United Healthcare Class Action Lawsuit Sign Up

A nationwide class action lawsuit against United Healthcare, one of the nation's largest health insurance providers, is gaining traction, with a growing number of individuals signing up to join the legal battle. The lawsuit alleges systematic underpayment and denial of claims for out-of-network healthcare services, potentially impacting millions of policyholders across the country.
At its core, the class action suit aims to hold United Healthcare accountable for what plaintiffs claim are unfair and deceptive practices that have resulted in significant financial burdens for patients seeking necessary medical care outside of the insurer's network. The outcome of this case could reshape the landscape of healthcare insurance reimbursement and influence how out-of-network claims are processed in the future.
The Allegations Against United Healthcare
The lawsuit centers on the assertion that United Healthcare has consistently utilized flawed or inappropriate methodologies to determine reimbursement rates for out-of-network services. Plaintiffs argue that these methods often result in payments far below the usual, customary, and reasonable (UCR) rates for similar services in a given geographic area. This forces policyholders to shoulder the difference between the billed amount and the insurer's payment, leading to unexpected and substantial medical bills.
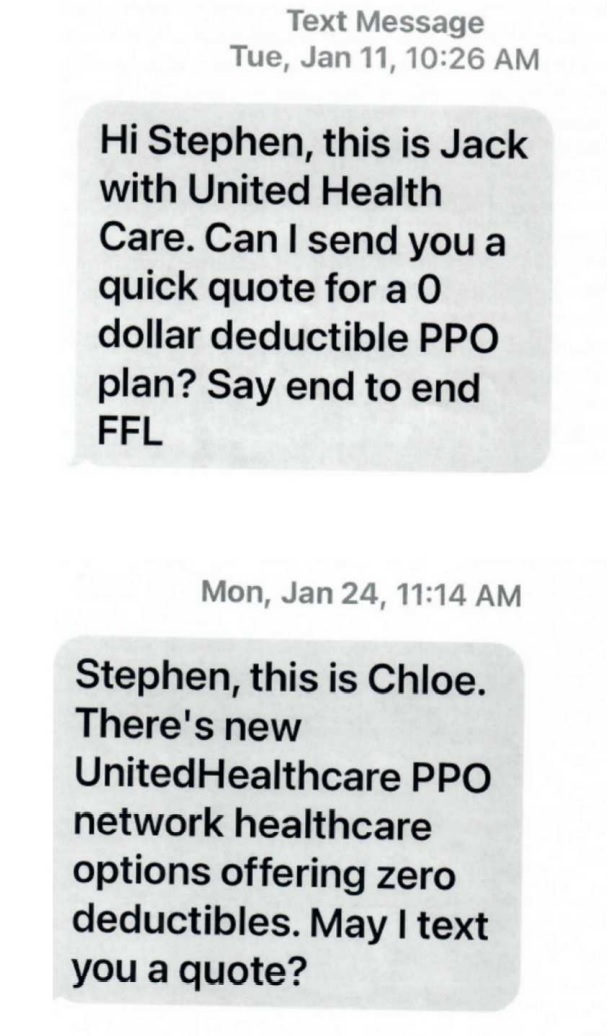
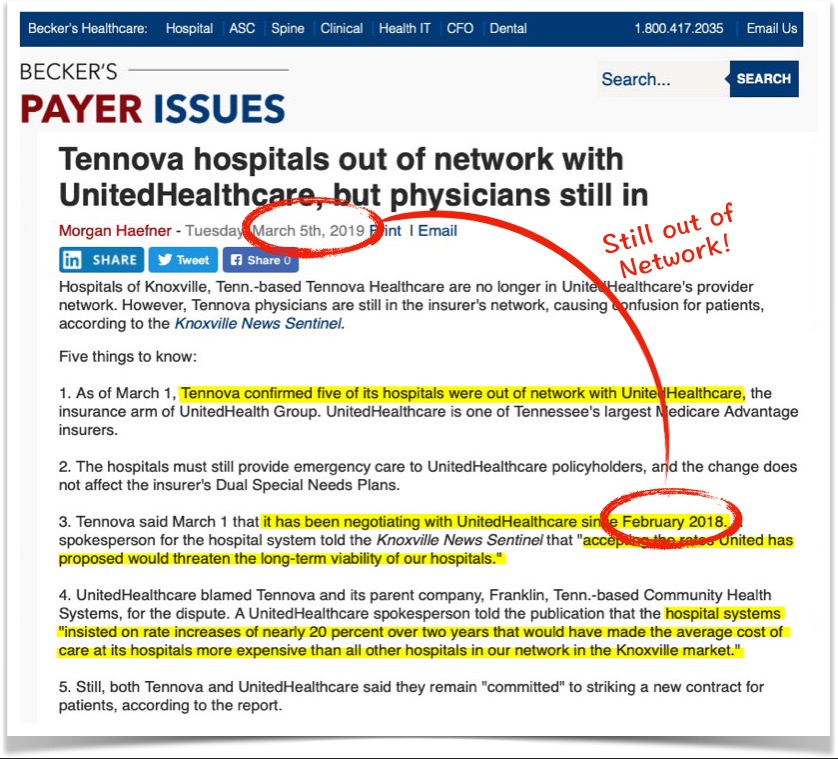
Furthermore, the lawsuit claims that United Healthcare has unjustly denied claims for out-of-network care based on arbitrary or inconsistent criteria. Patients have reported denials even when their in-network options were limited or non-existent, or when emergency medical situations necessitated immediate treatment at the nearest available facility, regardless of network affiliation. These denials allegedly violate the terms of their insurance policies and applicable state and federal laws.
