The Manifestations Of A Disease Are Best Defined As The
The insidious nature of disease often lies not just in its cause, but in the myriad ways it chooses to manifest itself. From a subtle fatigue that lingers for weeks to a sudden, debilitating pain that renders one immobile, understanding the full spectrum of these manifestations is paramount for timely diagnosis, effective treatment, and ultimately, better patient outcomes.
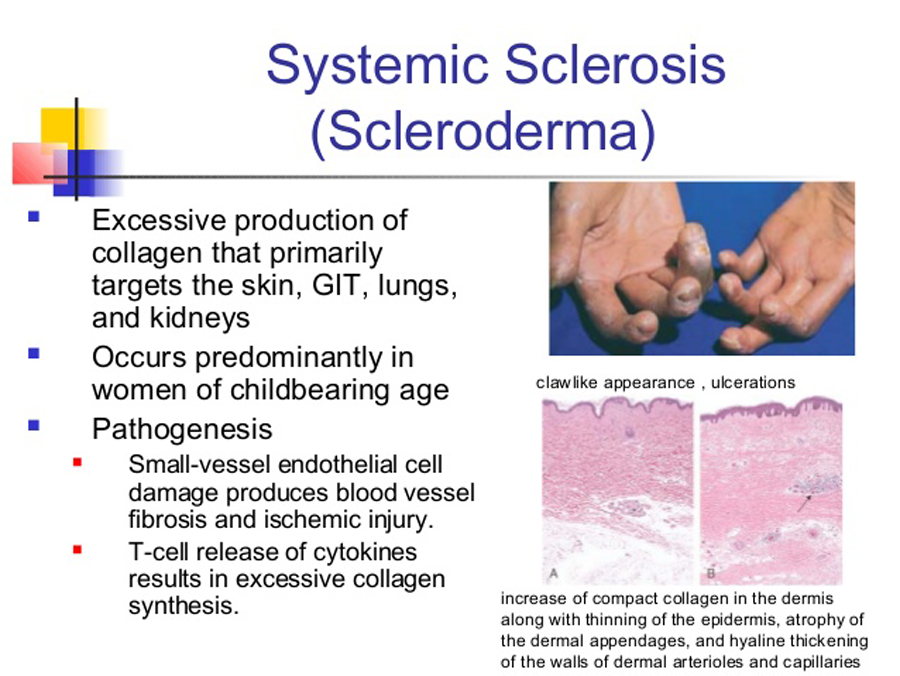
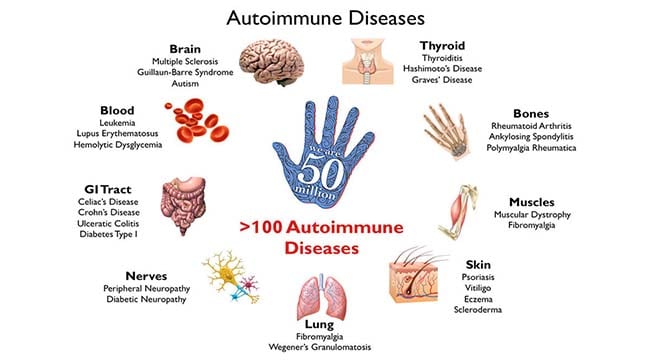
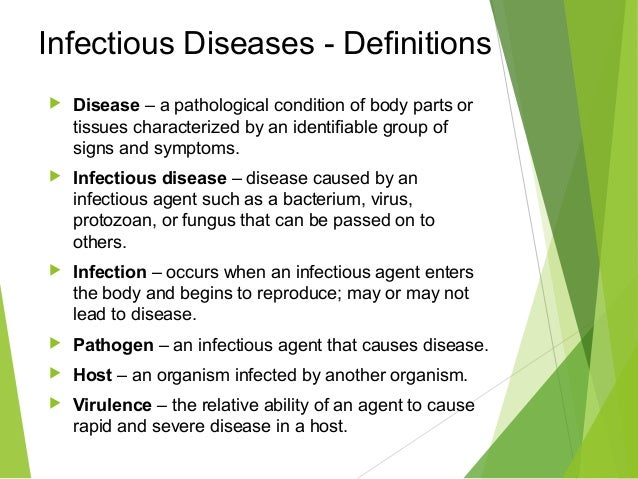
The term, "The Manifestations Of A Disease Are Best Defined As The," refers to the observable or detectable characteristics and symptoms that arise as a direct result of the disease process. This encompasses a wide range of signs, symptoms, laboratory findings, and imaging results that collectively paint a picture of the ailment affecting an individual. Accurate interpretation of these manifestations, a complex interplay of medical knowledge, clinical experience, and diagnostic tools, is essential for effective healthcare.
