What Is The Focus During The Preoperative Phase Of Surgery

The minutes before a surgeon's first incision are anything but quiet. Behind the sterile drapes and buzzing monitors, a complex orchestration of activity unfolds, setting the stage for a successful outcome. This delicate prelude, known as the preoperative phase, is far more than just waiting; it's a critical period focused on meticulous preparation and patient safety.
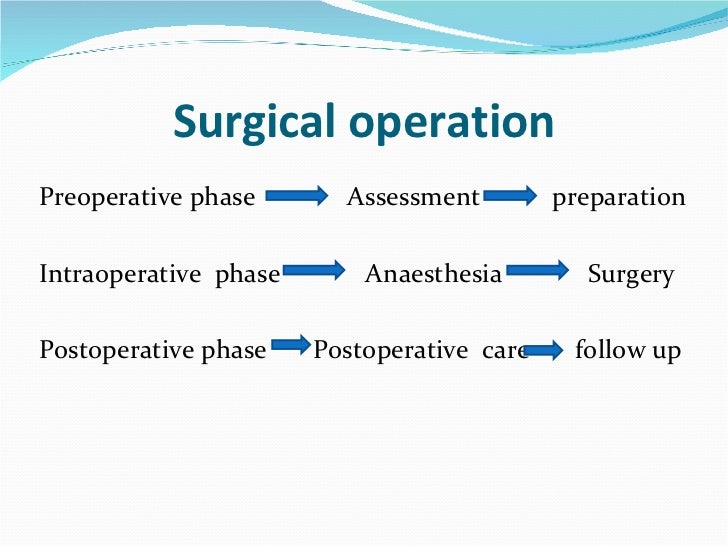
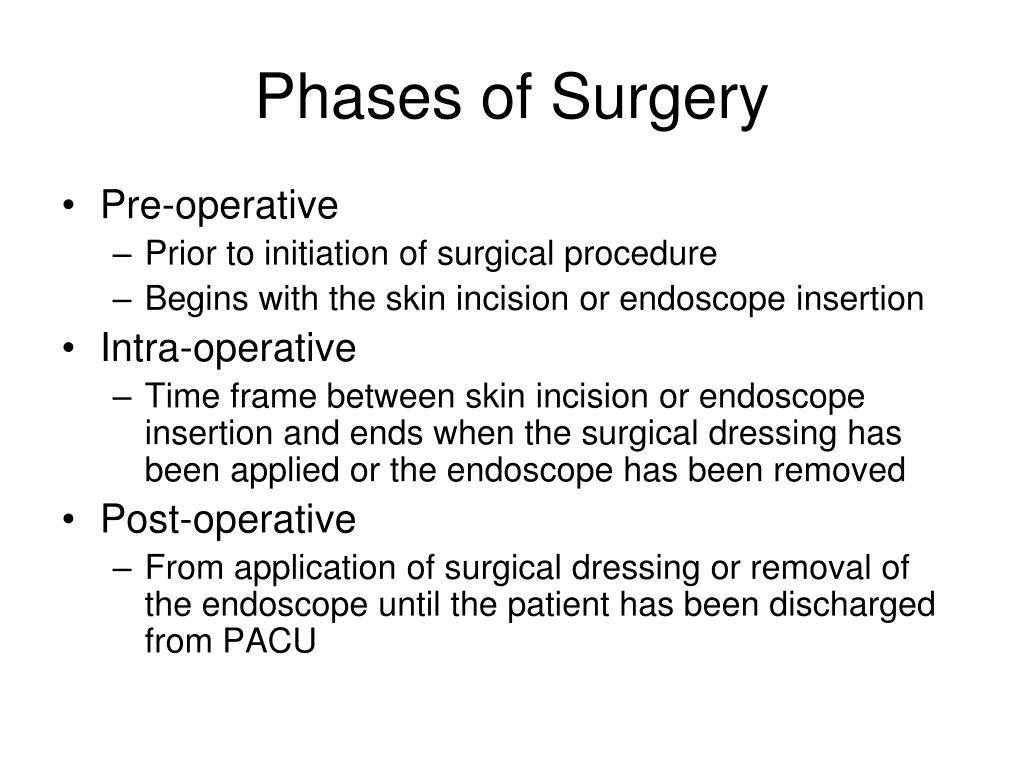
The preoperative phase is the period that begins when the decision for surgery is made and ends when the patient is transferred to the operating room table. Its core goal is to optimize the patient's condition, confirm readiness for surgery, and minimize potential risks. This includes thorough medical evaluation, detailed patient education, and psychological support, all aimed at ensuring the safest and most effective surgical experience possible. Poor preparation can lead to complications, delays, and increased morbidity, making this phase crucial for positive patient outcomes.
Comprehensive Patient Assessment: Laying the Groundwork
A cornerstone of the preoperative phase is a thorough assessment of the patient's overall health. This involves a detailed review of their medical history, including pre-existing conditions, allergies, and medications.
