Which Of The Following Is A Barrier To Shared Decision-making
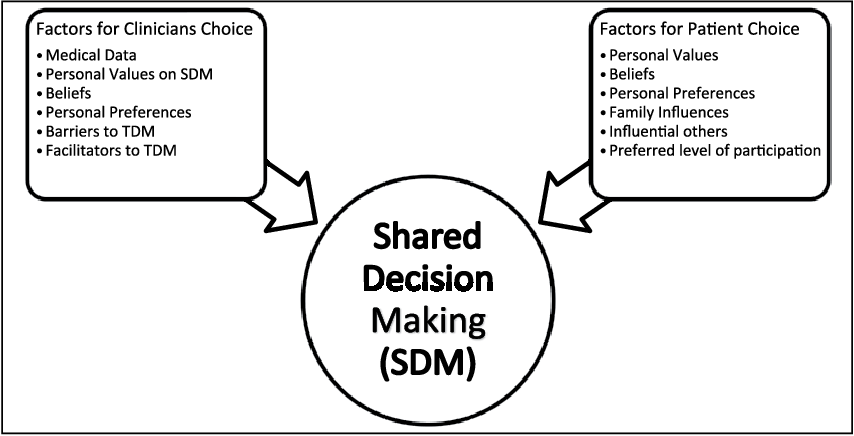
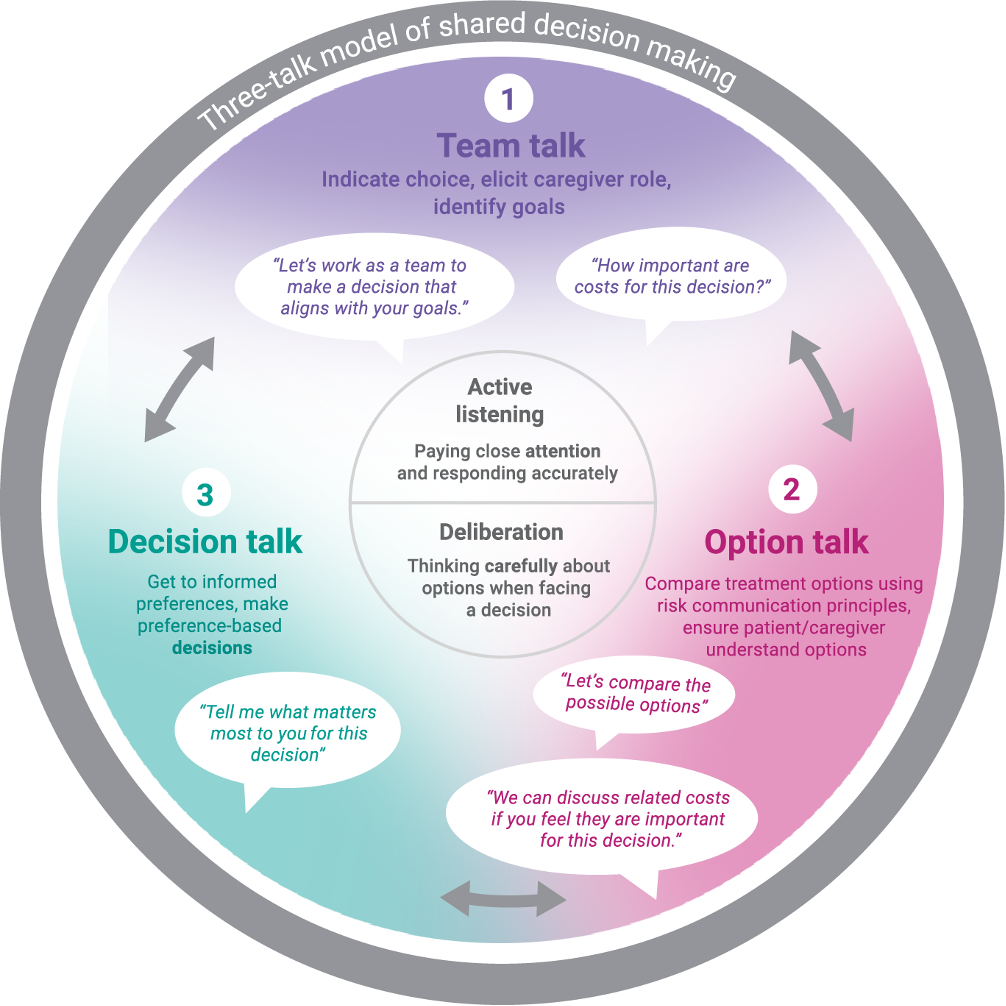
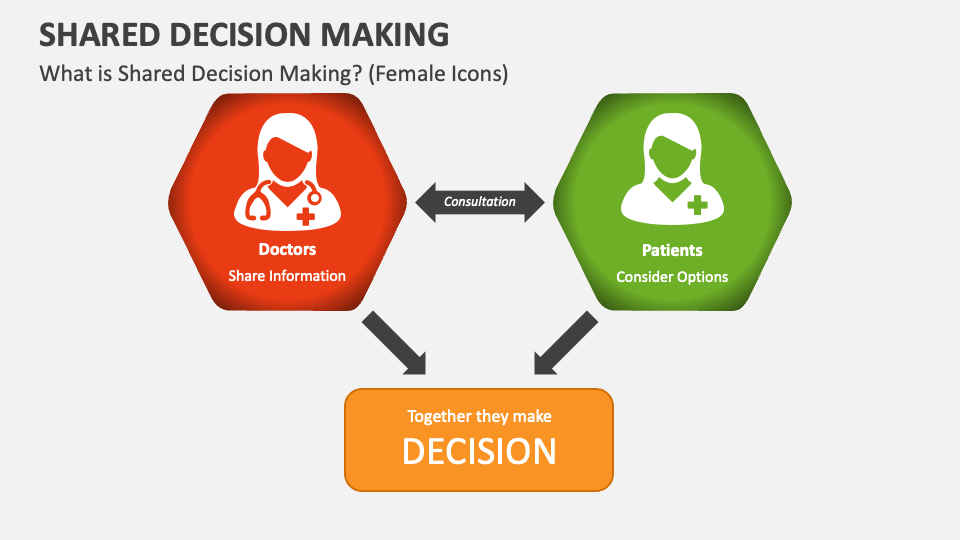
Shared decision-making (SDM), a cornerstone of patient-centered healthcare, aims to empower individuals to actively participate in choices regarding their health management. However, its widespread adoption faces numerous obstacles, hindering its full potential in improving patient outcomes and satisfaction. Identifying these barriers is crucial to developing effective strategies that promote genuine collaboration between patients and healthcare providers.
This article will explore the various barriers preventing shared decision-making in clinical settings. These challenges range from systemic limitations within healthcare systems to individual factors affecting both patients and practitioners. Understanding these impediments is essential to create a more equitable and effective healthcare landscape.
Systemic and Organizational Barriers