Defining Manifestations: A Medical Perspective
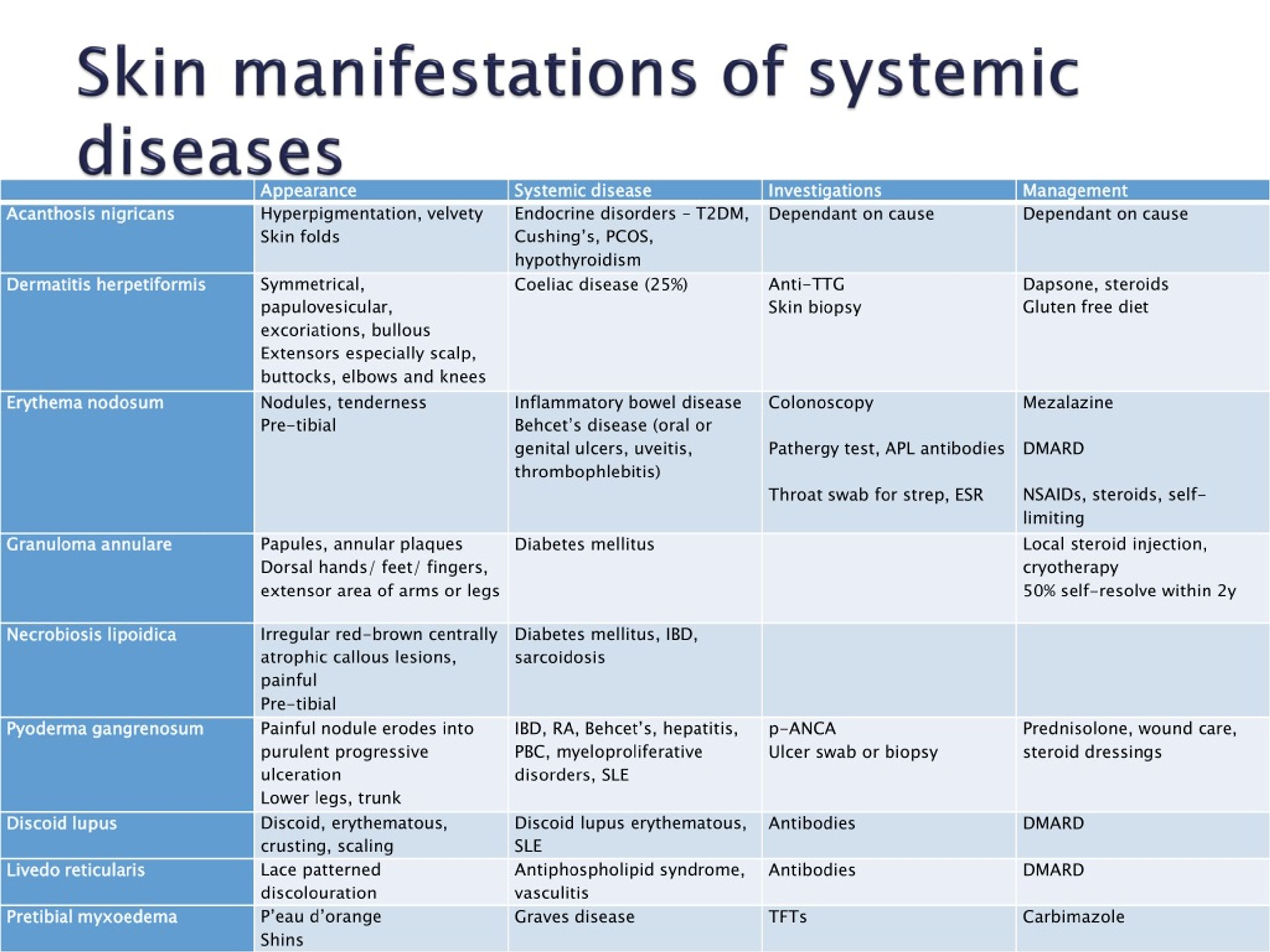
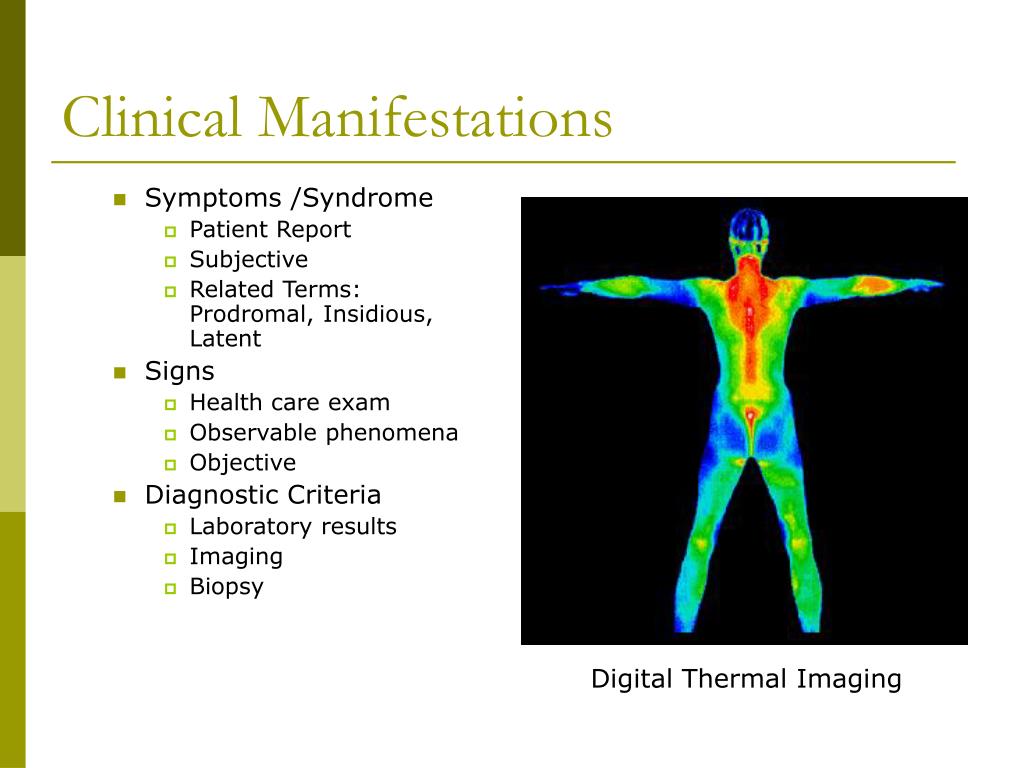
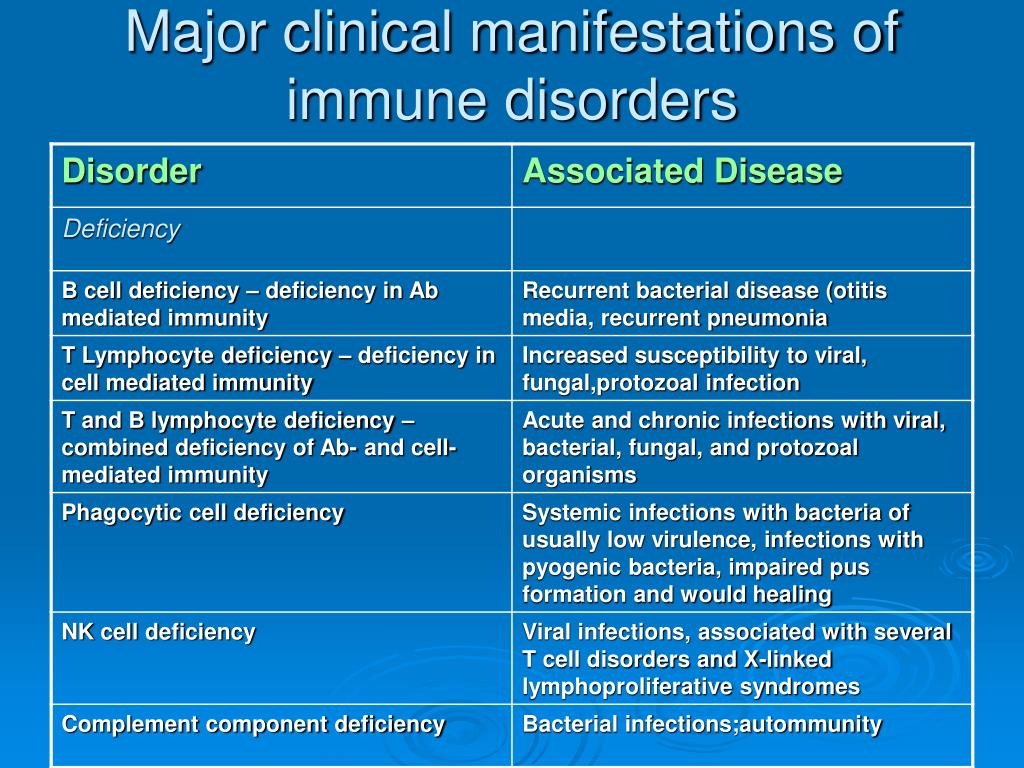
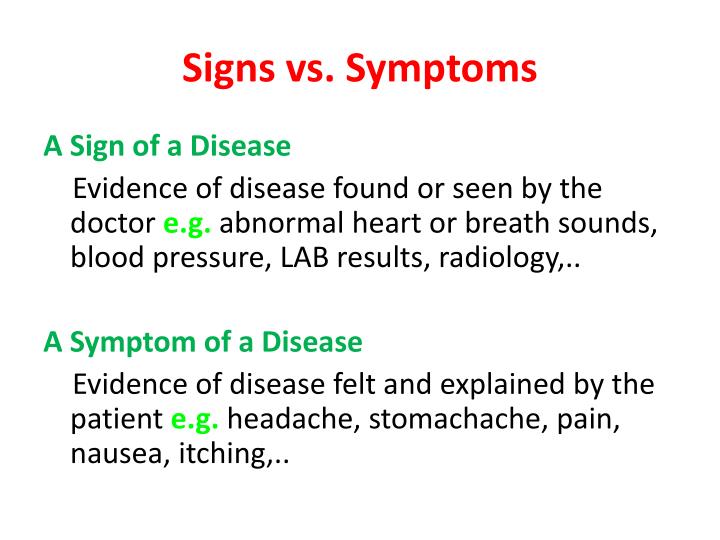
