Which Is Incorrect About Hepatitis A Infection
A surge in Hepatitis A cases across several states has triggered public health alerts and renewed focus on this preventable liver disease. However, amidst the genuine concerns, a parallel wave of misinformation is spreading, muddying understanding and potentially hindering effective prevention efforts. Sorting fact from fiction is crucial to protecting vulnerable populations and controlling outbreaks.
This article aims to dissect the most common misconceptions surrounding Hepatitis A infection. We'll rely on data and guidance from organizations like the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO). Our goal is to provide clarity, debunk inaccurate claims, and empower readers with evidence-based knowledge to make informed decisions about their health.
Myth 1: Hepatitis A is a Chronic Illness Like Hepatitis B or C
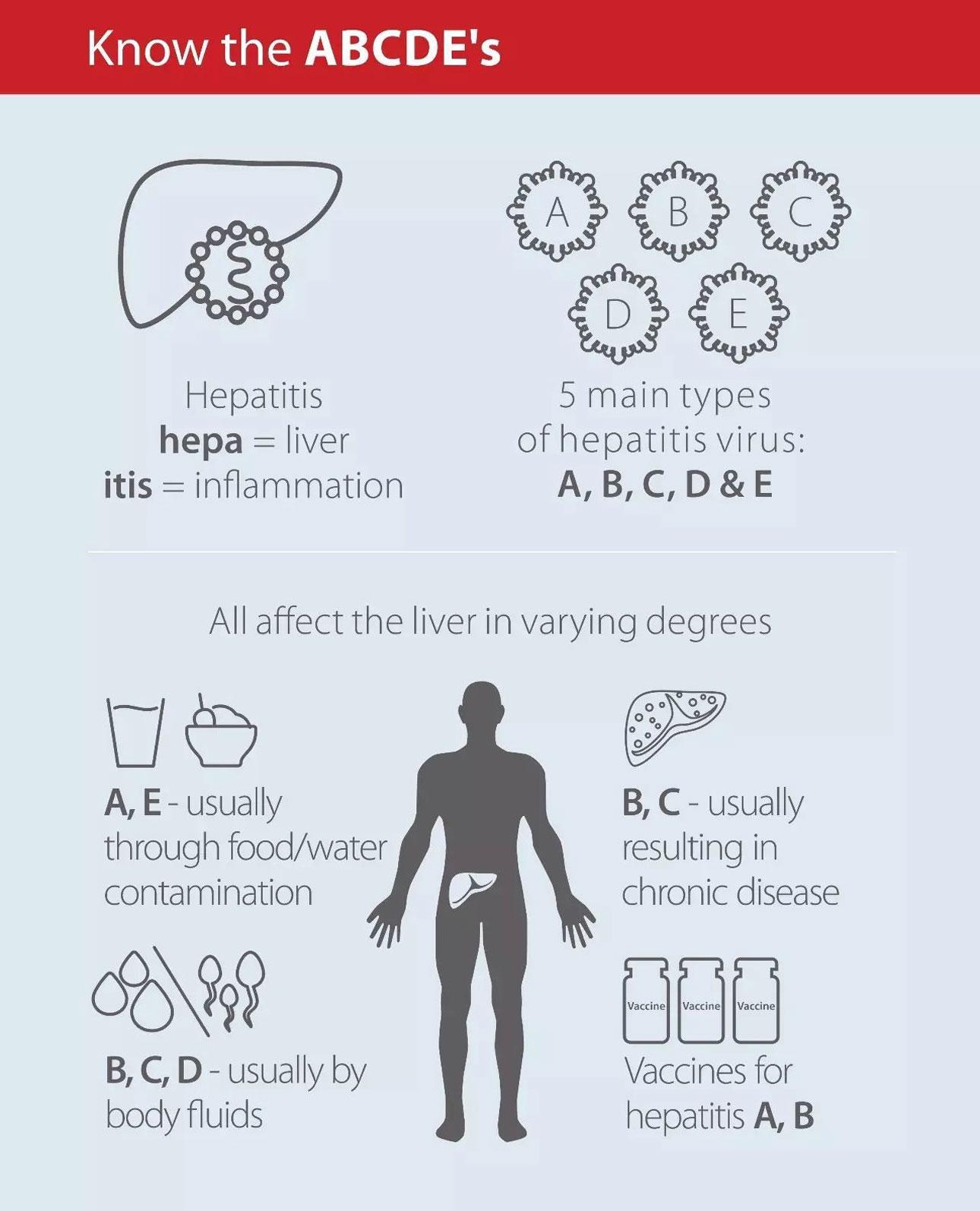
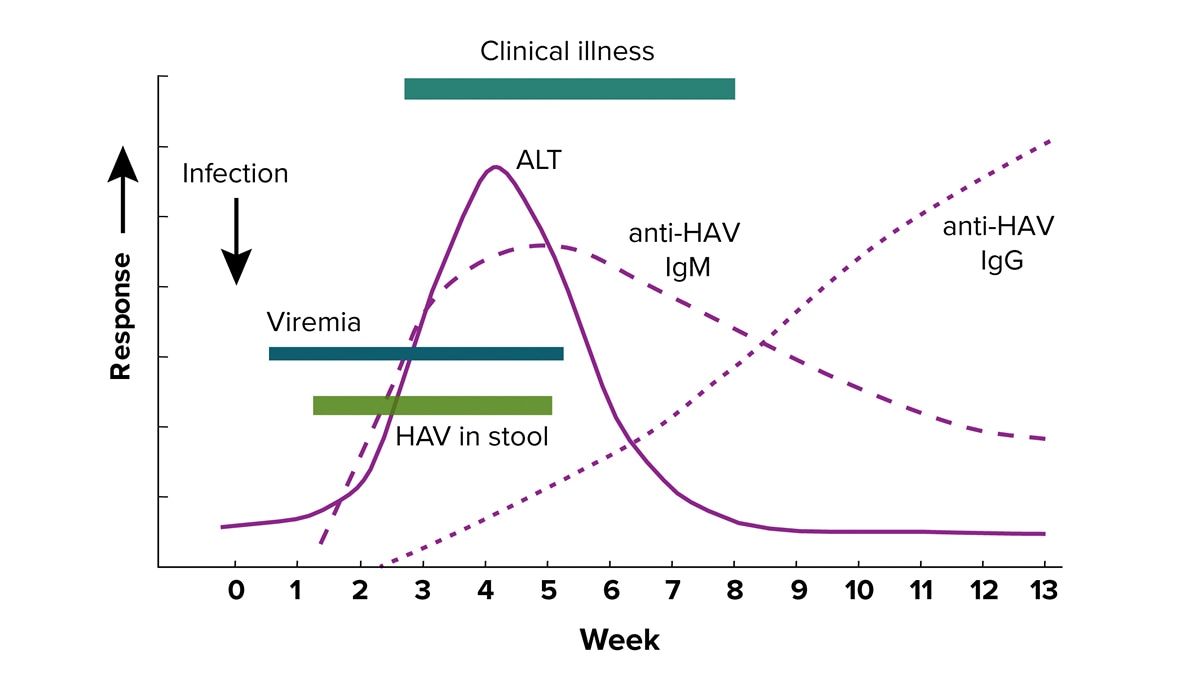
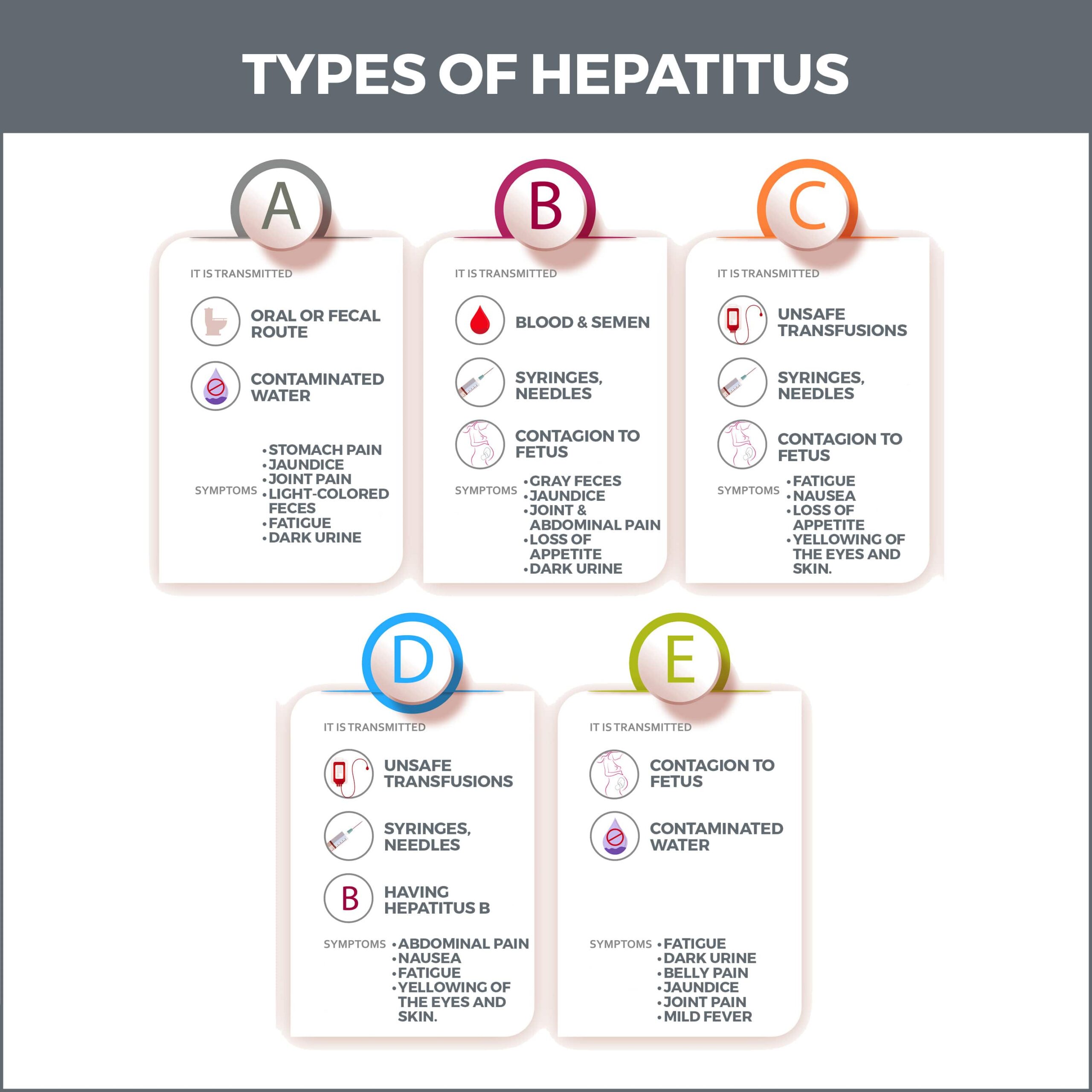
One of the most persistent and damaging myths is that Hepatitis A leads to chronic liver disease. Hepatitis A is almost always an acute, short-term illness. Unlike Hepatitis B and C, it does not cause chronic infection or long-term liver damage in the vast majority of cases.
The CDC clearly states that Hepatitis A infection resolves on its own within a few weeks to several months. The body clears the virus, and individuals develop lifelong immunity.
Rare but Serious Complications
While chronic infection is not a concern, it's important to acknowledge rare, severe complications. In very rare instances, Hepatitis A can cause acute liver failure, particularly in individuals with pre-existing liver conditions. This condition, known as fulminant hepatitis, requires immediate medical attention and may necessitate a liver transplant.
Myth 2: Only People with Poor Hygiene Get Hepatitis A
While poor hygiene can certainly contribute to the spread of Hepatitis A, it is not the sole determinant. This myth leads to stigmatization and a misunderstanding of transmission routes. Anyone can contract Hepatitis A, regardless of their personal hygiene practices.