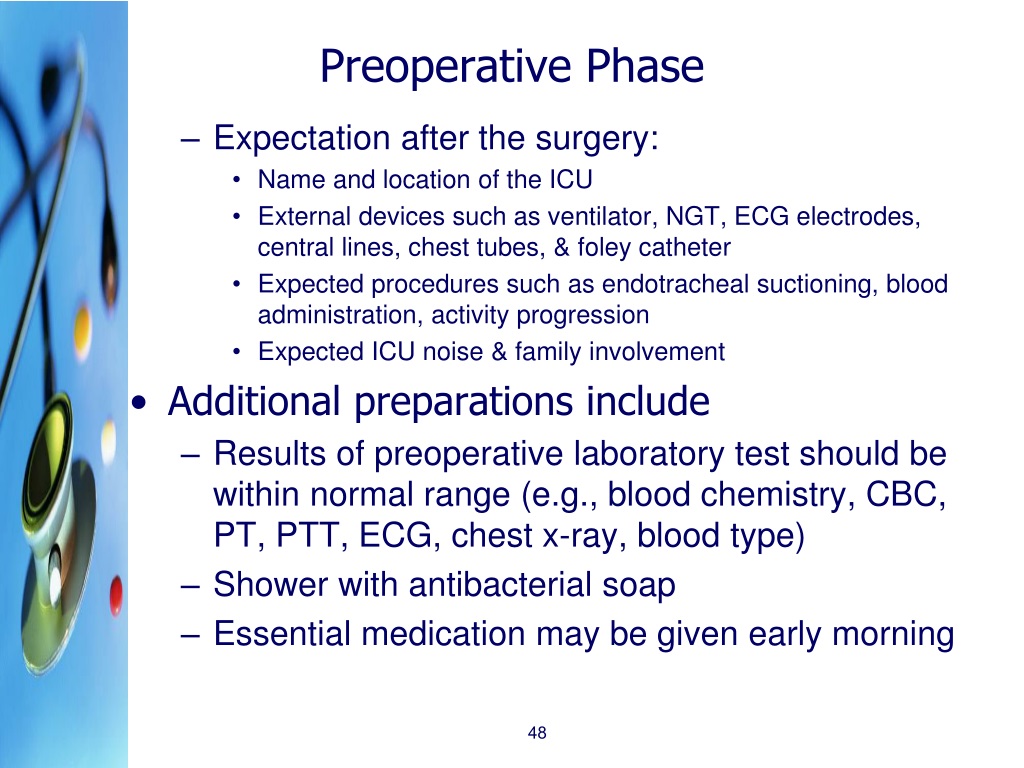
According to the American Society of Anesthesiologists (ASA), the goal is to identify any factors that could increase the risk of complications during or after surgery. This may involve ordering blood tests, electrocardiograms (ECGs), and other diagnostic tests to evaluate organ function and identify potential problems.
Medication Management: A Critical Balancing Act
Managing a patient's medications is a delicate balancing act in the preoperative phase. Some medications, such as blood thinners, may need to be adjusted or discontinued to reduce the risk of bleeding during surgery.
Conversely, other medications, such as those for chronic conditions like diabetes or heart disease, need to be carefully managed to ensure the patient remains stable. The surgeon, anesthesiologist, and primary care physician often collaborate to make these decisions, tailoring the medication plan to the individual patient's needs.
Informed Consent and Patient Education: Empowering the Patient
Obtaining informed consent is a crucial ethical and legal requirement. Patients must understand the nature of the surgery, the potential risks and benefits, and the alternative treatment options available.
This process involves a detailed discussion between the surgeon and the patient, allowing the patient to ask questions and express any concerns. Effective patient education extends beyond informed consent, providing patients with clear instructions on how to prepare for surgery and what to expect during the recovery period.
According to the Agency for Healthcare Research and Quality (AHRQ), well-informed patients are more likely to adhere to postoperative instructions and experience better outcomes.
Addressing Anxiety and Providing Psychological Support
Surgery can be a stressful experience, and many patients experience anxiety in the preoperative phase. Providing psychological support is an essential component of patient care.
This can involve simple measures such as providing reassurance and answering questions, or more formal interventions such as counseling or medication. Creating a calm and supportive environment can help patients feel more relaxed and confident going into surgery.
The "Time Out" Procedure: Ensuring Accuracy and Safety
The "time out" procedure is a final safety check performed immediately before the surgery begins. This involves the entire surgical team verifying the patient's identity, the correct surgical site, and the planned procedure.
This step, recommended by organizations like the World Health Organization (WHO), is designed to prevent wrong-site surgery and other errors that can have devastating consequences. It is a critical safeguard against human error and a testament to the importance of meticulous attention to detail in the preoperative phase.
Optimizing Patient Positioning and Equipment Readiness
Proper patient positioning is essential for both surgical access and patient safety. The surgical team carefully positions the patient to ensure optimal visualization of the surgical site while minimizing the risk of nerve damage or pressure ulcers.
Furthermore, all necessary equipment, including surgical instruments, anesthesia machines, and monitoring devices, must be checked and readily available. A well-prepared operating room contributes to a smooth and efficient surgical procedure.
The Role of Technology: Enhancing Preoperative Care
Technology plays an increasingly important role in the preoperative phase. Electronic health records (EHRs) allow for seamless access to patient information, facilitating better communication and coordination among healthcare providers.
Computerized order entry systems help to prevent medication errors and ensure that patients receive the correct medications at the correct doses. Furthermore, telemedicine can be used to conduct preoperative assessments remotely, improving access to care for patients in rural areas or those with limited mobility.
"The preoperative phase is not merely a waiting period, but an active process of optimizing the patient for surgery," states Dr. Emily Carter, Chief of Surgery at University Hospital.
Looking Ahead: Continuous Improvement in Preoperative Care
The field of preoperative care is constantly evolving, with ongoing research focused on identifying new ways to improve patient outcomes. Future directions include developing personalized preoperative care plans based on individual patient risk factors and utilizing artificial intelligence to predict and prevent complications.
By continuously refining our approach to the preoperative phase, we can ensure that patients receive the best possible care and achieve the best possible outcomes from their surgical procedures. The commitment to excellence in preoperative care ultimately translates to safer surgeries and improved patient well-being.