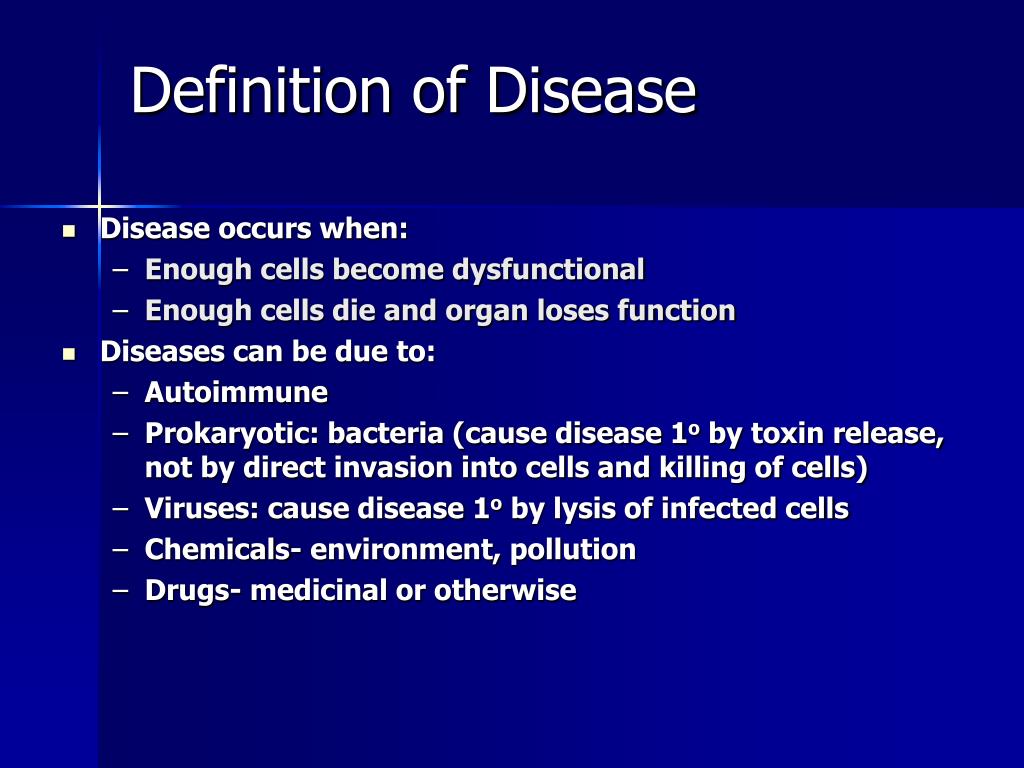
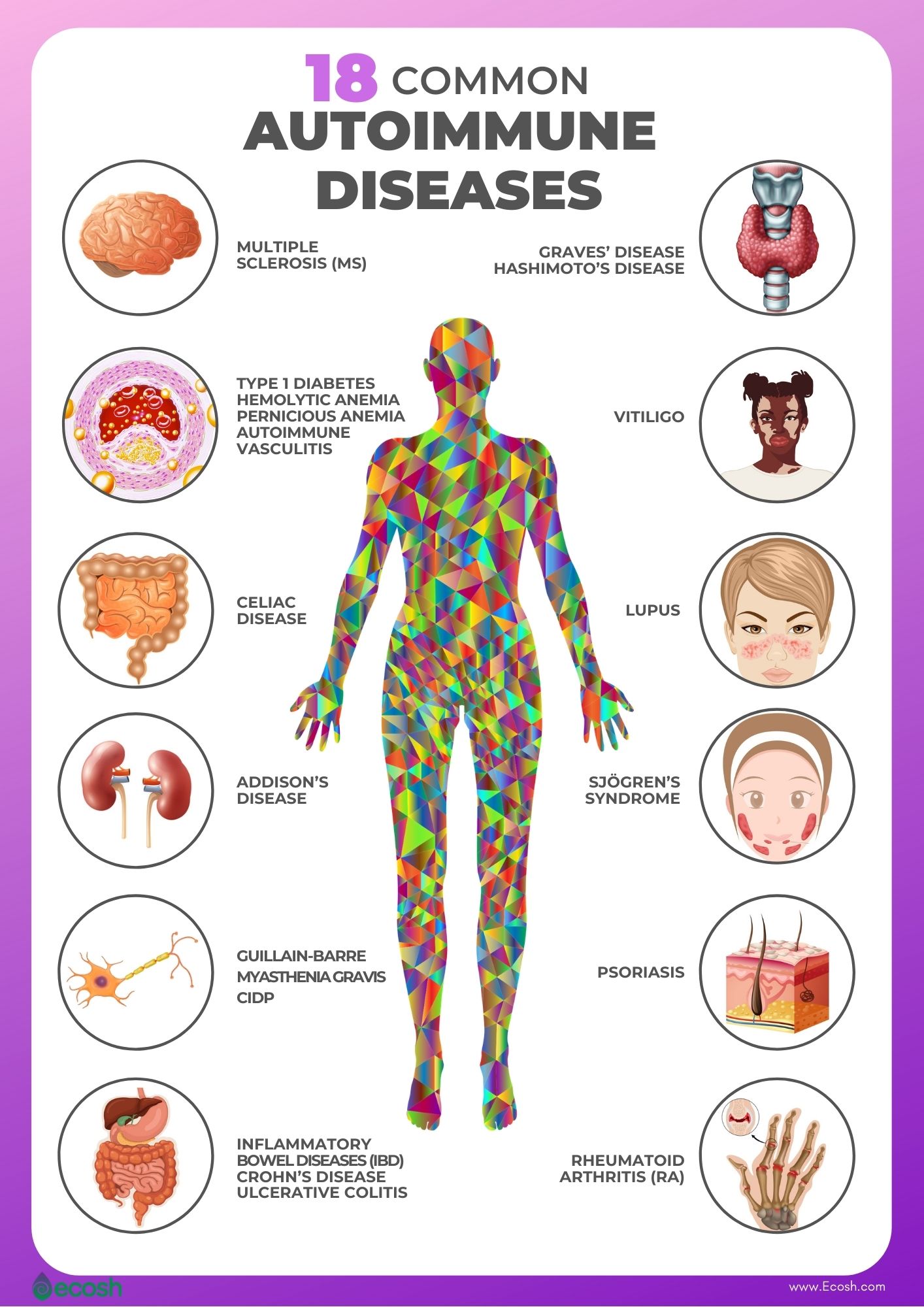
From a purely medical standpoint, disease manifestations are the objective and subjective indicators that clinicians use to identify and classify illnesses. Signs are objective findings detectable by a healthcare professional during a physical examination or through diagnostic tests. These include things like fever, rash, elevated blood pressure, or abnormal lab results.
Symptoms, on the other hand, are subjective experiences reported by the patient themselves. Pain, nausea, fatigue, and dizziness all fall under this category.