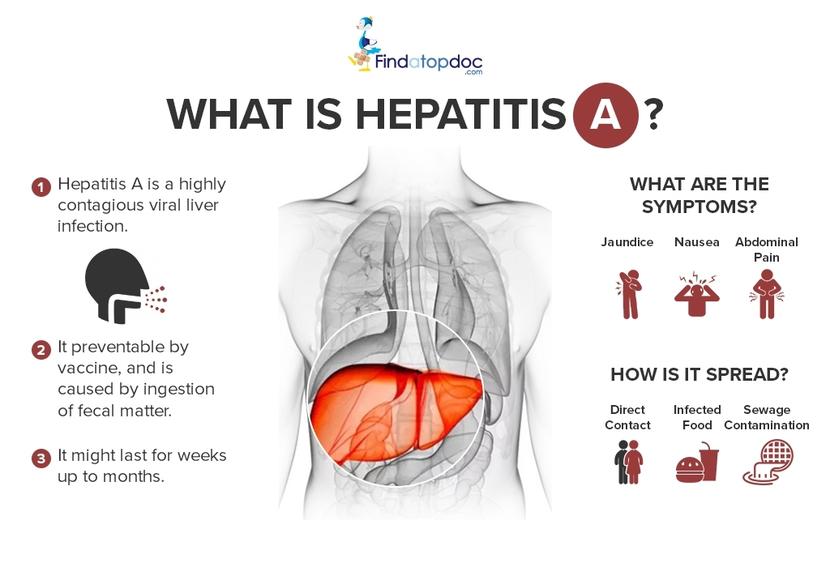
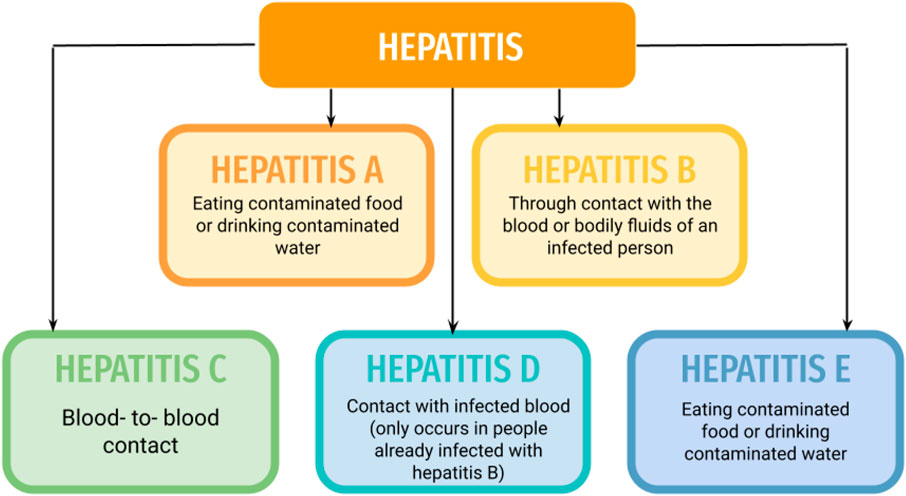
The virus is primarily transmitted through the fecal-oral route. This means that someone ingests the virus after coming into contact with the feces of an infected person.
This can happen through contaminated food or water, or through close personal contact. Outbreaks have been linked to contaminated produce, shellfish, and even food handlers who are infected.
Myth 3: There's No Treatment for Hepatitis A
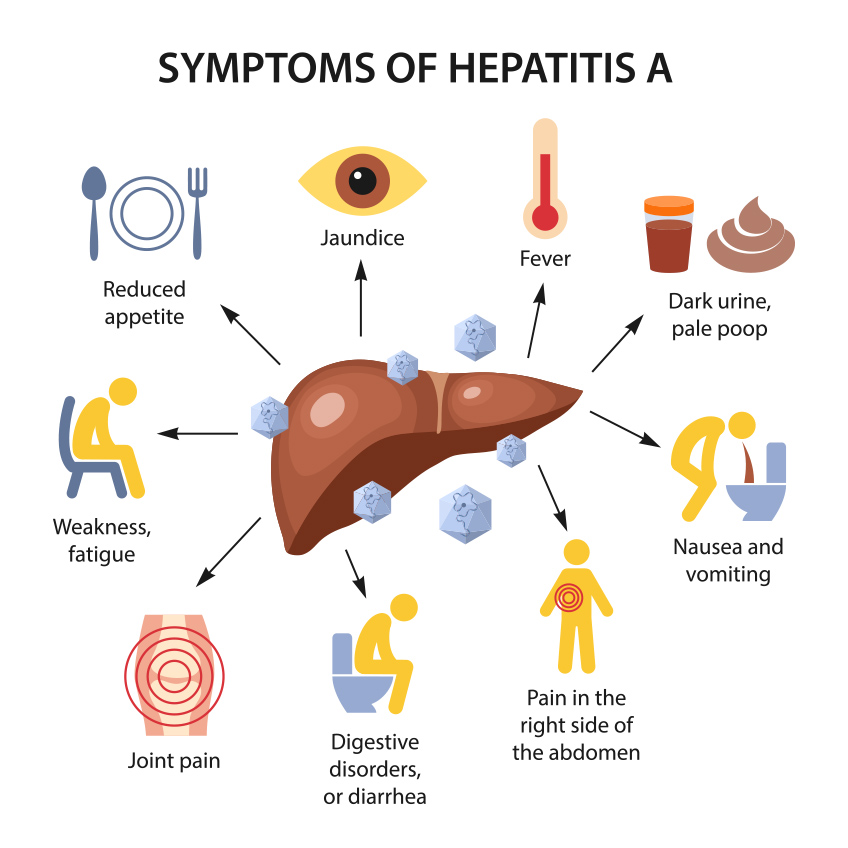
While there's no specific antiviral medication to cure Hepatitis A, this doesn't mean there's no treatment available. Supportive care is crucial for managing symptoms and preventing complications. This includes rest, adequate hydration, and a healthy diet.
