Which Of The Following Is True Concerning The Primary Assessment

Confusion and misinformation surrounding the correct application of primary assessment protocols are jeopardizing patient safety in emergency medical situations. A critical review of current training materials reveals significant discrepancies, demanding immediate clarification and standardized instruction.
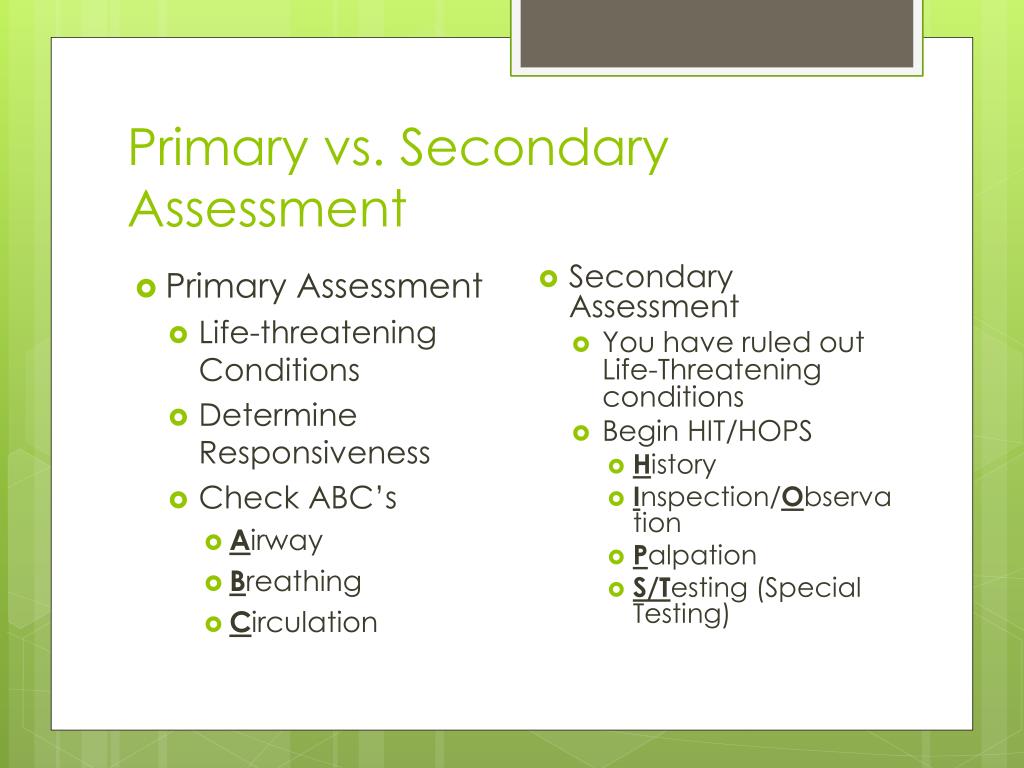
The integrity of the primary assessment – the initial evaluation to identify and treat immediate life threats – is under scrutiny following a surge in reported errors. This article dissects the core components of the primary assessment and clarifies the definitively correct sequence and actions, addressing widespread misconceptions and advocating for unified training standards.
The Core Elements Under Scrutiny
Several key areas within the primary assessment protocol are proving particularly problematic. These include the accurate interpretation of airway patency, the proper assessment of breathing effectiveness, and the timely identification of circulatory compromise.
Furthermore, the integration of the 'C-A-B' (Circulation, Airway, Breathing) versus the older 'A-B-C' (Airway, Breathing, Circulation) sequence, while intended to prioritize immediate hemorrhage control, is generating debate and inconsistent application in the field.
