The Complement Cascade And Its By Products Contribute To

Imagine your body as a meticulously guarded fortress, constantly vigilant against invaders. Immune cells stand watch on the ramparts, ready to sound the alarm. But what if the very system designed to protect you, the fortress's intricate defense mechanisms, could inadvertently contribute to the siege?
This is the complex reality researchers are uncovering about the complement cascade, a crucial part of our immune system. While designed to neutralize threats like bacteria and viruses, its powerful byproducts can, under certain circumstances, contribute to tissue damage and inflammatory diseases.
The Complement Cascade: A Double-Edged Sword
The complement system, discovered over a century ago, is a network of proteins in the blood that work together to identify and eliminate pathogens. Think of it as a molecular alarm system that triggers a chain reaction, ultimately leading to the destruction of foreign invaders.
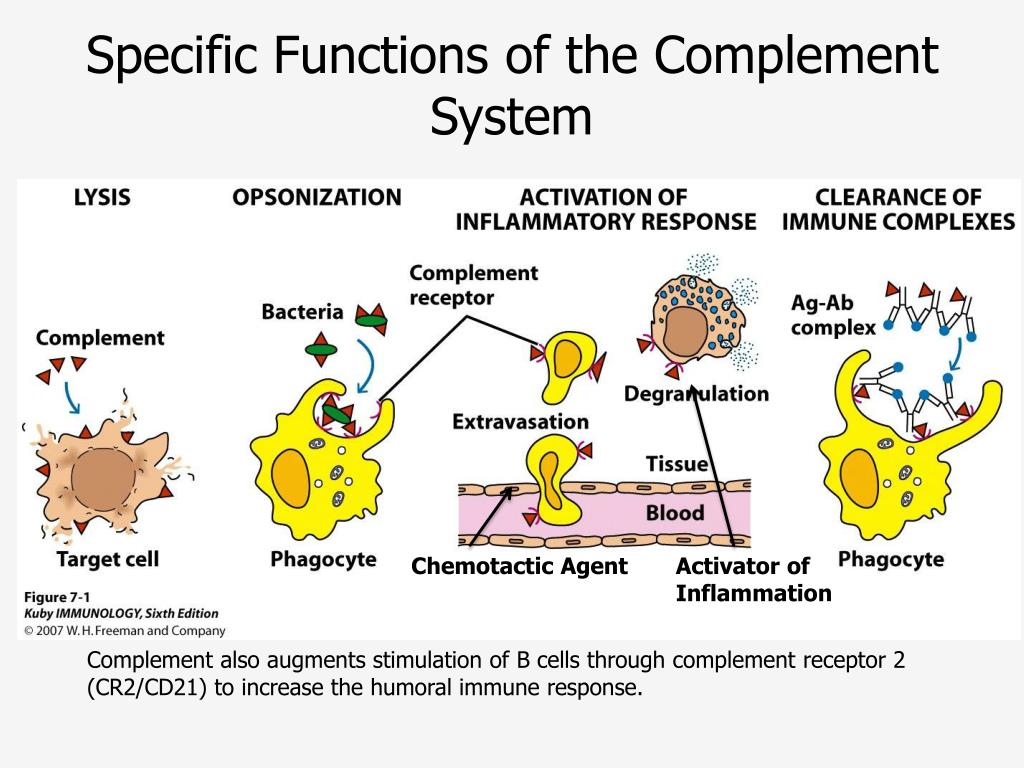
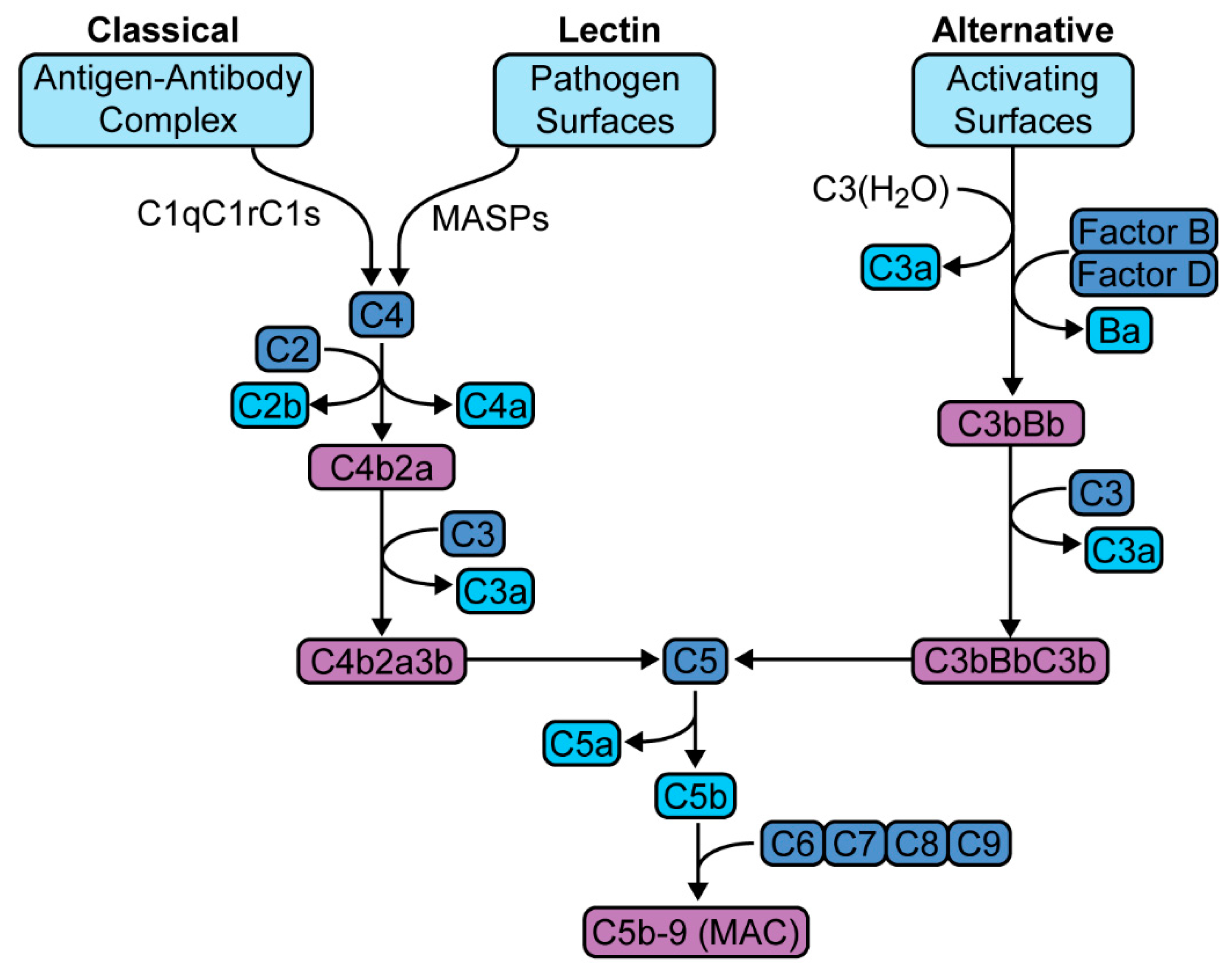
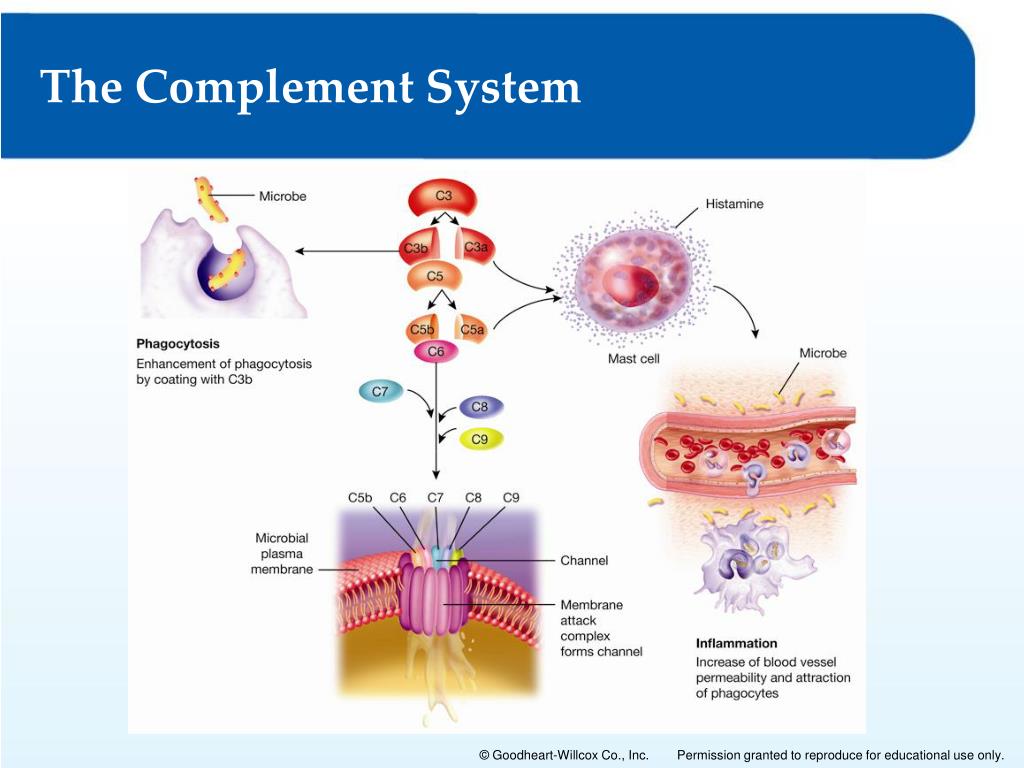