The interplay between signs and symptoms is critical in differential diagnosis, the process of distinguishing between diseases with similar presentations. A cough, for example, is a symptom, but the doctor's observation of wheezing (a sign) coupled with a patient's reported shortness of breath can point towards asthma or bronchitis.
The Role of Diagnostic Tools
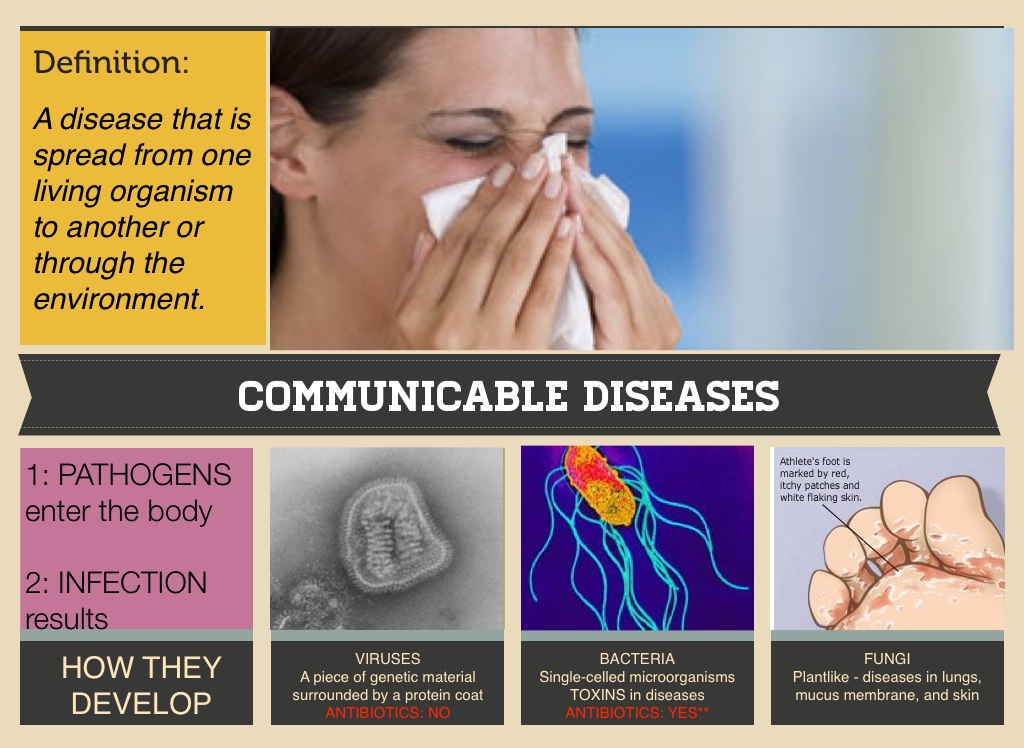
Modern medicine relies heavily on diagnostic tools to detect and characterize disease manifestations. Imaging techniques such as X-rays, CT scans, and MRIs can visualize internal structures and identify abnormalities like tumors, inflammation, or organ damage.
Laboratory tests, including blood tests, urine analyses, and biopsies, can provide crucial information about the body's physiological state. These tests can reveal the presence of infection, assess organ function, or detect genetic markers associated with specific diseases. The accuracy and sensitivity of these tests are continuously improving, allowing for earlier and more precise detection of disease manifestations.
Furthermore, advanced molecular techniques like genomics and proteomics are playing an increasingly important role in understanding disease manifestations at a cellular and molecular level. By analyzing gene expression patterns and protein profiles, researchers can identify unique biomarkers that differentiate between disease subtypes and predict treatment responses.
The Patient Experience: A Crucial Element
While objective signs and diagnostic tests provide valuable information, the patient's own experience of their illness is equally important. Understanding the specific symptoms a patient is experiencing, how those symptoms impact their daily life, and their personal concerns about their health is crucial for providing patient-centered care.
Effective communication between the patient and the healthcare provider is essential for eliciting a comprehensive understanding of the patient's subjective experience. A detailed medical history, careful listening, and empathy are all vital components of this process.
The importance of patient-reported outcomes (PROs) is also increasingly recognized in clinical research and practice. PROs are standardized questionnaires that capture the patient's perspective on their symptoms, functional status, and quality of life. These measures can provide valuable insights into the impact of disease and treatment from the patient's point of view.
