Which Of The Following Is A Metabolic Function Of Skin

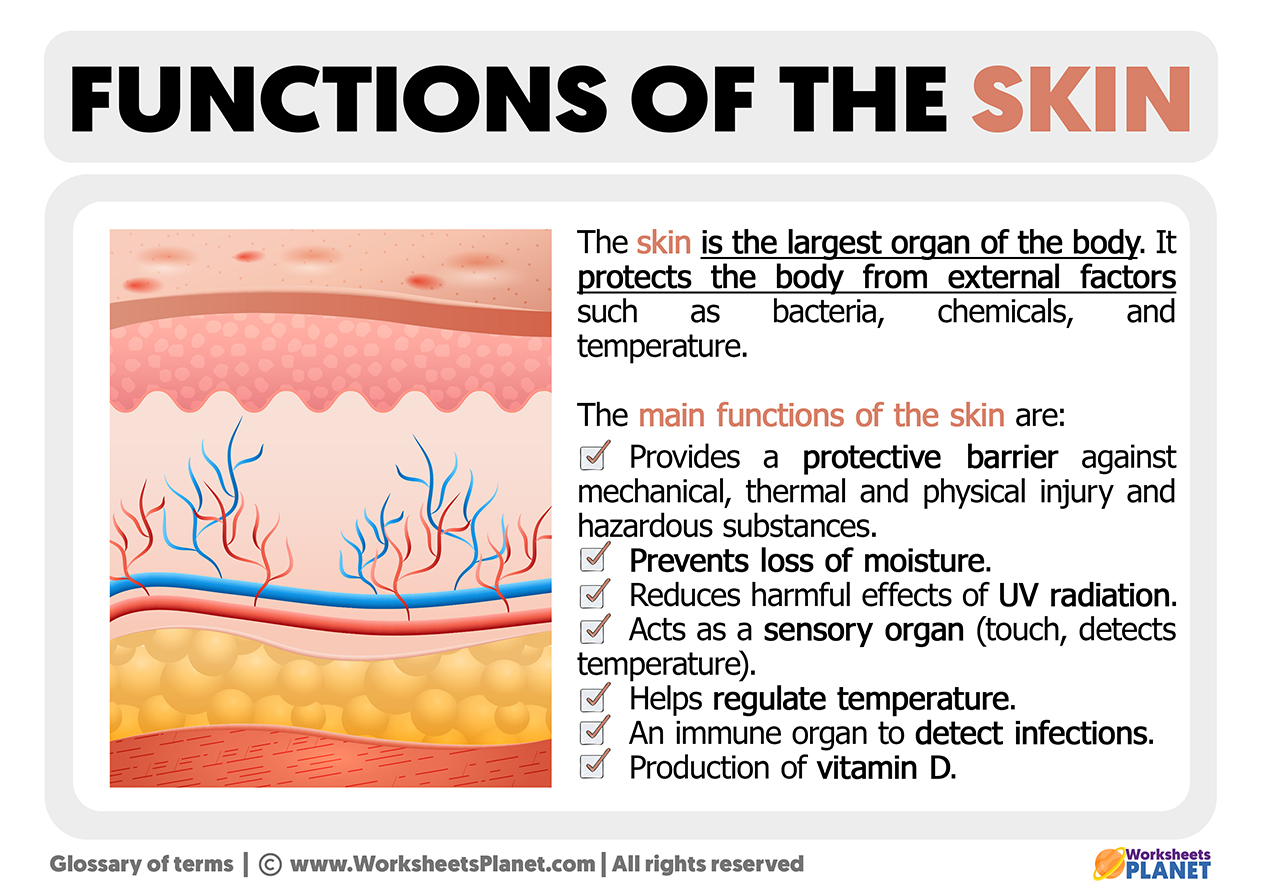
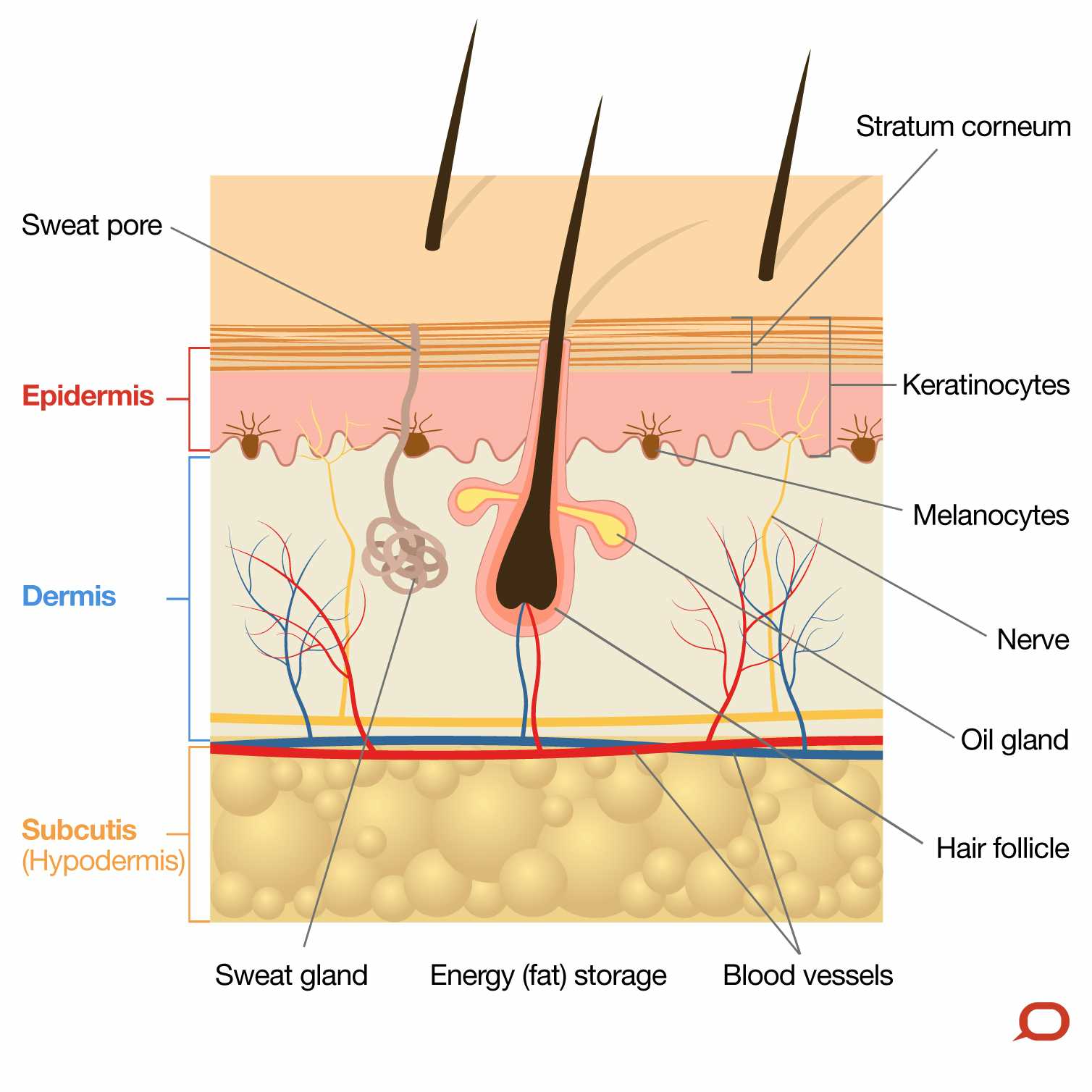
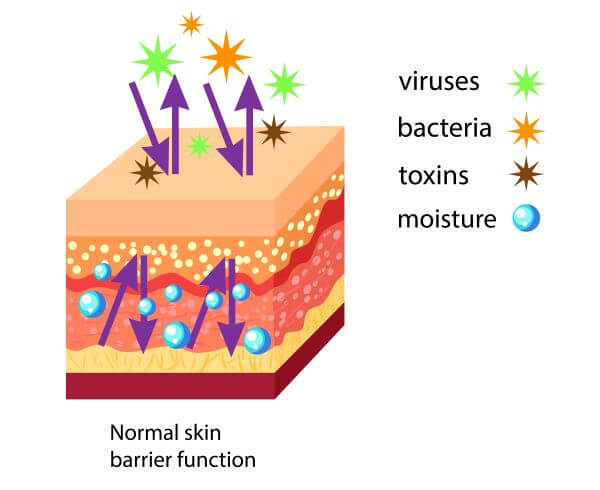
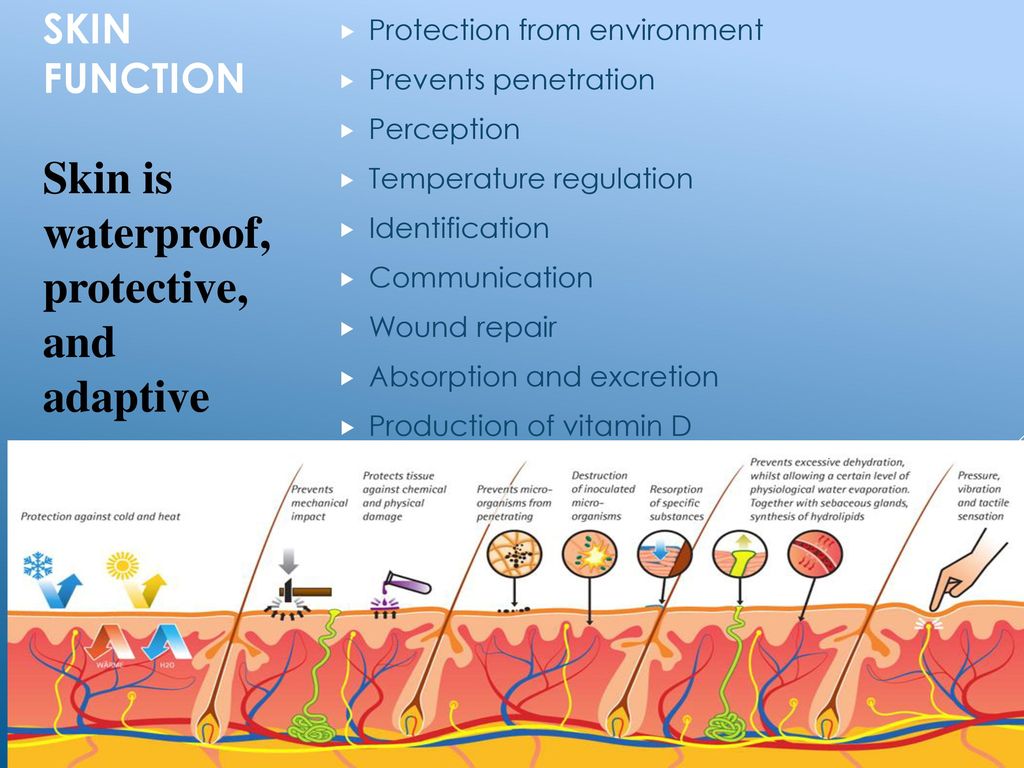
