Treatment Of Bk Virus In Kidney Transplantation

Kidney transplant recipients face a persistent threat: the BK virus (BKV). Early detection and intervention are crucial to prevent graft loss.
BKV reactivation, a common complication following kidney transplantation, can lead to BK virus-associated nephropathy (BKVAN) and subsequent allograft failure, impacting long-term patient survival.
Prevalence and Risk Factors
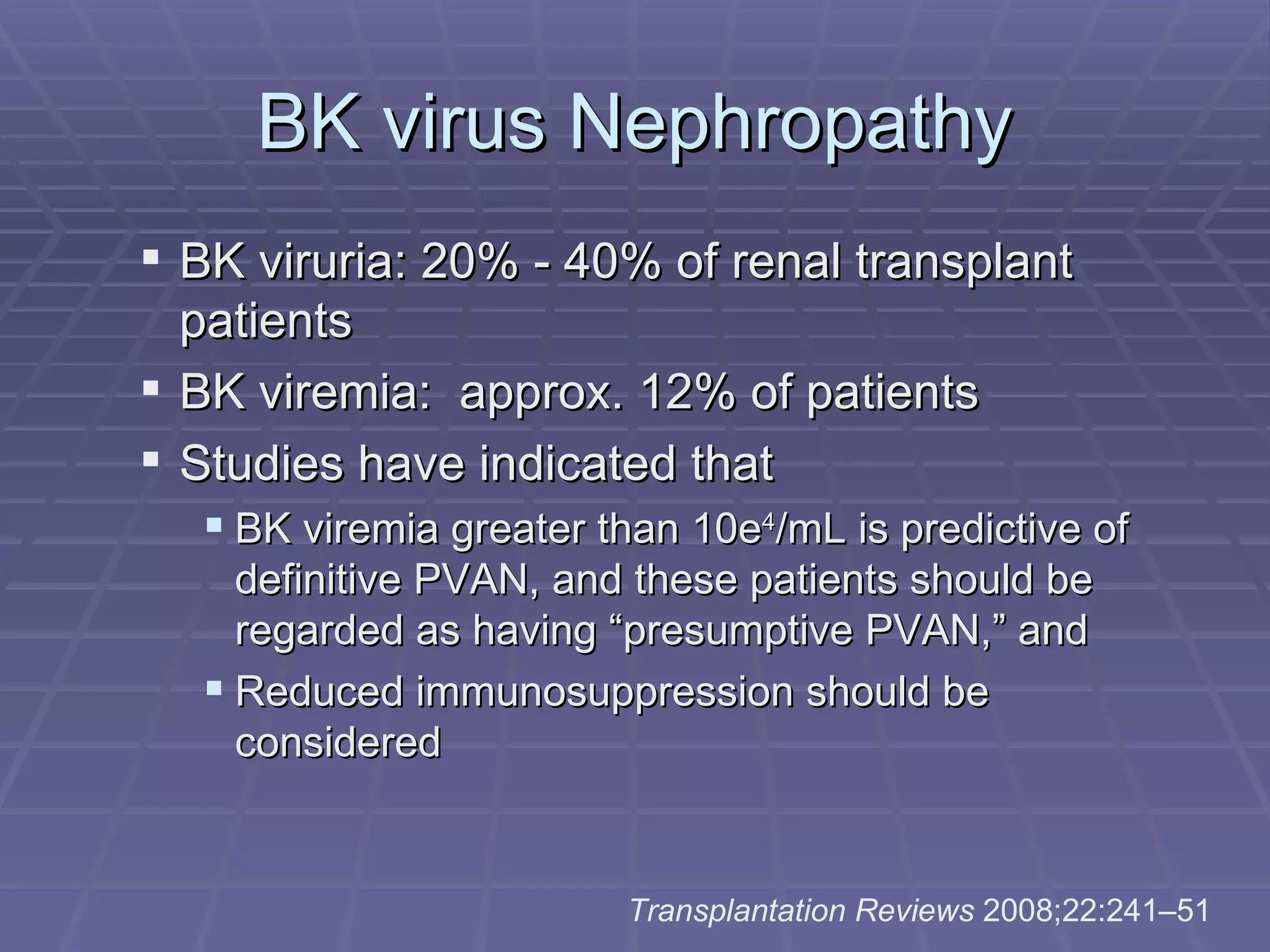
BKV affects a significant proportion of kidney transplant patients. Studies indicate that up to 90% of adults have been exposed to BKV, and reactivation occurs in 1-10% of kidney transplant recipients.