In severe cases, hospitalization may be necessary to manage dehydration, nausea, and other symptoms. Medications can also be used to alleviate nausea and vomiting. Avoiding alcohol and other substances that can stress the liver is also important.
Myth 4: You Can Only Get Hepatitis A Once
This statement contains a partial truth but needs clarification. Once you've had Hepatitis A, you develop lifelong immunity to the virus. This means you cannot be infected with the same strain of Hepatitis A again.
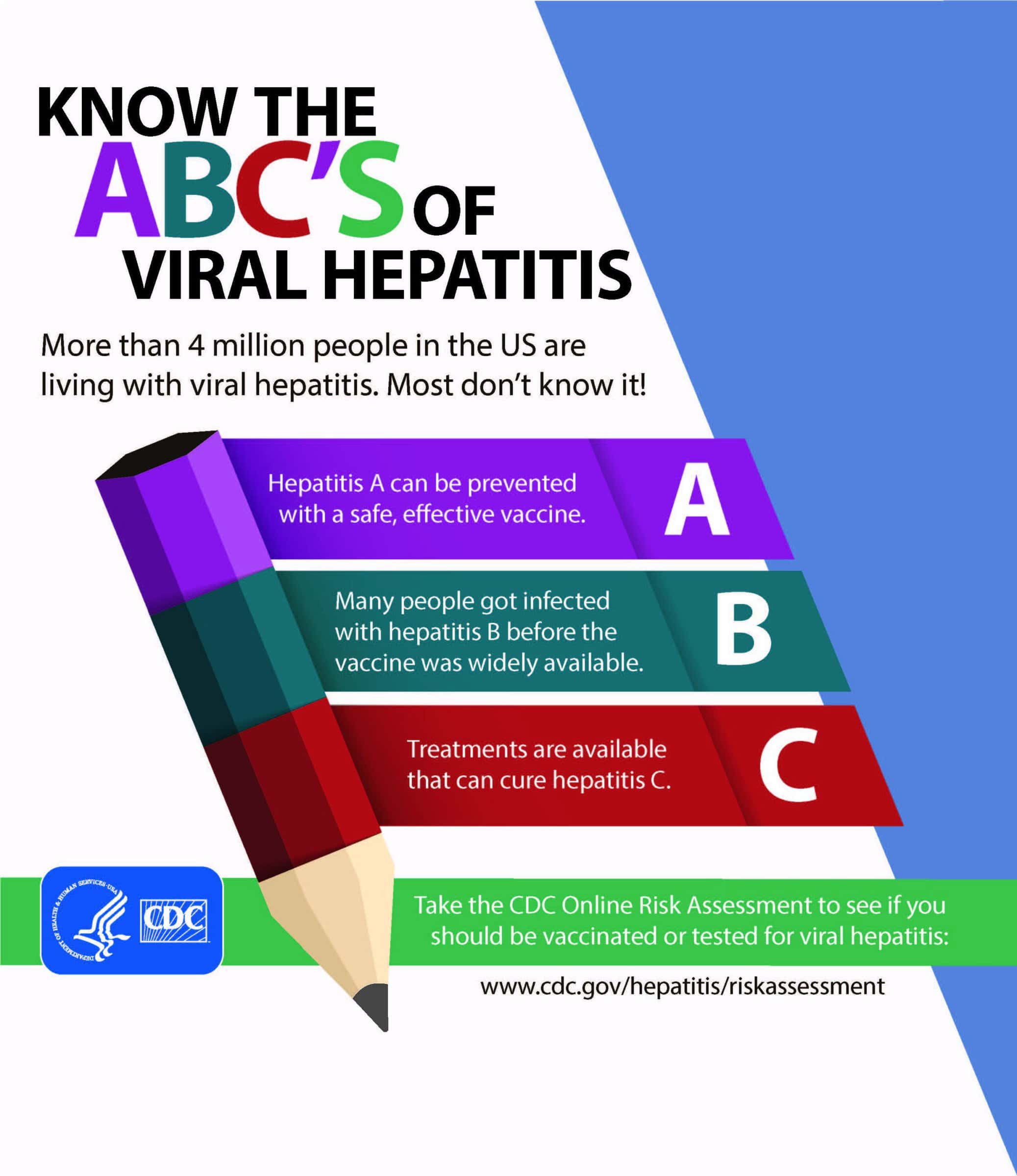
However, it's essential to differentiate Hepatitis A from other types of viral hepatitis (B, C, D, and E). Immunity to Hepatitis A does not protect you from these other viruses. Vaccination against Hepatitis A and Hepatitis B is available and recommended for certain groups.
