What Is The First Line Treatment For Hypercalcemia
Imagine a garden, vibrant with life, but one plant starts to wilt, its leaves yellowing despite ample water and sunlight. The problem isn't obvious; it's not a pest or lack of care, but something within the soil itself, an imbalance that's throwing the whole system off-kilter. This is somewhat analogous to the human body when dealing with hypercalcemia, a condition where the calcium levels in the blood become too high, impacting everything from bone health to kidney function.
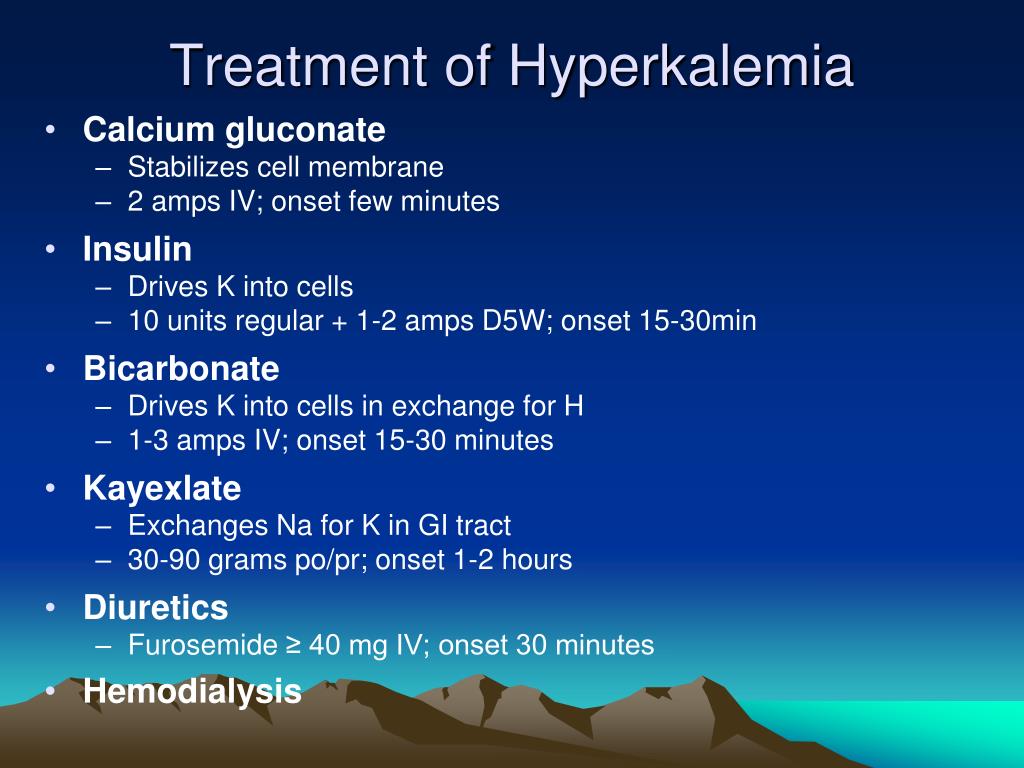
The first line treatment for hypercalcemia, a condition characterized by elevated calcium levels in the blood, typically involves immediate hydration with intravenous (IV) fluids, often saline solution. This helps to dilute the calcium concentration and promote its excretion through the kidneys, offering a rapid and effective initial approach. Following hydration, the administration of calcitonin and bisphosphonates may be considered to further reduce calcium levels and prevent future elevation.
