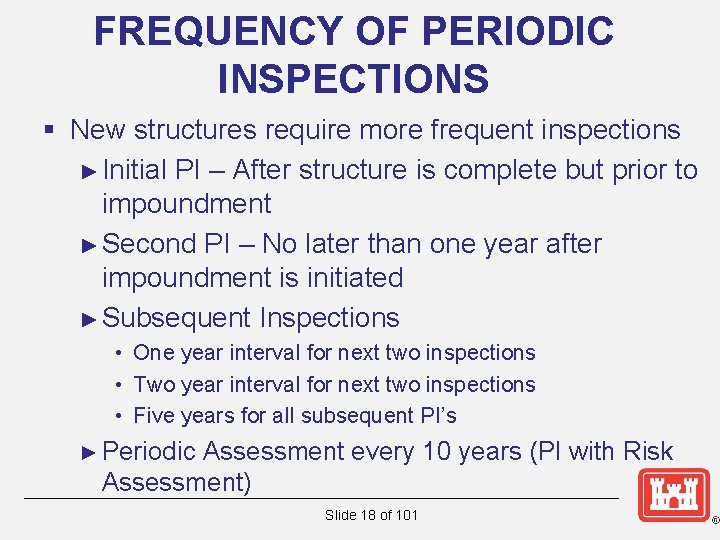
Which Establishment May Require More Frequent Inspections

Urgent action is underway to increase the frequency of inspections for nursing homes across several states, driven by a surge in reported safety violations and concerns over resident well-being. The changes could impact thousands of facilities and millions of residents nationwide.
This shift comes after a recent federal audit revealed systemic failures in current inspection protocols, leading to overlooked deficiencies and potential harm to vulnerable residents. The audit, conducted by the Office of Inspector General (OIG), identified significant shortcomings in staffing oversight, infection control, and emergency preparedness.
Mounting Evidence Demands Change
The catalyst for the increased scrutiny is the OIG report, which analyzed inspection data from the past three years. It revealed that nearly 40% of nursing homes cited for serious deficiencies were not re-inspected within the mandated timeframe. This delay allowed violations to persist, jeopardizing resident safety and quality of care.
The report highlighted instances where inadequate staffing levels directly contributed to resident neglect and increased risk of falls and medication errors. Furthermore, lapses in infection control protocols were linked to outbreaks of COVID-19 and other infectious diseases, resulting in preventable hospitalizations and deaths.
Who: Nursing homes, specifically those with a history of violations or located in states with weaker oversight. What: More frequent inspections, potentially unannounced, focusing on staffing levels, infection control, and emergency preparedness. Where: Initially targeting states identified by the OIG report as having the most significant deficiencies in their inspection programs. When: Implementation is expected to begin within the next quarter, with a phased rollout across different regions. How: Increased funding for state inspection agencies, enhanced training for inspectors, and the use of data analytics to identify high-risk facilities.
States Respond to Federal Pressure
Several states, including California, New York, and Florida, have already announced plans to implement more stringent inspection protocols. These measures include increasing the number of annual inspections, conducting unannounced visits, and imposing stricter penalties for violations. States will receive federal grants to support these initiatives.
California's Department of Public Health is proposing legislation to mandate annual inspections for all nursing homes, regardless of their prior inspection history. New York is focusing on enhancing training for inspectors to better identify and address subtle signs of neglect and abuse. Florida plans to increase the frequency of unannounced inspections, particularly for facilities with a history of violations.
The increased inspections may include closer scrutiny of staff-to-resident ratios, which the OIG report identified as a critical factor in determining the quality of care. Facilities that consistently fail to meet minimum staffing requirements could face fines, temporary suspension of admissions, or even closure.
Industry Concerns and Resident Advocacy
The nursing home industry has expressed concerns about the potential financial burden of increased inspections and the availability of qualified staff to meet the higher standards. The American Health Care Association (AHCA), a leading industry trade group, acknowledged the need for improvements but cautioned against overly burdensome regulations.
Resident advocacy groups, such as the National Consumer Voice for Quality Long-Term Care, have applauded the move towards more frequent inspections. They argue that increased oversight is essential to protect vulnerable residents and ensure they receive the care they deserve.
“This is a crucial step towards holding nursing homes accountable and ensuring the safety and well-being of residents,” said Robyn Grant, Director of Public Policy at the National Consumer Voice.
Focus Areas: Staffing, Infection, and Emergency Preparedness
Inspections will primarily focus on three key areas: staffing levels, infection control protocols, and emergency preparedness plans. The goal is to identify and address deficiencies before they lead to serious harm or neglect. The Centers for Medicare & Medicaid Services (CMS) is providing guidance to states on how to conduct more effective inspections in these areas.
Staffing Levels
Inspectors will be reviewing staffing schedules to ensure that facilities meet minimum staffing requirements for nurses and certified nursing assistants (CNAs). They will also be observing staff interactions with residents to assess the quality of care provided.
Infection Control
Facilities will be assessed on their adherence to infection control protocols, including hand hygiene, isolation procedures, and the use of personal protective equipment (PPE). Inspectors will also be reviewing facilities' plans for preventing and managing outbreaks of infectious diseases.
Emergency Preparedness
Inspectors will be evaluating facilities' emergency preparedness plans, including their procedures for responding to natural disasters, power outages, and other emergencies. They will also be assessing facilities' ability to evacuate residents safely in the event of an emergency.
Next Steps and Ongoing Developments
CMS is expected to issue further guidance to states in the coming weeks, outlining specific requirements for increased inspections and enforcement. State agencies are actively developing implementation plans and training their inspectors to conduct more thorough and effective evaluations.
Residents and their families are encouraged to report any concerns about the quality of care or safety conditions in nursing homes to state authorities. Ongoing monitoring and public awareness will be crucial to ensuring the success of these initiatives and protecting vulnerable residents.
The changes in inspection frequency signify a crucial step toward accountability and enhanced protection for nursing home residents. Continued vigilance and proactive measures will be necessary to sustain improvements in long-term care facilities nationwide.

![Which Establishment May Require More Frequent Inspections Crane Inspection Requirements [With Checklists] | BigRentz](https://acropolis-wp-content-uploads.s3.us-west-1.amazonaws.com/frequent-crane-inspection-checklist.webp)