Challenges and Future Directions
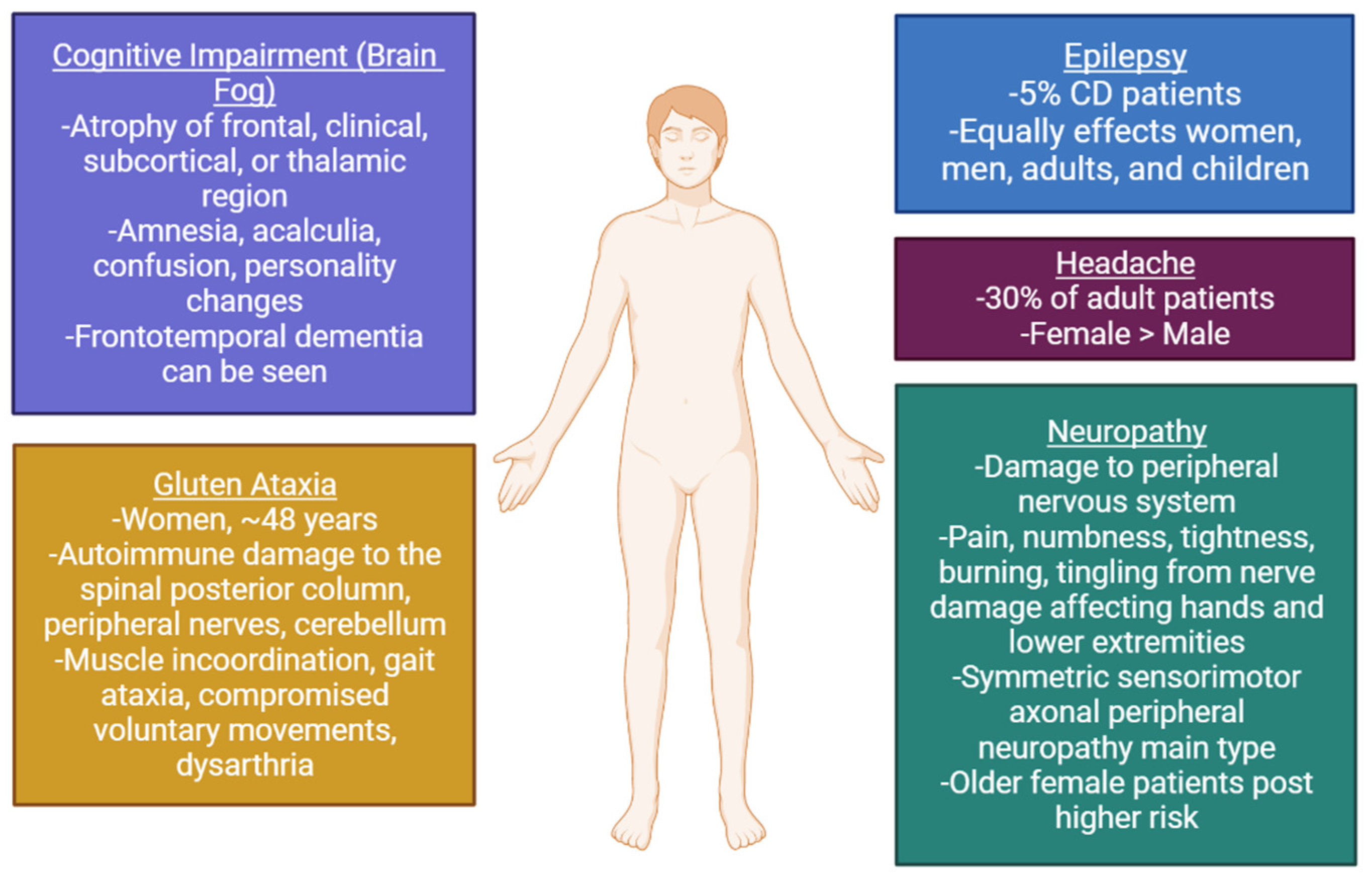
Despite significant advances in our understanding of disease manifestations, several challenges remain. One major challenge is the variability in how diseases present across different individuals.