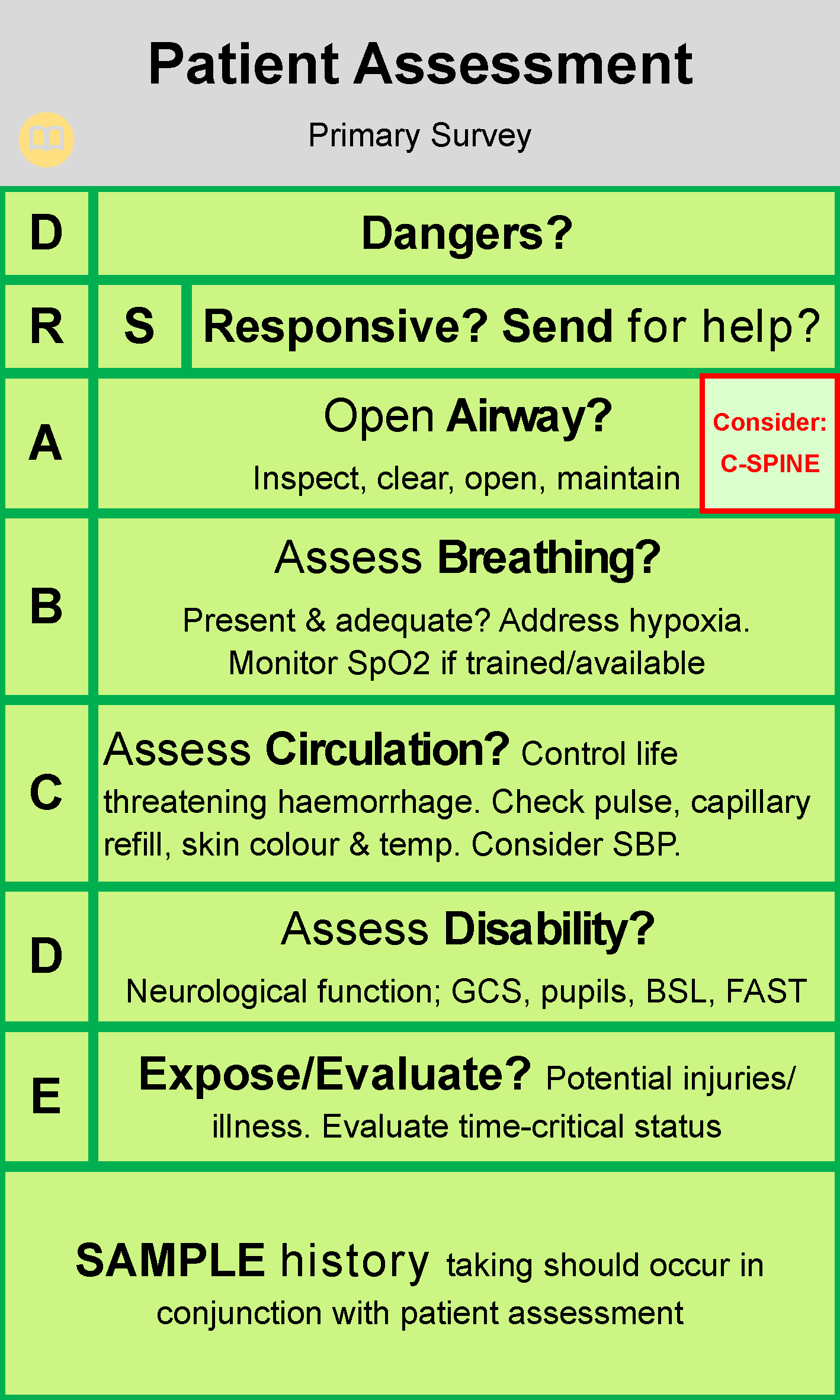
Airway: Clearing the Path to Life
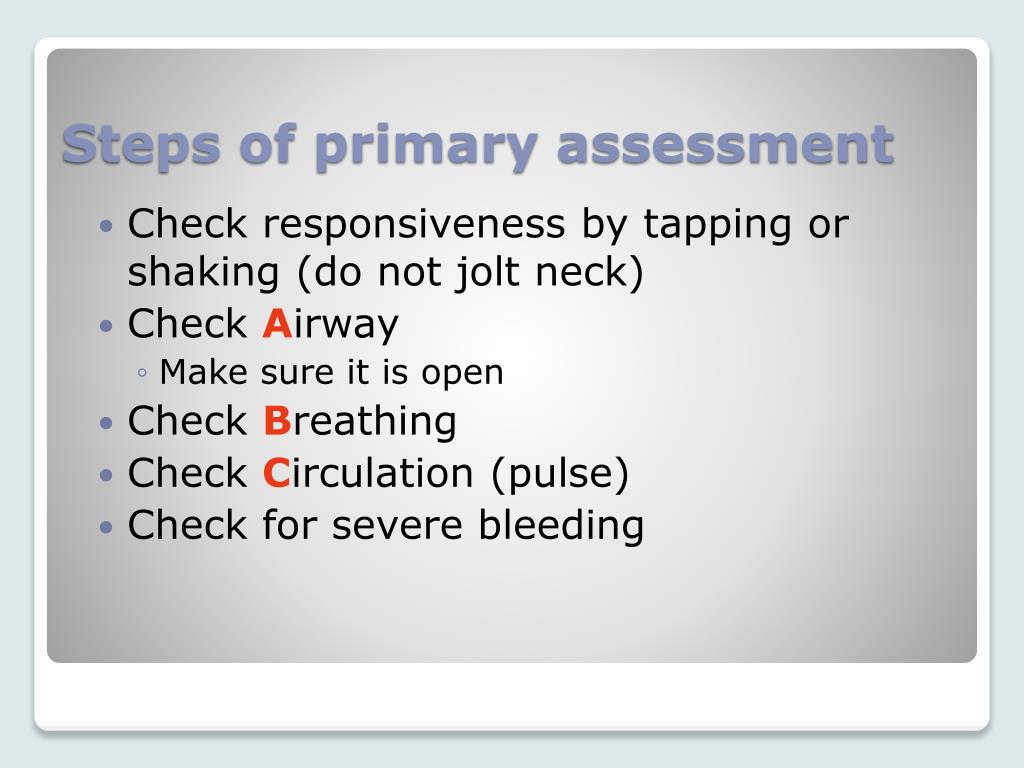
The primary assessment of the airway focuses on ensuring it is open and clear. Obstruction can be caused by the tongue, foreign bodies, or fluids like blood or vomit. The use of techniques such as the head-tilt/chin-lift maneuver or the jaw-thrust maneuver (especially in suspected spinal injury) are crucial.
Suctioning to remove fluids and the insertion of adjuncts like an oropharyngeal airway (OPA) or nasopharyngeal airway (NPA) may be necessary to maintain a patent airway.