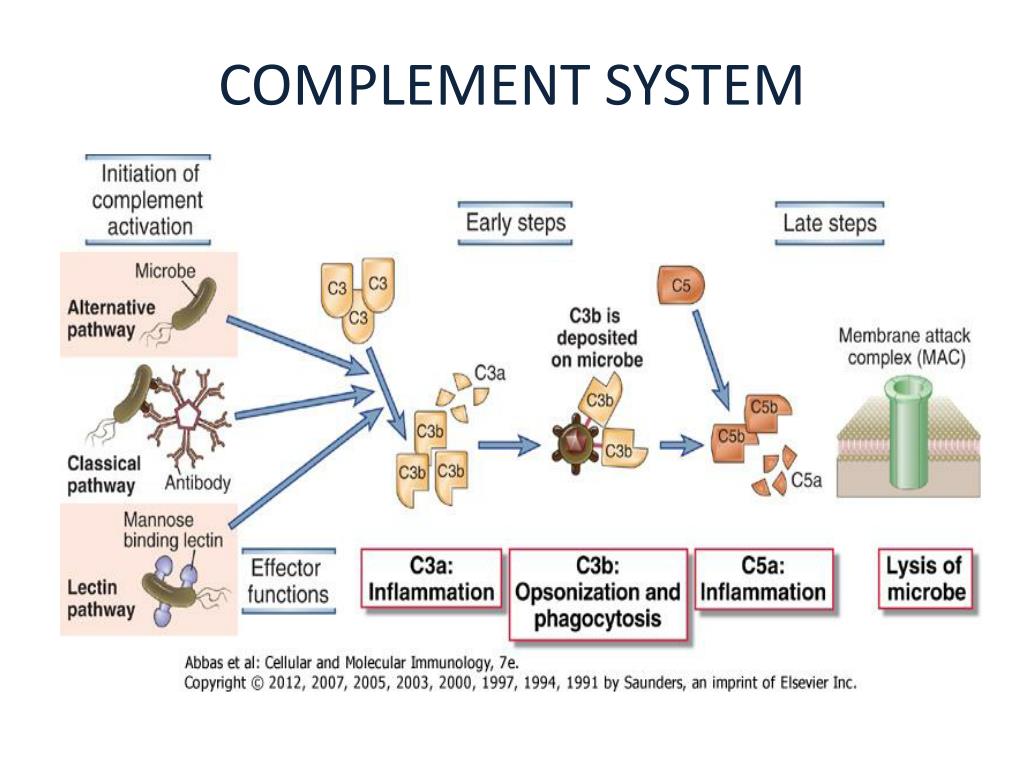
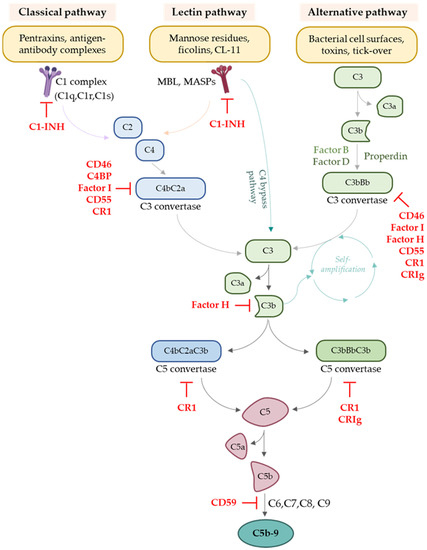
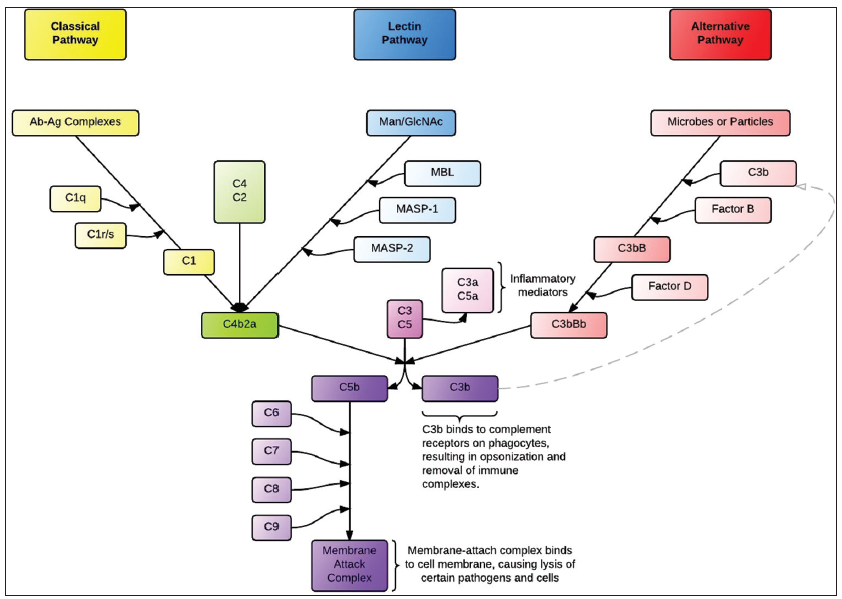
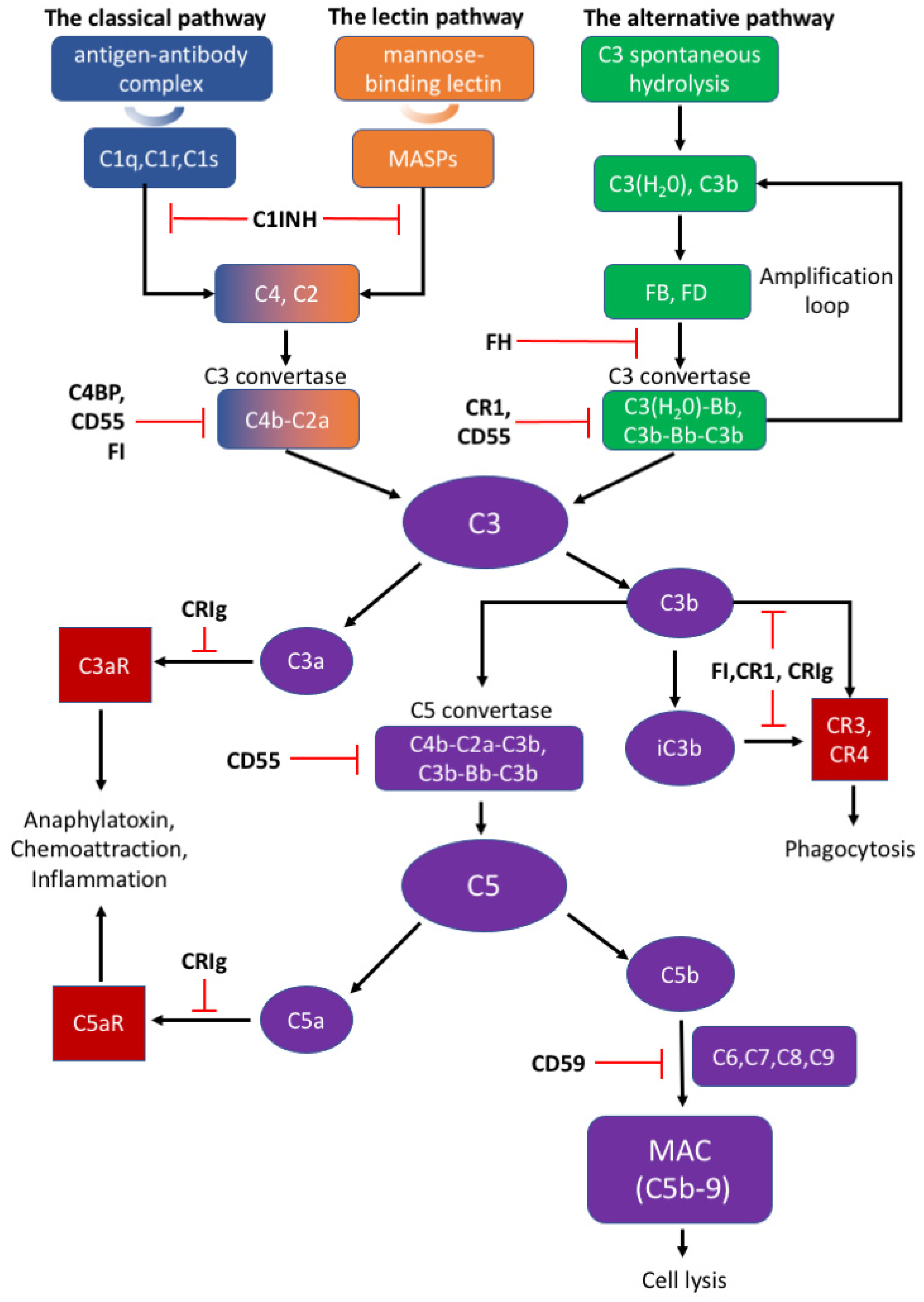
It is activated through three main pathways: the classical pathway, the alternative pathway, and the lectin pathway. Each pathway converges to activate a central component, C3, kicking off a cascade of events that lead to inflammation, opsonization (marking pathogens for destruction by phagocytes), and direct lysis (rupturing the cell membrane) of the target.
This sophisticated system is essential for defending us against infections. Yet, when dysregulated or overactivated, it can turn against our own tissues, contributing to a variety of diseases.