The suit also challenges United Healthcare's use of algorithms and data analytics in claim processing, alleging that these systems are designed to minimize payouts rather than ensure fair and accurate reimbursements. This raises concerns about transparency and the potential for bias in the decision-making process, particularly when it comes to complex or high-cost medical procedures.
Who is Involved and Why?
The class action is being spearheaded by several law firms specializing in healthcare litigation and consumer protection. These firms have a track record of successfully representing patients and providers in disputes against insurance companies. They argue that United Healthcare's alleged practices are not only detrimental to patients but also undermine the integrity of the healthcare system as a whole.
Individuals signing up for the lawsuit include patients who have experienced underpayment or denial of out-of-network claims by United Healthcare. Many have shared stories of financial hardship, emotional distress, and difficulty accessing necessary medical care due to the insurer's alleged practices. Their participation is crucial to building a strong case and demonstrating the widespread impact of United Healthcare's policies.
Healthcare providers, particularly those who frequently treat out-of-network patients, are also closely watching the lawsuit. If successful, the suit could lead to fairer reimbursement rates for out-of-network services and reduce the administrative burden associated with appealing denied or underpaid claims. This would help ensure that providers are adequately compensated for their services and can continue to provide quality care to all patients, regardless of their insurance status.
The Sign-Up Process and Potential Outcomes
Individuals who believe they may have been affected by United Healthcare's out-of-network claim practices are encouraged to contact the law firms involved in the class action. The sign-up process typically involves providing documentation of their insurance policy, claim submissions, and any related correspondence with United Healthcare. This information will help the attorneys assess the individual's eligibility to participate in the lawsuit.
If the lawsuit is successful, eligible class members could receive compensation for underpaid or denied claims, as well as reimbursement for out-of-pocket expenses incurred as a result of United Healthcare's alleged practices. The exact amount of compensation will depend on the specific circumstances of each case and the overall settlement or judgment reached.
Beyond financial compensation, the lawsuit could also lead to significant changes in United Healthcare's claim processing procedures and reimbursement policies. This could include the adoption of more transparent and accurate methodologies for determining UCR rates, as well as stricter guidelines for denying out-of-network claims. Such changes would benefit not only current United Healthcare policyholders but also future enrollees.
Potential Impact and Future Implications
The United Healthcare class action lawsuit has the potential to set a precedent for similar litigation against other health insurance companies that engage in questionable out-of-network claim practices. A successful outcome could embolden patients and providers to challenge unfair reimbursement policies and demand greater transparency from insurers. This could lead to a more equitable and sustainable healthcare system.
The case also highlights the growing importance of understanding one's insurance coverage and advocating for fair treatment when seeking medical care. Policyholders are encouraged to carefully review their policy documents, keep detailed records of all claim submissions and correspondence, and seek legal advice if they believe their rights have been violated.
The outcome of this lawsuit will be closely watched by the healthcare industry, consumer advocacy groups, and policymakers alike. It underscores the need for greater oversight and regulation of health insurance practices to ensure that patients receive the care they need without facing undue financial burdens. The case serves as a reminder that individuals have the power to hold large corporations accountable for their actions and fight for a more just and equitable healthcare system.