One of the most significant barriers is the pervasive time constraints faced by healthcare providers. In many clinical settings, doctors and nurses are burdened with heavy workloads and short appointment times, leaving insufficient opportunity for comprehensive discussions with patients about treatment options and their preferences. This lack of time can lead to rushed decisions and a feeling of being unheard among patients.
Healthcare system structures themselves can also impede SDM. Many institutions operate under a hierarchical model, where physicians are traditionally viewed as the primary decision-makers. This can create a culture that does not readily encourage patient participation, especially if those institutions do not have systemic support for the SDM.
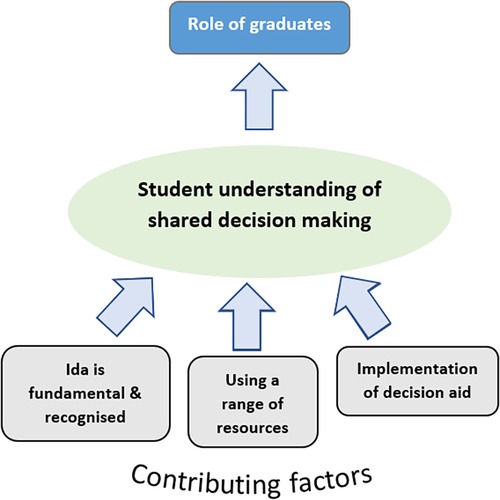
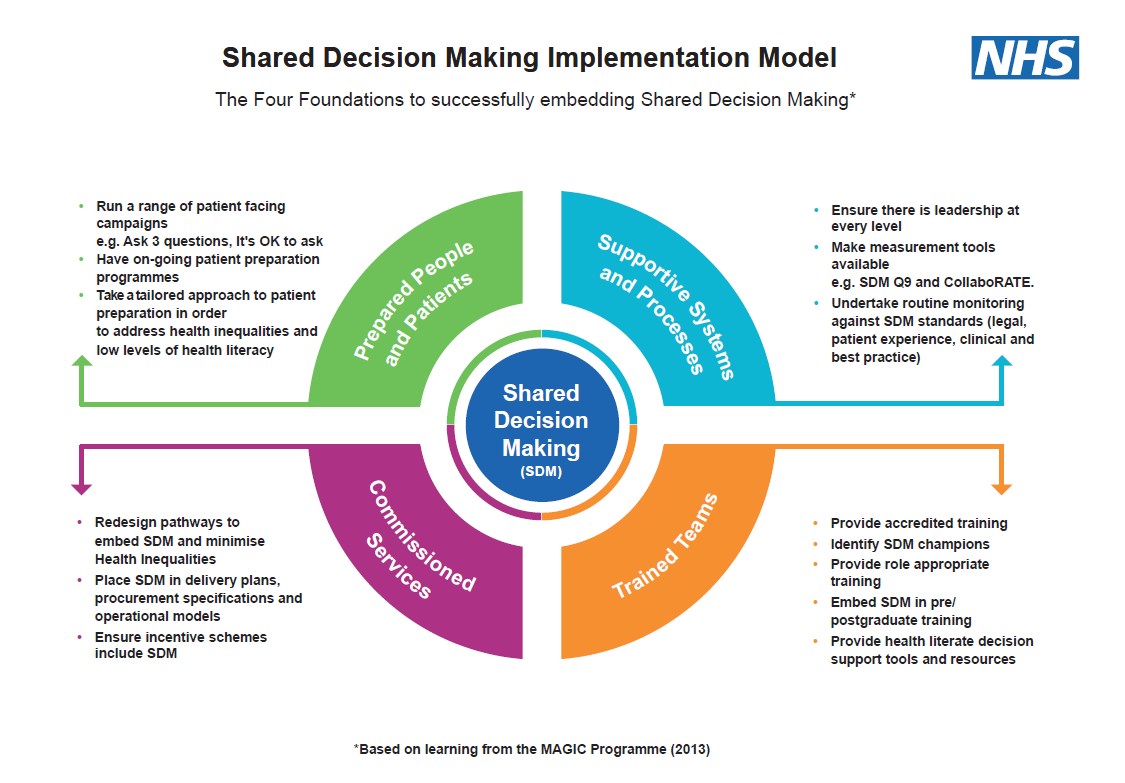
Furthermore, insufficient resources for SDM training and implementation represent a major challenge. Many healthcare professionals lack formal training in communication skills, shared decision-making techniques, and how to effectively incorporate patient values into treatment plans. Without dedicated resources and support, widespread adoption of SDM remains difficult.