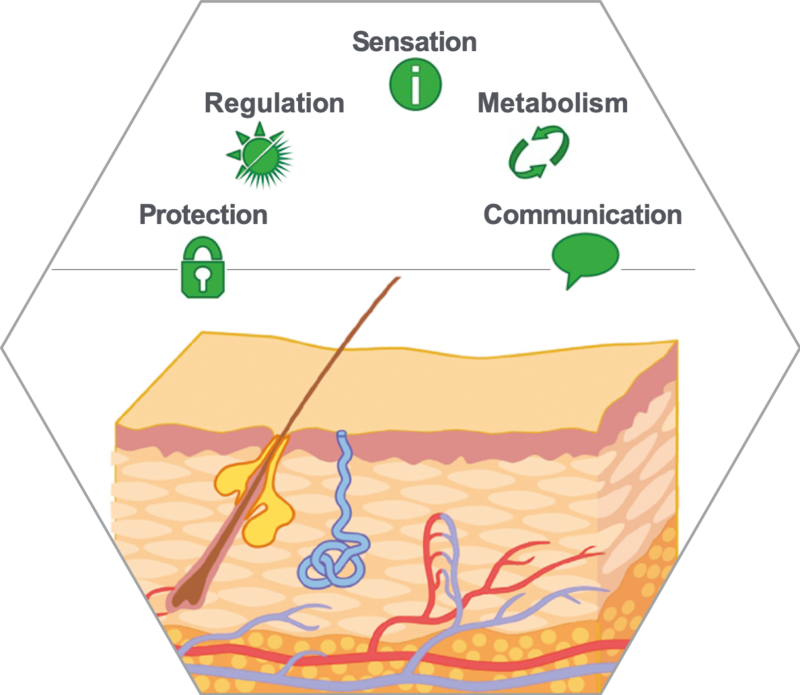
The skin, our largest organ, is often perceived as merely a protective barrier, shielding us from the external world. However, beneath its surface lies a complex metabolic landscape, actively participating in crucial bodily functions. Disentangling these metabolic processes is vital for understanding skin health, disease, and overall well-being.