The incidence of BKVAN, the severe form of BKV infection, ranges from 1-10%. Intense immunosuppression to prevent organ rejection is a primary risk factor.
Other risk factors include older age, male gender, deceased donor transplantation, ureteral stents, and specific immunosuppressive regimens, particularly those involving tacrolimus and mycophenolate mofetil (MMF).
Diagnosis and Monitoring
Early detection is paramount. Routine monitoring for BKV DNA in blood and urine is essential for all kidney transplant recipients.
Monitoring typically begins within the first few months post-transplant and continues regularly. Quantitative PCR assays are used to measure BKV viral load in plasma and urine.
A rising viral load triggers further investigation. A kidney biopsy is performed to confirm BKVAN if the viral load exceeds a predetermined threshold, typically >10,000 copies/mL in blood.
Treatment Strategies
The cornerstone of BKV treatment is reduction of immunosuppression. This allows the patient's immune system to better control the virus.
The specific reduction strategy depends on the individual patient's clinical situation. Strategies include decreasing the dose of calcineurin inhibitors (tacrolimus or cyclosporine), stopping or reducing MMF, or switching to an alternative immunosuppressant such as sirolimus.
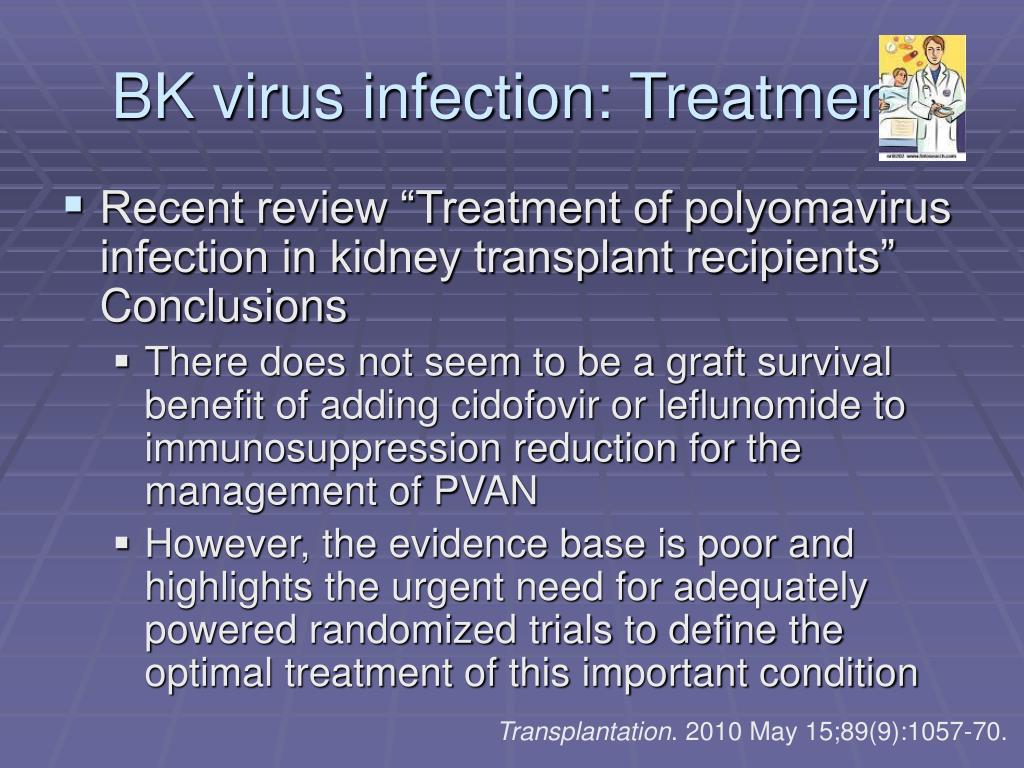
Antiviral medications, such as leflunomide and cidofovir, are sometimes used. However, their efficacy is limited, and they carry potential side effects.