Understanding Hypercalcemia: The Basics
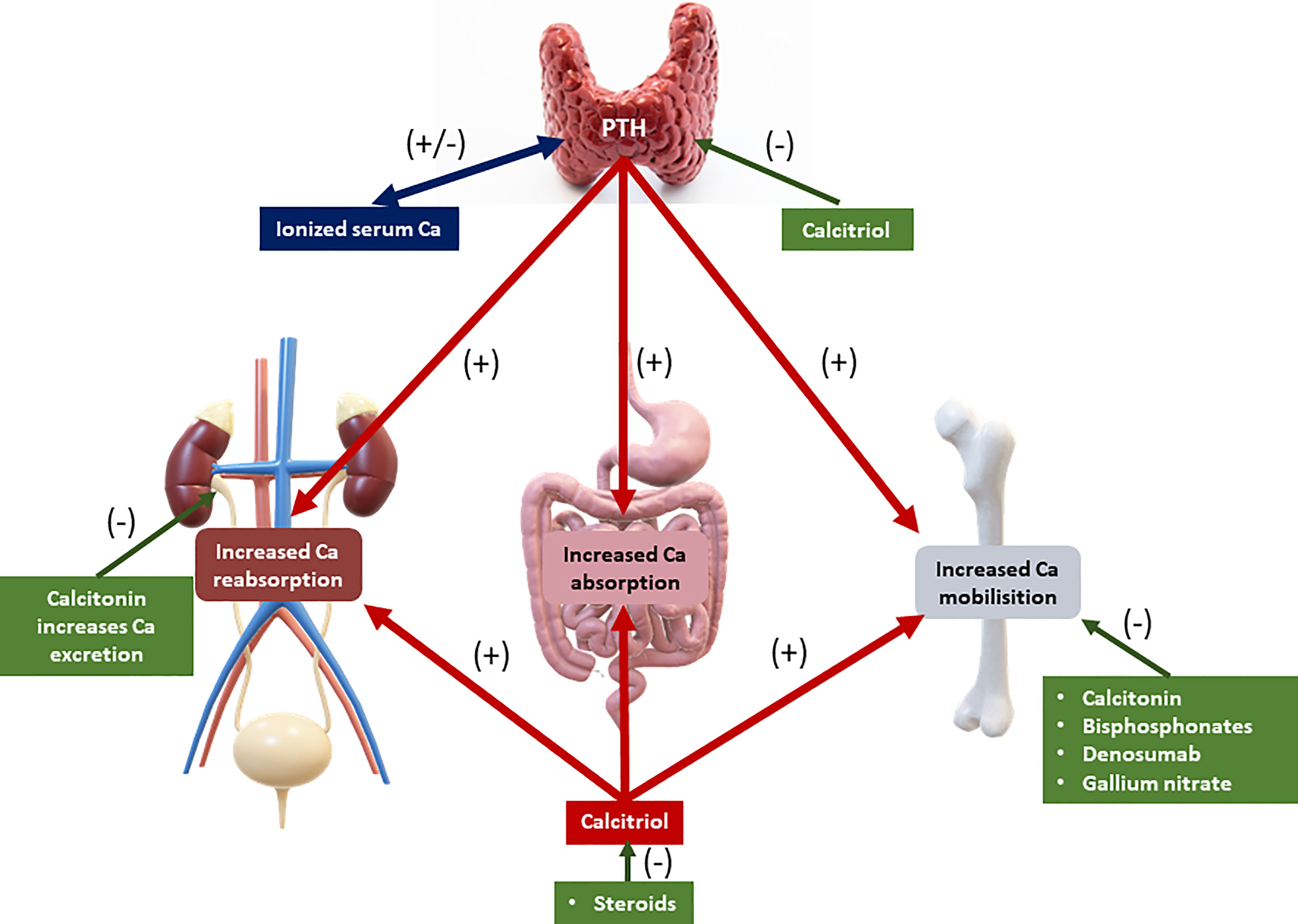
Hypercalcemia, at its core, is a disruption of calcium homeostasis in the body. Calcium, essential for a myriad of functions, including bone health, nerve transmission, muscle contraction, and blood clotting, is normally tightly regulated. When this regulation falters, calcium levels can rise above the normal range, leading to a cascade of potential health problems.