Patient-Related Barriers
Patients themselves can present barriers to SDM. Some individuals may feel overwhelmed by medical information and lack the confidence to engage in complex medical discussions. This information asymmetry can lead to deference to the physician's judgment, even when the patient has reservations or preferences that are not addressed.
Health literacy is another critical factor. Patients with low health literacy may struggle to understand medical terminology, interpret treatment options, and assess the potential risks and benefits associated with each choice. This lack of understanding can make it difficult for them to participate meaningfully in decision-making.
Cultural and linguistic differences can also create significant barriers. Language barriers can hinder communication, while cultural beliefs and values may influence a patient's preferences and willingness to question medical advice. Healthcare providers must be sensitive to these differences and adapt their approach accordingly.
Provider-Related Barriers
On the provider side, certain attitudes and beliefs can hinder SDM. Some healthcare professionals may believe that they are best equipped to make decisions for their patients, often stemming from a paternalistic approach to medicine. This can lead to a reluctance to share control and actively involve patients in the decision-making process.
A lack of awareness or understanding of SDM is also a significant barrier. Some providers may not be fully aware of the benefits of SDM or may not know how to effectively implement it in their practice. This can result in a continuation of traditional, physician-centered decision-making models.
Fear of increased liability is another concern among some providers. They may worry that involving patients in decision-making could increase their legal risk, particularly if a patient makes a choice that ultimately leads to an unfavorable outcome. Addressing these concerns and providing legal support is crucial for promoting SDM.
The Impact and Moving Forward
Overcoming these barriers is critical for realizing the full potential of shared decision-making. Studies have shown that SDM can lead to improved patient satisfaction, increased adherence to treatment plans, and better health outcomes. By empowering patients to actively participate in their care, SDM can foster a sense of ownership and responsibility for their health.
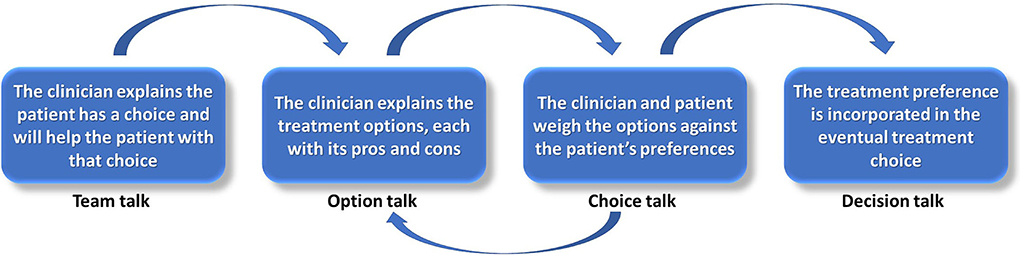
Addressing these barriers requires a multi-faceted approach. This includes implementing organizational changes to provide more time for patient-provider interactions. Enhanced SDM training for healthcare professionals will enable them to effectively communicate with patients and incorporate their values into treatment decisions.
Efforts to improve patient health literacy are also essential. Creating patient-friendly materials, providing language assistance, and addressing cultural differences can help empower patients to actively participate in their care. By acknowledging and addressing these various barriers, healthcare systems can promote a more patient-centered and equitable approach to healthcare.
The journey towards widespread adoption of SDM is ongoing. However, by recognizing and addressing the obstacles that hinder its implementation, healthcare providers and institutions can work together to create a future where patients are truly partners in their own healthcare journey. This shift toward patient-centered care is not only ethically sound but also has the potential to improve health outcomes and reduce healthcare costs in the long run.