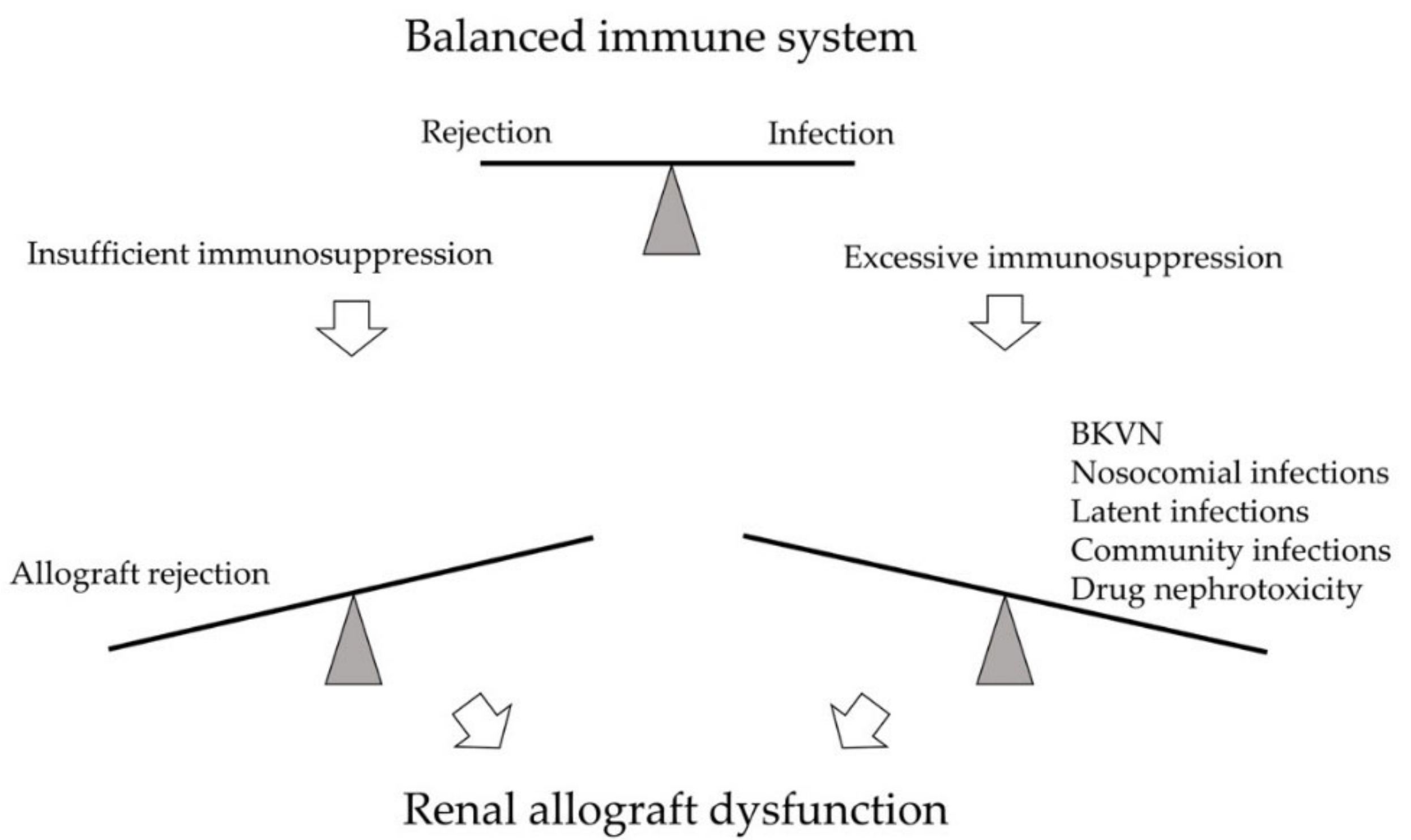
Immunosuppression Reduction: A Balancing Act
Reducing immunosuppression carries the risk of acute rejection. Careful monitoring of kidney function and consideration of potential rejection episodes are crucial.
Close communication between the transplant team, including nephrologists and transplant surgeons, is vital. Individualized treatment plans should be developed based on the patient's specific risk factors and clinical course.