Breathing: Assessing the Effectiveness of Respiration
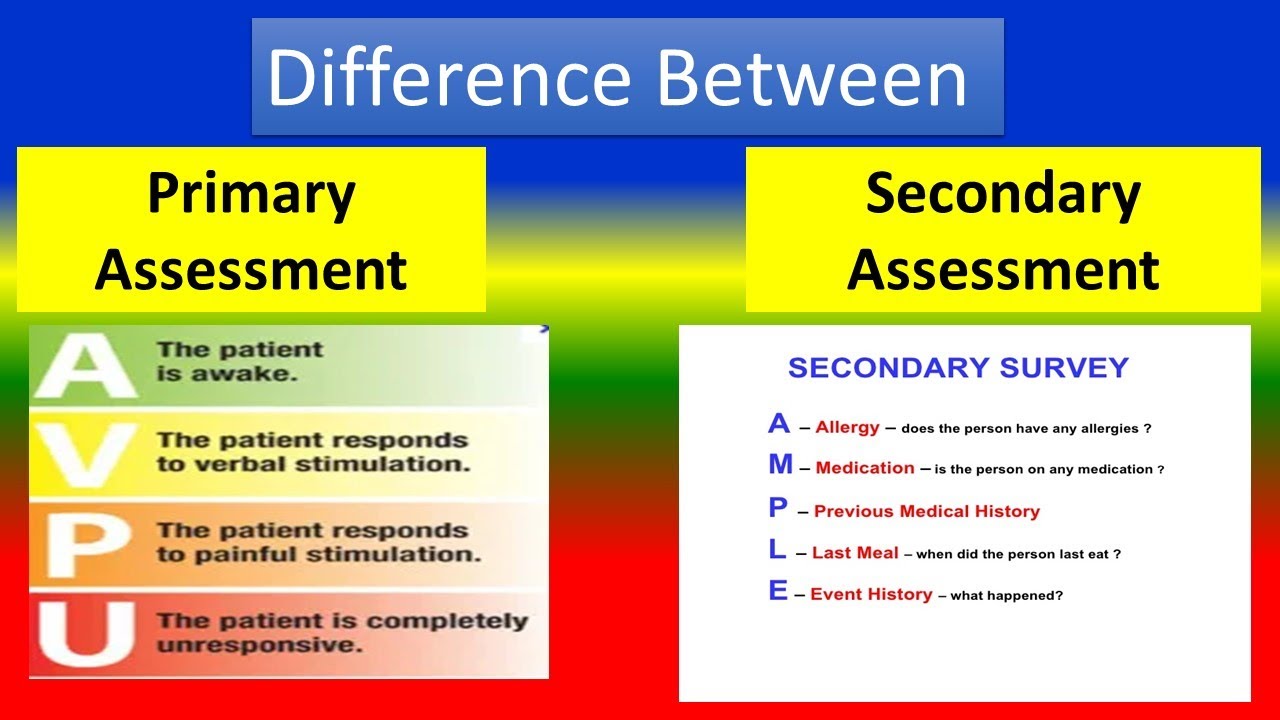
Once the airway is open, the primary assessment shifts to evaluating the patient's breathing. This involves observing the rate, rhythm, and depth of respirations. Assessing for signs of respiratory distress, such as the use of accessory muscles, nasal flaring, or cyanosis, is paramount.
Consideration should be given to the administration of supplemental oxygen via non-rebreather mask or bag-valve-mask (BVM) ventilation if the patient's breathing is inadequate.
Circulation: Evaluating and Addressing Perfusion
The circulatory assessment focuses on evaluating the patient’s pulse, skin color, temperature, and condition. Assessing for signs of bleeding, both external and internal, is essential.
Controlling major hemorrhage with direct pressure, tourniquets, or hemostatic agents takes precedence. Rapid transport is indicated for patients with signs of shock or uncontrolled bleeding.