The Byproducts and Their Impact
The complement cascade generates a number of potent byproducts. These include C3a, C5a, and the membrane attack complex (MAC), all of which play vital roles in immune defense, but can also drive inflammation and tissue damage.
C3a and C5a are anaphylatoxins, meaning they can trigger the release of histamine from mast cells, leading to vasodilation and increased vascular permeability. This contributes to inflammation and can even cause anaphylactic shock in severe cases.
C5a also acts as a chemoattractant, drawing immune cells, such as neutrophils, to the site of inflammation. While crucial for fighting infection, an excessive influx of neutrophils can release damaging enzymes and reactive oxygen species, exacerbating tissue injury.
The MAC, formed by the terminal components of the complement cascade (C5b-9), inserts itself into the cell membrane of pathogens, creating pores that cause cell lysis. However, in certain situations, the MAC can also target healthy cells, leading to their destruction.
Diseases Linked to Complement Dysregulation
The list of diseases linked to complement dysregulation is extensive and growing. It includes autoimmune diseases, inflammatory diseases, and even neurodegenerative disorders.
In autoimmune diseases like systemic lupus erythematosus (SLE) and rheumatoid arthritis, the complement system can mistakenly target the body's own tissues, leading to chronic inflammation and organ damage. Studies have shown elevated levels of complement components and activation products in the blood and affected tissues of patients with these diseases.
In inflammatory diseases such as age-related macular degeneration (AMD), the complement system plays a significant role in the development and progression of the disease. Specifically, the alternative pathway of complement is implicated in the chronic inflammation that damages the retina, leading to vision loss.
Emerging research suggests that the complement system may also be involved in neurodegenerative disorders like Alzheimer's disease. Activated complement components have been found in the brains of Alzheimer's patients, contributing to neuronal damage and cognitive decline.
COVID-19, the recent pandemic caused by SARS-CoV-2, highlighted yet another area where complement dysregulation can have devastating consequences. Studies have shown that the complement system is excessively activated in severe COVID-19, contributing to acute respiratory distress syndrome (ARDS) and other life-threatening complications.
Therapeutic Strategies: Targeting the Complement Cascade
Given the significant role of the complement system in various diseases, researchers are actively developing therapeutic strategies to target its activity. These approaches aim to selectively inhibit specific components of the cascade, thereby reducing inflammation and tissue damage while preserving the system's essential immune functions.
One promising approach involves the use of complement inhibitors, which are drugs that block the activation of specific complement components. For example, eculizumab, a monoclonal antibody that inhibits C5, has been approved for the treatment of paroxysmal nocturnal hemoglobinuria (PNH) and atypical hemolytic uremic syndrome (aHUS), both of which are characterized by excessive complement activation.
Other therapeutic strategies focus on targeting specific complement receptors or downstream signaling pathways. These approaches aim to modulate the inflammatory response triggered by complement activation, rather than directly inhibiting the cascade itself.
While significant progress has been made in developing complement-targeted therapies, challenges remain. One major challenge is the complexity of the complement system itself, with its multiple pathways and interacting components. Another challenge is the potential for off-target effects and the need to carefully balance the benefits of inhibiting complement activation with the risk of impairing immune function.
The Future of Complement Research
The study of the complement cascade is a rapidly evolving field, with new discoveries constantly expanding our understanding of its role in health and disease. Future research will likely focus on identifying new targets for therapeutic intervention, developing more selective and effective complement inhibitors, and understanding the complex interplay between the complement system and other components of the immune system.
By unraveling the intricate mechanisms of the complement cascade and its byproducts, we can hope to develop more targeted and effective therapies for a wide range of diseases, ultimately improving the lives of millions of people.
The journey to understand the complement system is ongoing, but the progress made so far offers hope for a future where we can harness its power for good, while mitigating its potential for harm. It's a complex dance of defense, and we are learning to lead.