Emerging Therapies
Research is ongoing to develop more effective and targeted therapies for BKVAN. These include new antiviral agents and immunomodulatory strategies.
Several clinical trials are evaluating the use of adoptive T-cell therapy. This involves infusing patients with BKV-specific T cells to enhance viral clearance.
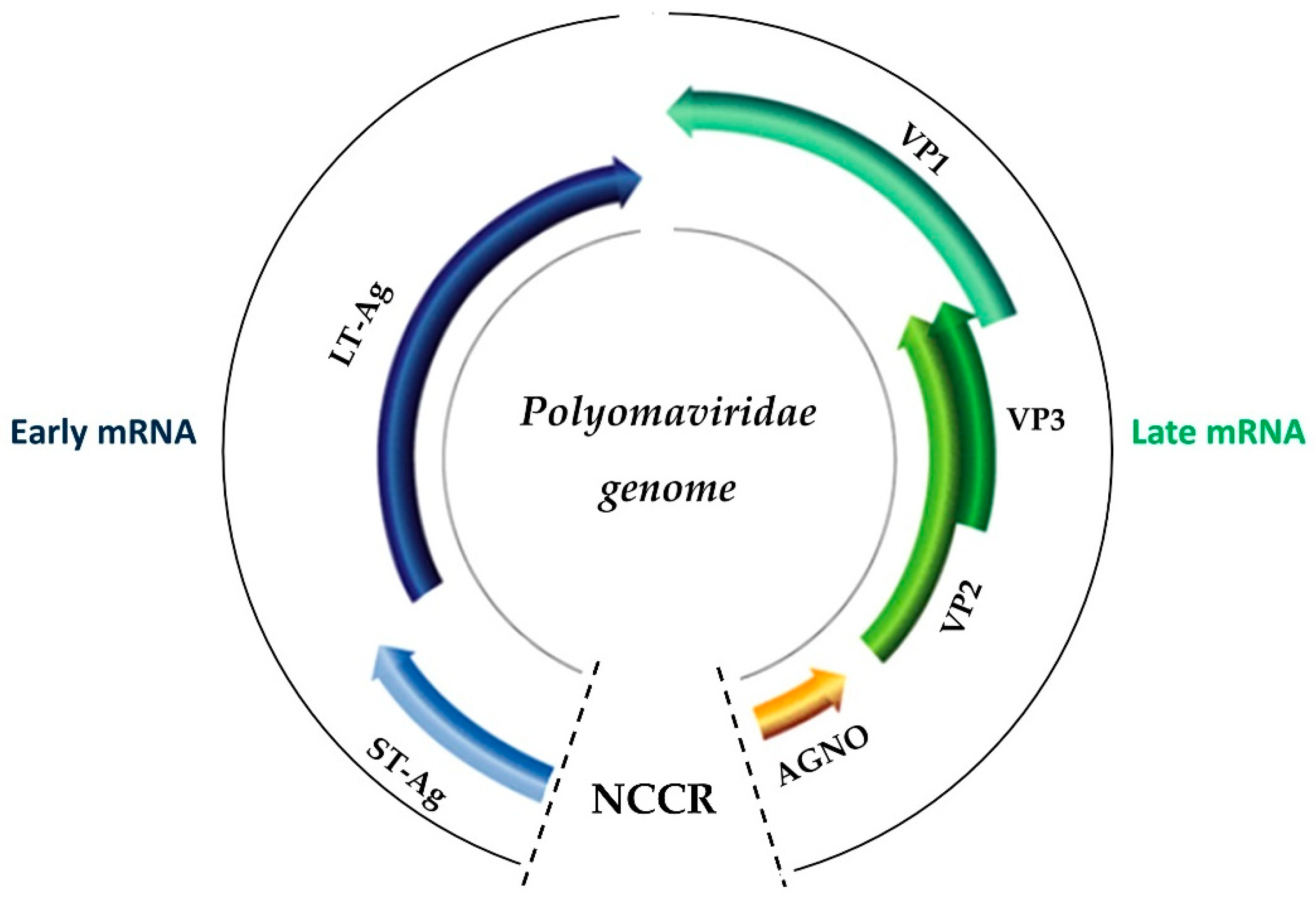
Novel antiviral drugs targeting different stages of the BKV lifecycle are also in development. These hold promise for improving treatment outcomes and reducing the need for aggressive immunosuppression reduction.