This article delves into the metabolic functions of the skin, exploring its role in vitamin D synthesis, thermoregulation, detoxification, and immune response. We will examine scientific evidence and expert opinions to clarify which of these functions truly qualify as metabolic activities, and discuss their implications for maintaining a healthy integumentary system. Understanding these processes is crucial for developing effective strategies to prevent and treat skin-related disorders.
Vitamin D Synthesis: A Key Metabolic Role
Perhaps the most well-known metabolic function of the skin is its role in vitamin D synthesis. When exposed to ultraviolet B (UVB) radiation from sunlight, a cholesterol-based molecule in the skin, 7-dehydrocholesterol, is converted into previtamin D3. This previtamin D3 then undergoes further processing in the liver and kidneys to become the active form of vitamin D, calcitriol.
Vitamin D is essential for calcium absorption, bone health, and immune function. Deficiencies can lead to rickets in children and osteomalacia in adults. The skin's ability to synthesize vitamin D underscores its critical metabolic involvement in calcium homeostasis and skeletal integrity.
The Process in Detail
The conversion of 7-dehydrocholesterol to previtamin D3 is a photochemical reaction driven by UVB radiation. The amount of vitamin D produced depends on factors such as latitude, season, time of day, skin pigmentation, and sunscreen use. Individuals with darker skin pigmentation require more sun exposure to produce the same amount of vitamin D as those with lighter skin.
The synthesized previtamin D3 is not immediately active. It requires two hydroxylation steps: first in the liver to form 25-hydroxyvitamin D [25(OH)D], and then in the kidneys to form 1,25-dihydroxyvitamin D [1,25(OH)2D], or calcitriol. This final step is tightly regulated by parathyroid hormone (PTH) and calcium levels to maintain calcium homeostasis.
Thermoregulation: Beyond Metabolism?
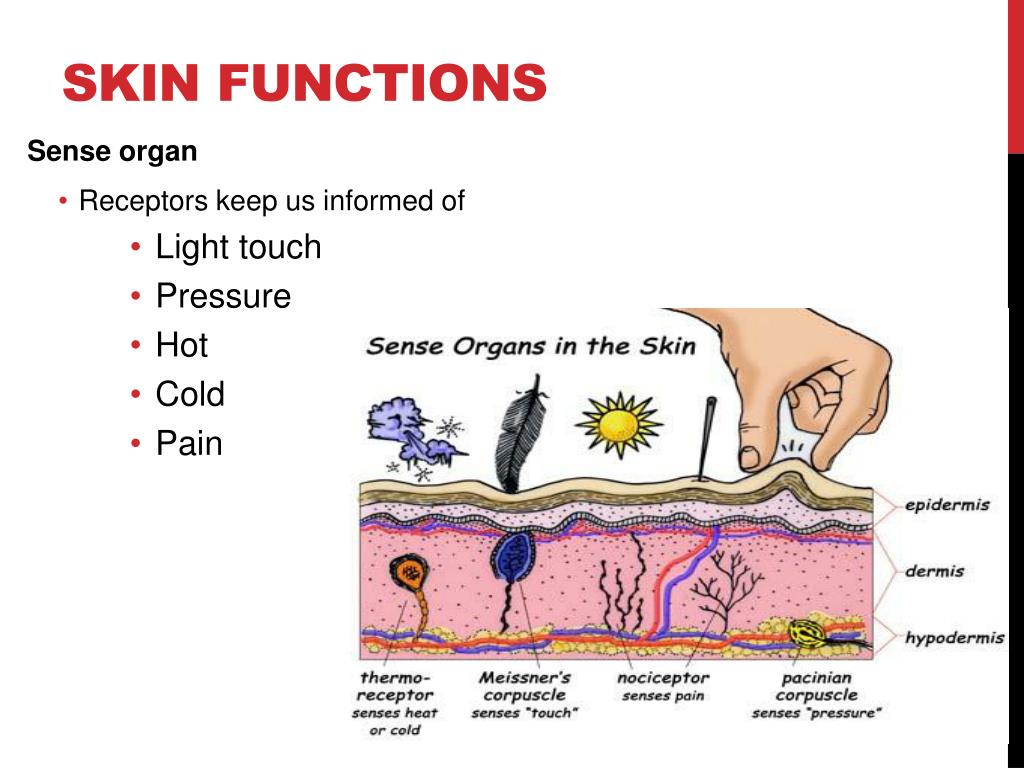
The skin plays a significant role in thermoregulation, helping the body maintain a stable internal temperature. This is achieved through various mechanisms, including sweating, vasodilation, and vasoconstriction. While essential for survival, the extent to which thermoregulation is a direct *metabolic* function of the skin is debated.
