenaline and noradrenaline), can provide direct evidence of increased SNS activity. However, these tests are not routinely performed.
Management Strategies: Calming the Nervous System
Managing hypertension related to SNS overactivity involves a multifaceted approach. Lifestyle modifications are often the first line of defense.
Regular exercise, a healthy diet low in sodium and saturated fat, smoking cessation, and moderate alcohol consumption can all help lower blood pressure and reduce SNS activity. Stress management techniques, such as mindfulness meditation, yoga, and deep breathing exercises, can also be highly effective.
In some cases, medications may be necessary to control blood pressure. Beta-blockers, for example, work by blocking the effects of adrenaline and noradrenaline on the heart and blood vessels, reducing heart rate and blood pressure.
Other medications, such as alpha-blockers and central alpha agonists, can also help lower blood pressure by reducing SNS activity. However, medication choices should always be made in consultation with a healthcare professional.
Emerging Therapies and Future Directions
Research is ongoing to develop new and more targeted therapies for managing hypertension related to SNS overactivity. One promising area is renal denervation, a minimally invasive procedure that uses radiofrequency energy or ultrasound to disrupt the nerves in the renal arteries, which play a key role in regulating blood pressure.
Studies have shown that renal denervation can significantly lower blood pressure in some patients with resistant hypertension, meaning hypertension that is difficult to control with medication. However, the long-term efficacy and safety of renal denervation are still being evaluated.
Another area of research is focused on developing drugs that specifically target the SNS without causing unwanted side effects. Personalized medicine, tailoring treatment to an individual's specific genetic and physiological profile, is also gaining traction.
The Takeaway: Proactive Management is Key
The link between the sympathetic nervous system and blood pressure is undeniable. Understanding this connection is crucial for preventing and managing hypertension.
By adopting healthy lifestyle habits, managing stress effectively, and working closely with healthcare professionals, individuals can take proactive steps to calm their nervous system and safeguard their cardiovascular health. The future of hypertension management lies in a holistic approach that addresses both the symptoms and the underlying causes, including the often-overlooked role of the SNS.
Early detection and intervention are crucial to preventing the long-term consequences of hypertension. Regular blood pressure screenings are recommended for all adults, and individuals with risk factors for hypertension should be monitored more closely.