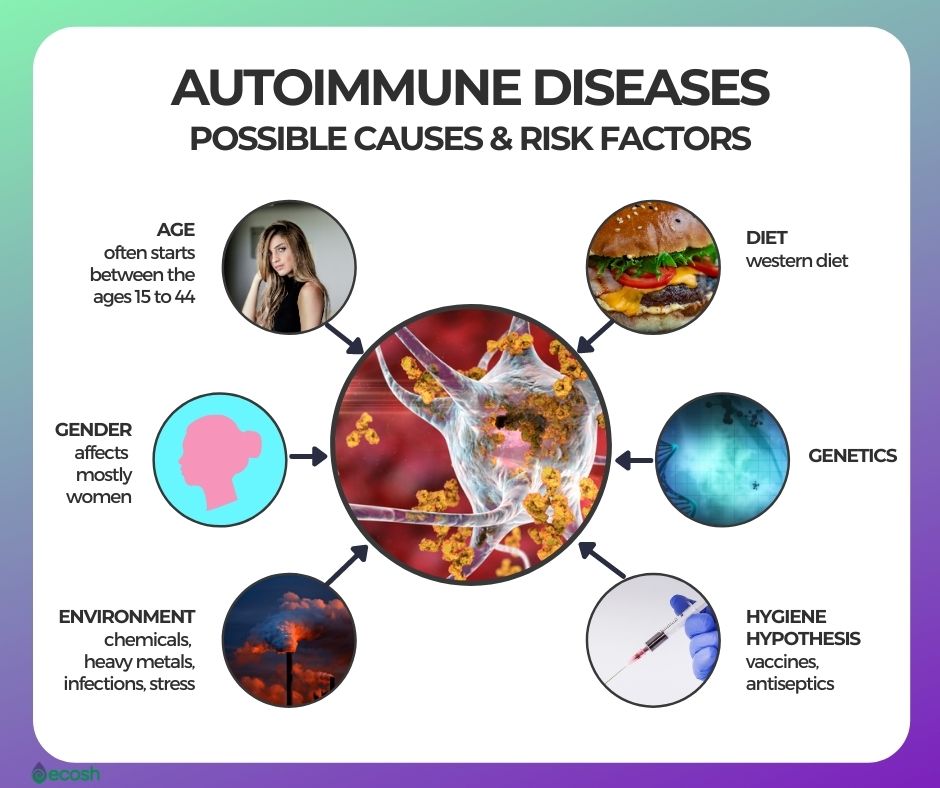
Factors such as age, gender, genetics, lifestyle, and co-existing conditions can all influence the expression of disease. This variability can make diagnosis difficult and lead to delays in treatment.
Another challenge is the presence of non-specific symptoms, which can be associated with a wide range of conditions. Fatigue, for example, can be a symptom of anything from a common cold to a serious chronic illness. Differentiating between these possibilities requires careful clinical evaluation and often, extensive diagnostic testing.
Looking ahead, several promising avenues of research hold the potential to improve our understanding and detection of disease manifestations. The use of artificial intelligence and machine learning to analyze large datasets of clinical data, including electronic health records, imaging results, and genomic information, can help identify patterns and predict disease risk.
Furthermore, the development of new diagnostic technologies, such as wearable sensors and point-of-care devices, can enable continuous monitoring of physiological parameters and early detection of disease manifestations. These advances promise to revolutionize healthcare by enabling earlier diagnosis, more personalized treatment, and ultimately, improved patient outcomes.
Ethical Considerations
The increasing sophistication of diagnostic tools and the ability to identify disease manifestations at an early stage also raise important ethical considerations. For example, genetic testing can reveal predispositions to certain diseases, but this information may also have implications for insurance coverage and employment opportunities.
The use of AI in healthcare raises questions about data privacy and security, as well as the potential for bias in algorithms. It is crucial to ensure that these technologies are developed and used in a responsible and ethical manner, with appropriate safeguards in place to protect patient rights and prevent discrimination.
Transparency and informed consent are essential when utilizing advanced diagnostic tools. Patients should be fully informed about the potential benefits and risks of testing, as well as the implications of the results.
Conclusion
Understanding "The Manifestations Of A Disease Are Best Defined As The" is fundamental to effective medical practice. It requires a holistic approach that integrates objective signs, subjective symptoms, and sophisticated diagnostic tools.
While challenges remain, ongoing research and technological advancements hold the promise of improving our ability to detect and characterize disease manifestations, leading to earlier diagnosis, more personalized treatment, and ultimately, better health outcomes for all. The continuous evolution of medical knowledge and technology necessitates a commitment to lifelong learning and adaptation among healthcare professionals.



:max_bytes(150000):strip_icc()/respiratory-diseases-5206842_final_2-d9513b617d8b42ffb3ab821c5cbb5a99.jpg)