Sweating, for example, involves the production and secretion of sweat by eccrine sweat glands. This process requires energy and involves the active transport of ions and water. Vasodilation and vasoconstriction, controlled by the autonomic nervous system, alter blood flow to the skin, influencing heat loss or conservation.
Different Perspectives on Thermoregulation
Some argue that thermoregulation, while involving energy expenditure and active transport, is primarily a physiological rather than strictly metabolic function. Metabolic processes are generally understood as the chemical reactions occurring within cells to sustain life, whereas thermoregulation is a broader system-level response.
Others contend that the energy expenditure associated with sweating and the cellular processes involved in vasodilation and vasoconstriction qualify thermoregulation as a metabolic activity, albeit an indirect one. The debate highlights the complex interplay between physiology and metabolism in the skin.
Detoxification: Limited Metabolic Capacity
The skin has a limited capacity for detoxification, although it's often touted as a detoxifying organ. While some xenobiotics (foreign chemicals) can be eliminated through sweat, the skin's primary role is protection, not active detoxification like the liver or kidneys.
The skin expresses some enzymes involved in detoxification, such as cytochrome P450 enzymes, but their activity is relatively low compared to other organs. Therefore, the skin's contribution to systemic detoxification is minimal.
Challenging the "Detox" Myth
The idea that the skin can significantly detoxify the body is often promoted in marketing campaigns for various skin care products. However, scientific evidence supporting this claim is weak. While sweating can eliminate small amounts of toxins, it's primarily a mechanism for thermoregulation.
Over-reliance on the skin for detoxification can be misleading and may distract from addressing the root causes of toxin exposure or liver/kidney dysfunction. Focus should remain on supporting the body's primary detoxification organs for optimal health.
Immune Response: A Complex Metabolic Interaction
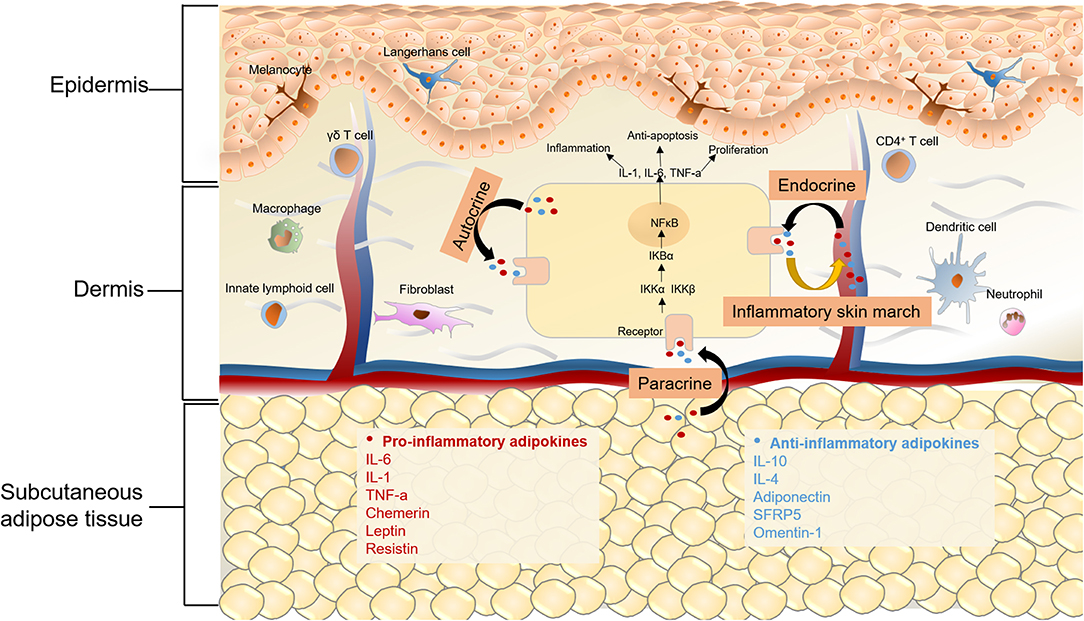
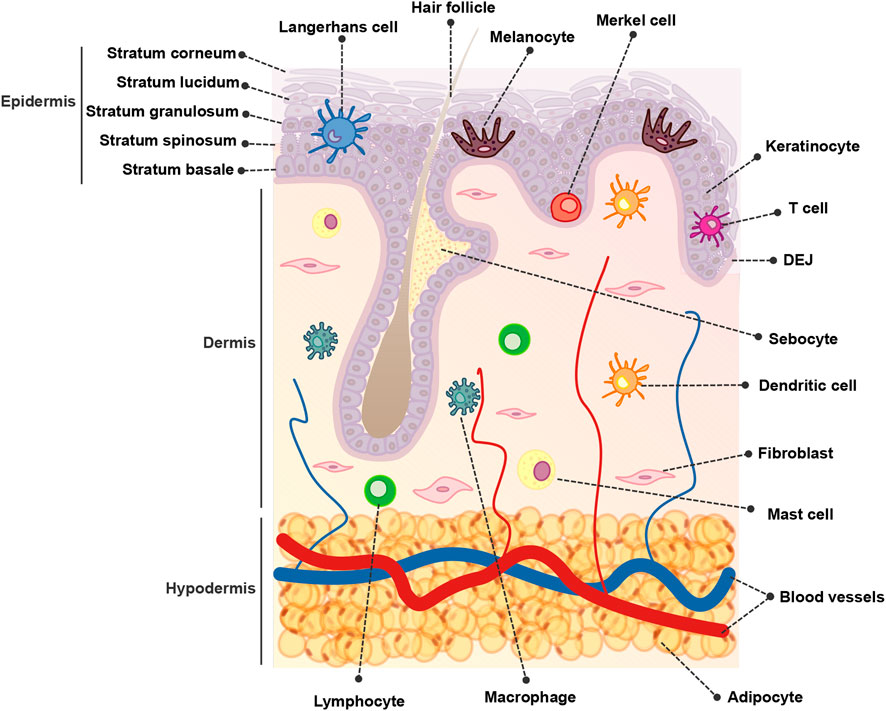
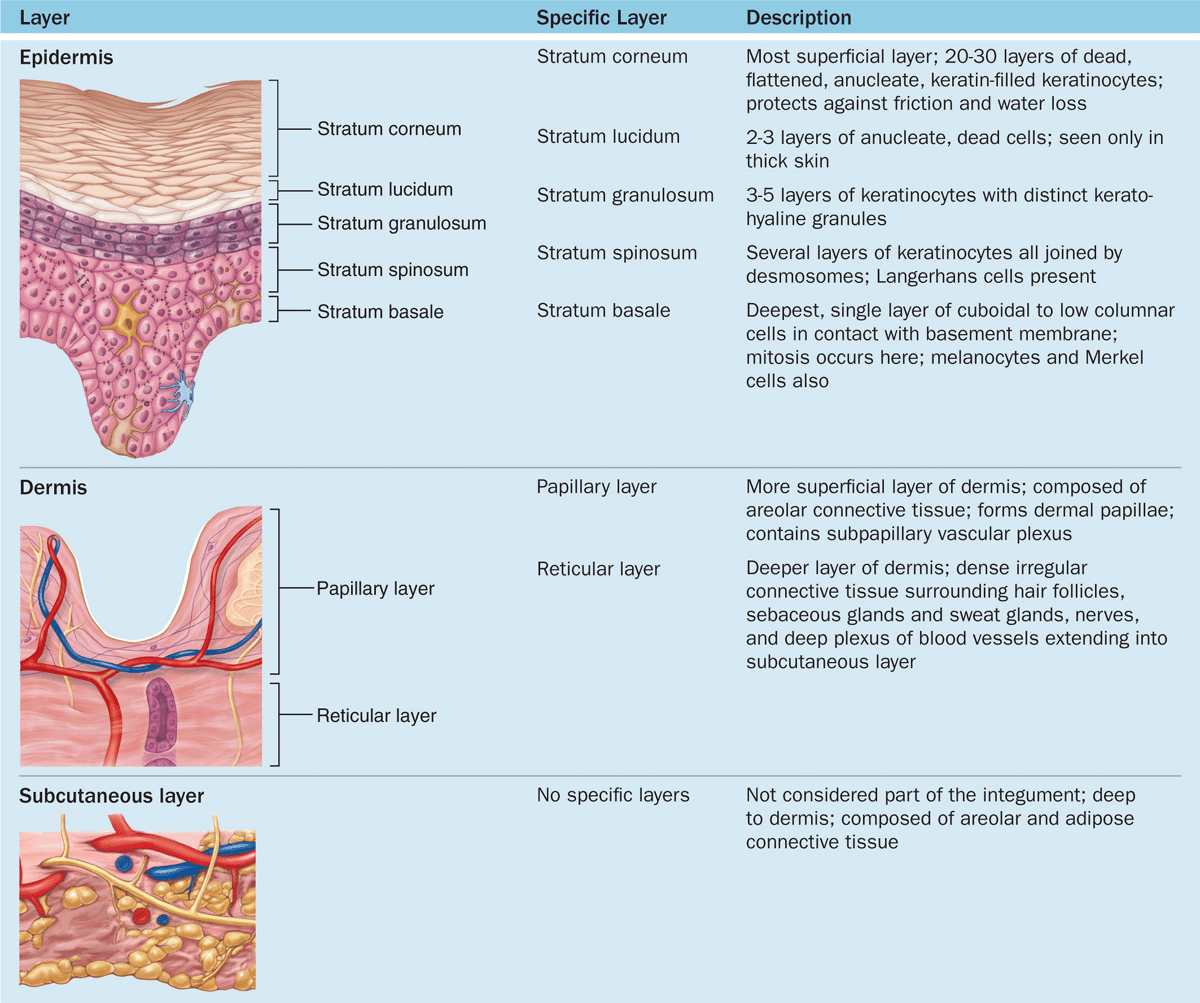
The skin is an integral part of the immune system, containing various immune cells such as Langerhans cells, keratinocytes, and T cells. These cells interact to detect and respond to pathogens, allergens, and other threats. The immune response involves complex metabolic changes within skin cells.
Keratinocytes, for instance, can produce cytokines and chemokines, signaling molecules that recruit other immune cells to the site of infection or inflammation. This production requires energy and involves the activation of various metabolic pathways. Immune cells within the skin also undergo metabolic reprogramming to meet the energy demands of their activation and proliferation.
Metabolic Reprogramming in Immune Cells
When immune cells are activated, they often switch from oxidative phosphorylation to glycolysis, a less efficient but faster way to produce energy. This metabolic shift allows them to rapidly proliferate and produce effector molecules. The skin's immune response is therefore intertwined with complex metabolic changes within its constituent cells.
This interplay between immunity and metabolism in the skin is crucial for maintaining barrier function and preventing infection. Understanding these metabolic pathways is essential for developing targeted therapies for inflammatory skin conditions like eczema and psoriasis.
Conclusion: Skin as a Metabolic Contributor
The skin is more than just a passive barrier; it actively participates in various metabolic processes, most notably vitamin D synthesis. While thermoregulation, detoxification, and immune response involve metabolic components, their primary functions extend beyond pure metabolism.
Recognizing the skin's metabolic capabilities is crucial for promoting skin health and overall well-being. Further research into the metabolic pathways within the skin will undoubtedly lead to new insights and innovative treatments for a wide range of dermatological conditions. Understanding the metabolic function of the skin remains an active area of investigation in both dermatology and broader medical research, with many more discoveries yet to come, impacting how we understand and care for our largest organ.