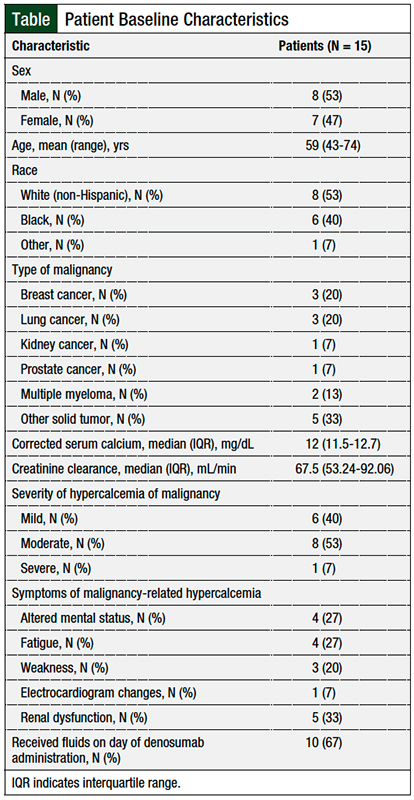
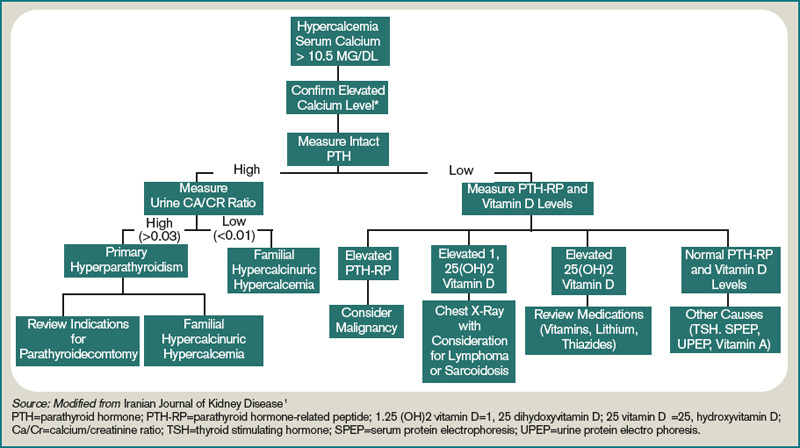
Several factors can contribute to hypercalcemia, with primary hyperparathyroidism and malignancy being the most common culprits. Primary hyperparathyroidism involves an overactivity of the parathyroid glands, which regulate calcium levels, while malignancy can cause hypercalcemia through various mechanisms, such as the secretion of parathyroid hormone-related peptide (PTHrP).
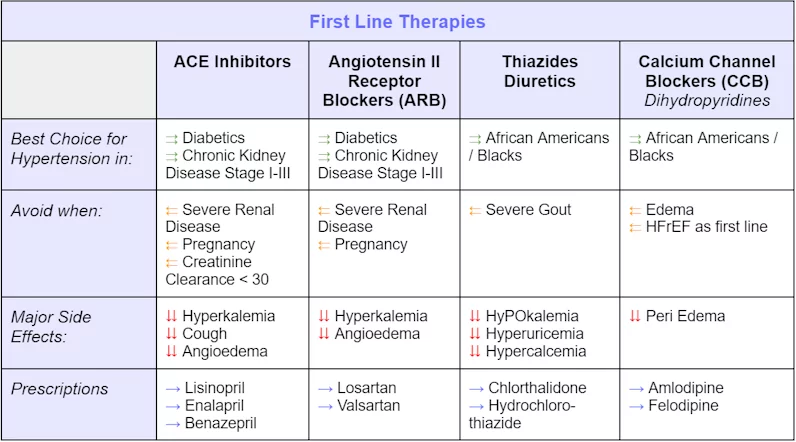
Other less common causes include certain medications (like thiazide diuretics), granulomatous diseases (such as sarcoidosis), vitamin D toxicity, and prolonged immobilization. Identifying the underlying cause is crucial for determining the long-term management strategy. Accurate diagnosis is essential to address the root cause of the imbalance.
Why First-Line Treatment Matters
Untreated hypercalcemia can lead to a range of complications, some of which can be quite serious. These include kidney stones, kidney dysfunction, bone pain, muscle weakness, fatigue, and neurological problems. In severe cases, hypercalcemia can even lead to cardiac arrhythmias and coma.
Prompt treatment is therefore essential to prevent these complications and restore normal calcium balance. The initial management of hypercalcemia focuses on rapidly lowering calcium levels to alleviate symptoms and prevent further organ damage. This is precisely where the first-line treatment comes into play.
Early intervention is crucial to prevent long-term damage and improve the patient's overall prognosis. Addressing the issue quickly can significantly enhance the quality of life and reduce the risk of severe health issues.
The Power of Hydration: Saline to the Rescue
The cornerstone of initial management is intravenous (IV) saline hydration. Administering large volumes of normal saline (0.9% sodium chloride) helps to dilute the calcium concentration in the blood. This dilution reduces the immediate impact of high calcium levels on the body's systems.
Furthermore, saline promotes calcium excretion through the kidneys. The increased fluid volume delivered intravenously encourages the kidneys to filter and eliminate excess calcium in the urine. This process is known as forced diuresis and is essential in the initial stages of hypercalcemia management.
Hydration helps protect the kidneys from damage caused by high calcium concentrations. Maintaining adequate hydration is critical for overall kidney health and function.