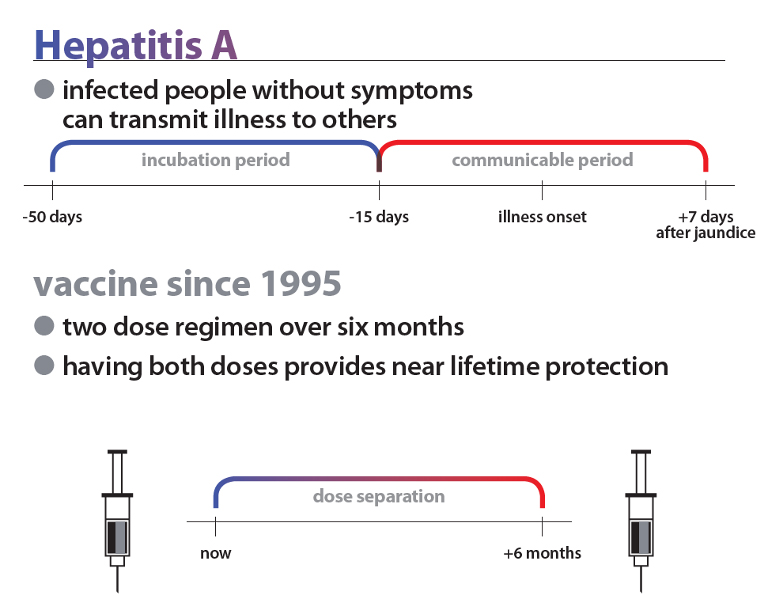
Myth 5: Vaccination is Only Necessary During an Outbreak
While vaccination is certainly crucial during an outbreak to curb its spread, it's not the only time it's recommended. The CDC recommends routine Hepatitis A vaccination for all children at age 1 year. Vaccination is also recommended for adults at increased risk.
This includes people who travel to countries where Hepatitis A is common, men who have sex with men, people who use illicit drugs, and those with chronic liver disease. Vaccination provides the best protection against Hepatitis A infection.
The Importance of Accurate Information
Combating misinformation is crucial for effective public health responses. Spreading awareness about the true nature of Hepatitis A, its transmission routes, and the availability of preventive measures is essential. This empowers individuals to make informed choices and protects vulnerable populations.
Public health officials and healthcare providers play a vital role in disseminating accurate information and addressing concerns. By working together, we can dispel myths and promote a better understanding of Hepatitis A prevention and management.
Looking Ahead: Strengthening Prevention Efforts
Hepatitis A remains a preventable disease. Continued efforts to improve sanitation, promote vaccination, and educate the public are critical. Investment in public health infrastructure and accessible healthcare services is essential for protecting communities from future outbreaks.
The ongoing surveillance and reporting of Hepatitis A cases are also crucial. This allows public health agencies to identify outbreaks early and implement timely control measures. By staying informed and taking proactive steps, we can reduce the burden of Hepatitis A and protect public health.
Ultimately, understanding the truth about Hepatitis A, separating fact from harmful fiction, empowers individuals and communities to take appropriate preventive actions. This contributes to a healthier and more informed society.