Challenges and Future Directions
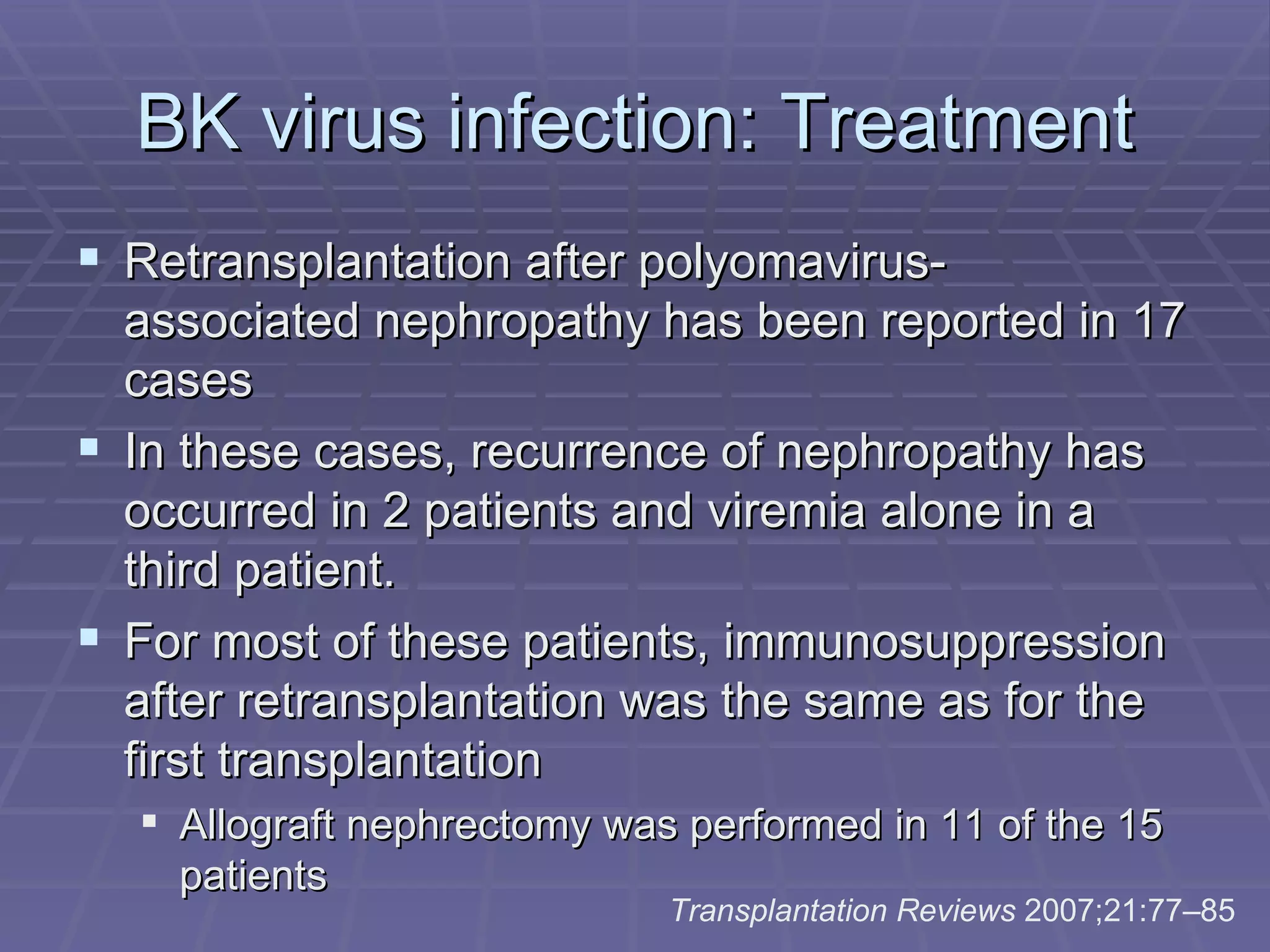
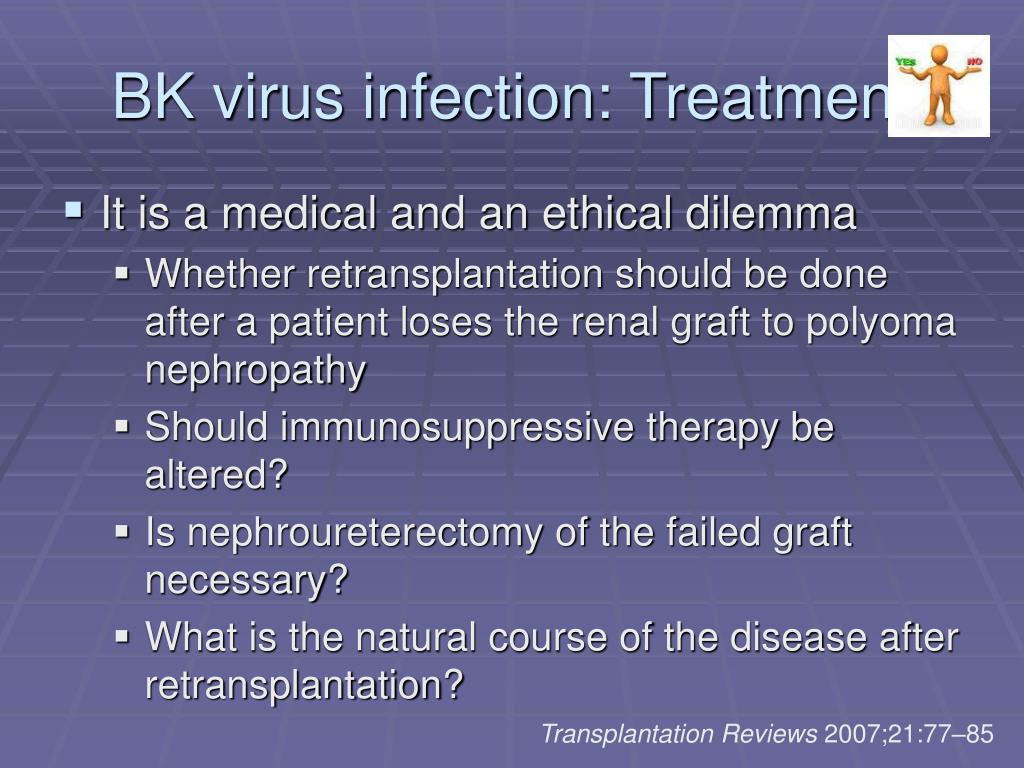
BKVAN remains a significant challenge in kidney transplantation. Current treatment strategies are not always effective, and the risk of rejection following immunosuppression reduction is a major concern.
Improved diagnostic tools, such as non-invasive biomarkers, are needed to detect BKVAN earlier and more accurately. This would allow for more timely intervention and potentially prevent irreversible kidney damage.
Further research is needed to develop safer and more effective antiviral therapies. A personalized approach to BKV management, taking into account individual patient risk factors and immune responses, is crucial for improving outcomes.
Impact on Graft Survival
Uncontrolled BKVAN can lead to graft loss. Studies have shown that BKVAN is associated with a significantly increased risk of graft failure and return to dialysis.
Early diagnosis and prompt treatment are essential to preserve kidney function. Long-term monitoring for BKV is crucial to detect reactivation and intervene before irreversible damage occurs.
Successful management of BKV requires a multidisciplinary approach. This includes close collaboration between nephrologists, transplant surgeons, infectious disease specialists, and other healthcare professionals.
Call to Action
Transplant centers must adhere to standardized monitoring protocols. Consistent screening for BKV is necessary to identify high-risk patients early.
Prompt intervention upon detection of BKV is paramount. Standardized treatment algorithms should be implemented to ensure consistent and effective management.
Continued research and development of new therapies are essential. Investment in innovative diagnostic and therapeutic approaches is crucial for improving outcomes for kidney transplant recipients affected by BKV.
Patients need to be educated about BKV and its potential impact. Understanding the importance of adherence to monitoring and treatment plans is vital.
The next steps involve implementing the latest research findings into clinical practice. There is a need to refine monitoring strategies, optimize immunosuppression protocols, and develop more effective antiviral therapies to combat BKV infection in kidney transplant recipients.