Debunking Common Misconceptions
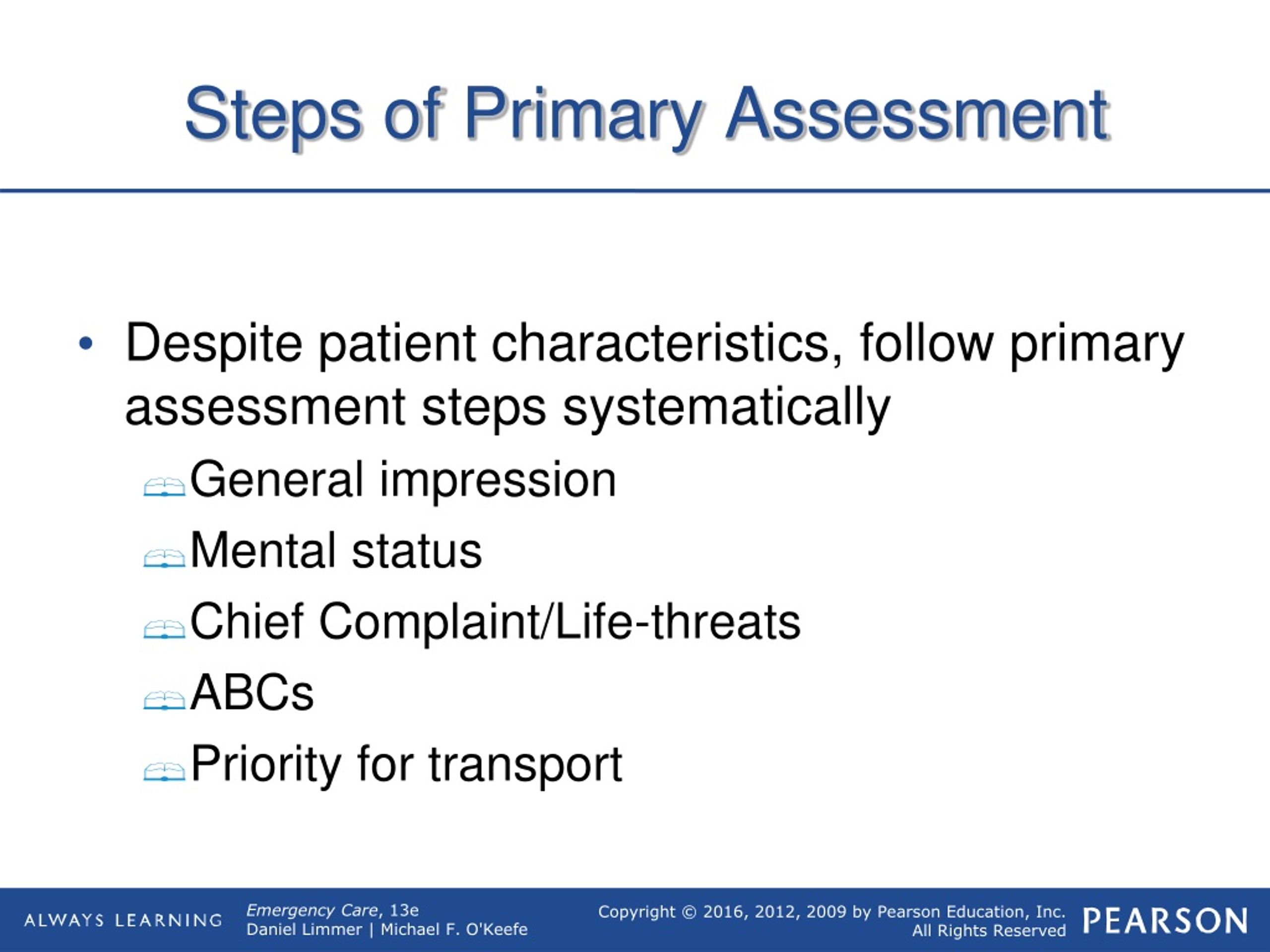
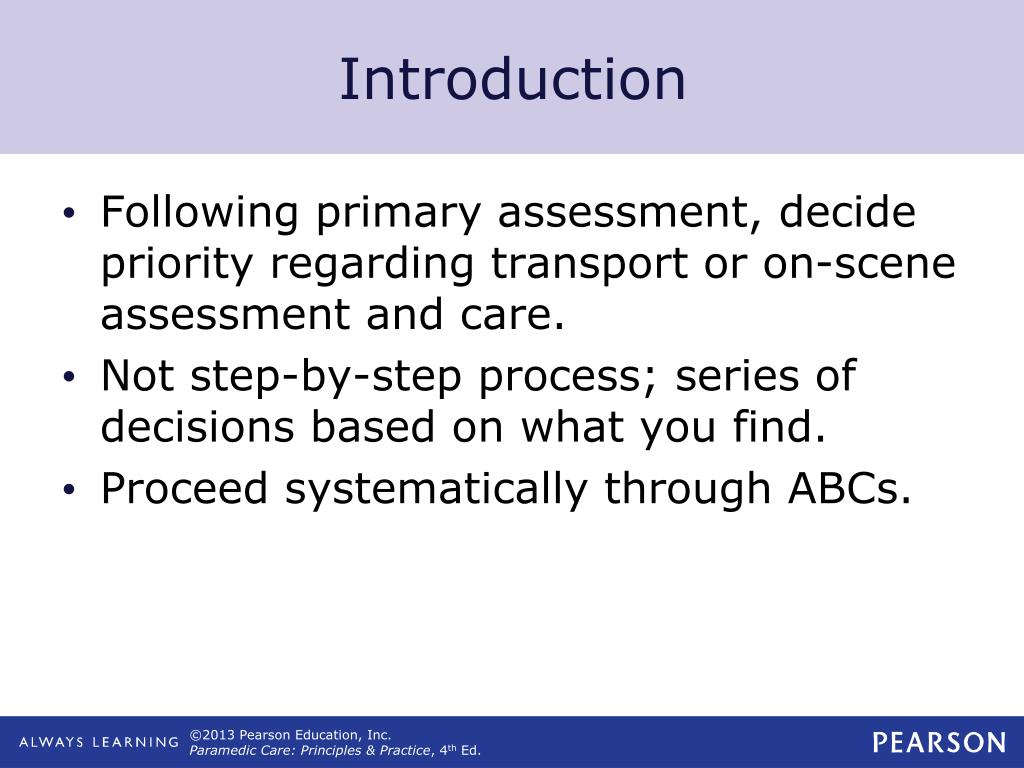
A widespread misconception is that the primary assessment is a rigid, inflexible process. In reality, it's a dynamic evaluation that adapts to the patient's condition. Continuous reassessment and intervention are critical components.
Another common error is neglecting to address life threats in the order they are identified. For example, addressing airway obstruction before assessing breathing can be fatal.
Some practitioners incorrectly believe that the primary assessment is solely a physical examination. It also involves obtaining a brief history of the event (e.g., mechanism of injury, chief complaint) from the patient, bystanders, or first responders, when possible.
Clarifying the 'C-A-B' Sequence
The shift from 'A-B-C' to 'C-A-B' in some protocols reflects a growing understanding of the importance of immediate hemorrhage control. While the updated sequence prioritizes circulation in specific situations like traumatic injuries with significant bleeding, it is not universally applicable.
The American Heart Association (AHA) emphasizes that for most medical emergencies (e.g., cardiac arrest), the traditional 'A-B-C' sequence remains appropriate. This distinction is a source of ongoing confusion and requires clear articulation in training materials.
The Urgency of Standardized Training
Healthcare professionals and Emergency Medical Services (EMS) providers require standardized training in primary assessment protocols. Discrepancies in training lead to inconsistent application in the field, potentially jeopardizing patient outcomes.
"The lack of unified standards is unacceptable," stated Dr. Emily Carter, a leading expert in emergency medicine. "We need clear, concise, and evidence-based guidelines that are consistently taught and implemented."
This issue affects everyone, from paramedics responding to accidents to nurses and doctors in emergency rooms. It is vital that all healthcare providers, regardless of their specific role, possess a solid understanding of this assessment.
Next Steps: Towards a Unified Approach
Several organizations are actively working to address the inconsistencies in primary assessment training. The National Association of Emergency Medical Technicians (NAEMT) is revising its educational materials to reflect the latest evidence and best practices.
Furthermore, the American College of Surgeons (ACS) is advocating for the integration of standardized primary assessment protocols into medical school curricula and continuing education programs.
The immediate priority is to disseminate clear and concise guidelines to all healthcare providers. This includes online resources, training videos, and simulation-based learning opportunities.
Ongoing monitoring of patient outcomes and feedback from field practitioners will be crucial to refining and improving the primary assessment process. The lives of countless individuals depend on our ability to get this right.

.jpg)

.jpg)