Calcitonin and Bisphosphonates: The Next Steps
While saline hydration is crucial, it's often not enough to completely resolve hypercalcemia, particularly in more severe cases. That's where medications like calcitonin and bisphosphonates come into play. These drugs work through different mechanisms to lower calcium levels and maintain them within a healthy range.
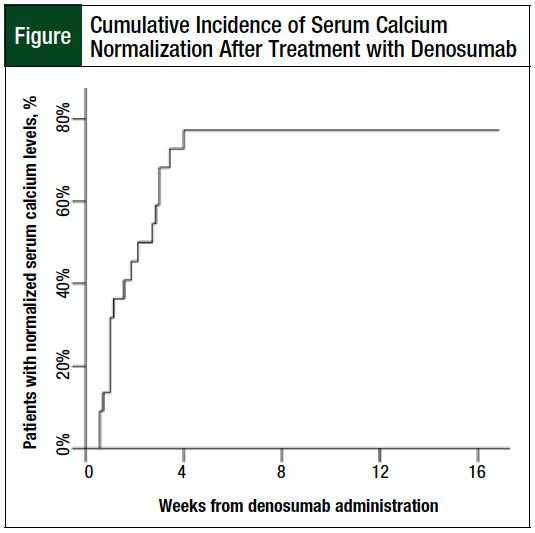
Calcitonin is a hormone that directly inhibits bone resorption, the process by which bone tissue is broken down and calcium is released into the bloodstream. Calcitonin acts quickly, usually within hours, but its effect is often short-lived. It is often used as a bridge to more long-lasting therapies.
Bisphosphonates, on the other hand, are a class of drugs that also inhibit bone resorption, but they do so through a different mechanism. Bisphosphonates are typically more effective than calcitonin in the long term, but they take several days to reach their maximum effect. Common examples include zoledronic acid and pamidronate.
Beyond First-Line: Addressing the Root Cause
While hydration, calcitonin, and bisphosphonates are the mainstays of initial treatment, it's equally important to identify and address the underlying cause of the hypercalcemia. This may involve further investigations, such as blood tests, imaging studies, and consultations with specialists like endocrinologists or oncologists.
If primary hyperparathyroidism is the culprit, surgery to remove the overactive parathyroid gland(s) may be necessary. For malignancy-associated hypercalcemia, treatment will focus on addressing the underlying cancer, which may include chemotherapy, radiation therapy, or other targeted therapies. Treating the source is crucial for sustained recovery.
Management of hypercalcemia also involves addressing contributing factors such as certain medications or vitamin D toxicity. Stopping the offending medication or correcting the vitamin D imbalance can help resolve the hypercalcemia.
Living Well with Hypercalcemia
Managing hypercalcemia is often a marathon, not a sprint. Patients may need to make lifestyle adjustments, such as increasing fluid intake, following a low-calcium diet, and avoiding medications that can worsen hypercalcemia. Regular monitoring of calcium levels is also essential to ensure that treatment remains effective and to detect any recurrence.
Support groups and online communities can provide valuable resources and encouragement for individuals living with hypercalcemia. Connecting with others who understand what you're going through can make a significant difference in your overall well-being. Sharing experiences helps people feel less alone.
Education is key to empowering individuals to manage their health effectively. Understanding the condition, its treatment, and potential complications can help patients make informed decisions and actively participate in their care. Awareness fosters empowerment and better health outcomes.
Looking Ahead: The Future of Hypercalcemia Treatment
Research continues to advance our understanding of hypercalcemia and to develop new and improved treatments. Novel therapies targeting specific pathways involved in calcium regulation are showing promise in clinical trials. Advances in medical science offer hope for better treatments.
Personalized medicine approaches, tailored to the individual patient's specific characteristics and underlying cause of hypercalcemia, are also gaining traction. This approach may lead to more effective and targeted therapies. Customizing treatment plans improves effectiveness.
Early detection and prompt treatment remain the cornerstones of successful hypercalcemia management. Regular check-ups and awareness of potential symptoms can help ensure that individuals receive the care they need to live healthy and fulfilling lives. Prevention and early intervention are always best.
Just like that wilting plant in the garden, with the right care and attention, the body can often be brought back into balance. Hypercalcemia, while a serious condition, is often manageable with prompt and appropriate treatment. Knowledge, vigilance, and a proactive approach can make all the difference in maintaining health and well-being.