Which Of The Following May Result From Systemic Anaphylaxis

The sudden, terrifying onset of systemic anaphylaxis can transform a seemingly ordinary moment into a life-threatening emergency. A single bite of the wrong food, a bee sting, or even a medication can trigger a cascade of physiological events that, if not promptly addressed, can lead to catastrophic consequences. Understanding the potential outcomes of this severe allergic reaction is crucial for both individuals at risk and the medical professionals who treat them.
This article delves into the potentially devastating results of systemic anaphylaxis, exploring the range of symptoms, the underlying mechanisms, and the critical interventions necessary to prevent the most severe outcomes. We will examine the physiological pathways that lead from initial allergen exposure to the most dangerous consequences, drawing on data from reputable organizations like the National Institute of Allergy and Infectious Diseases (NIAID) and the World Allergy Organization (WAO) to provide a clear and comprehensive picture of this serious medical condition.
Understanding Systemic Anaphylaxis
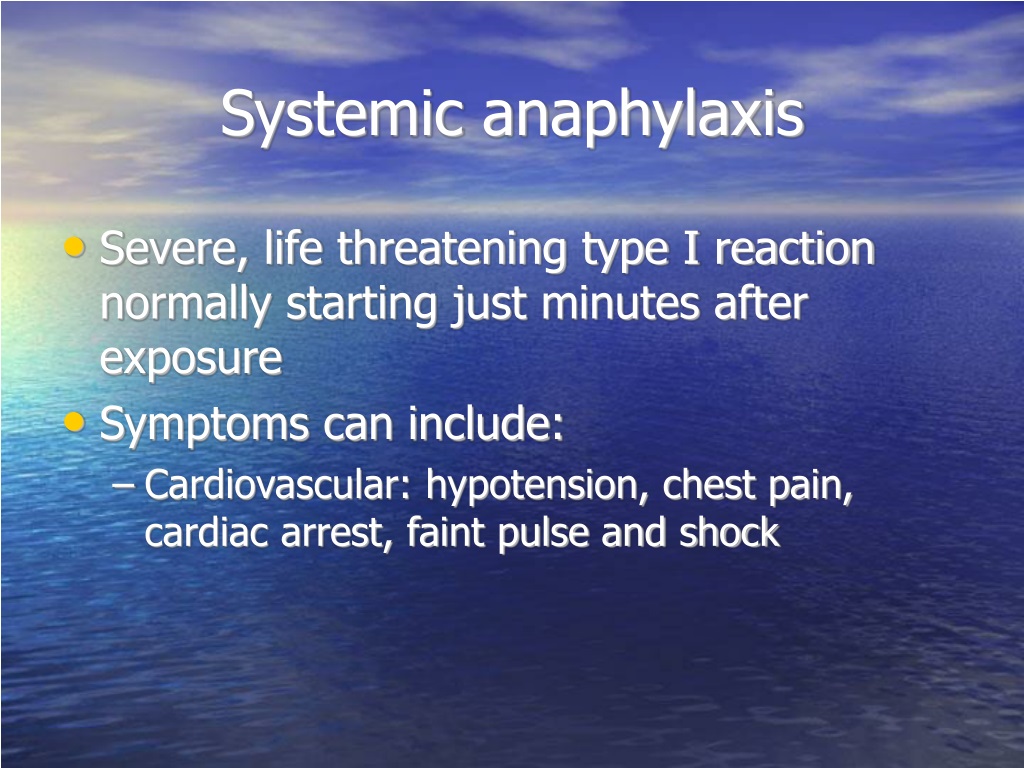
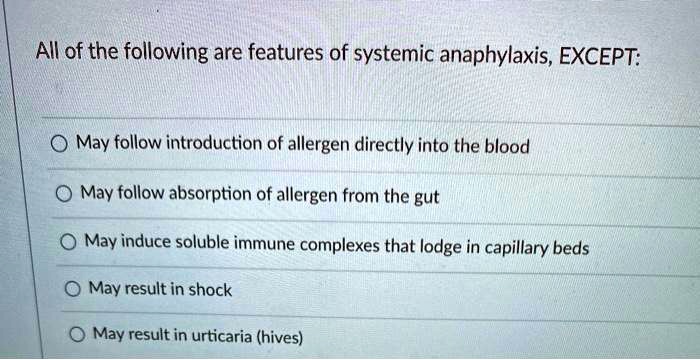
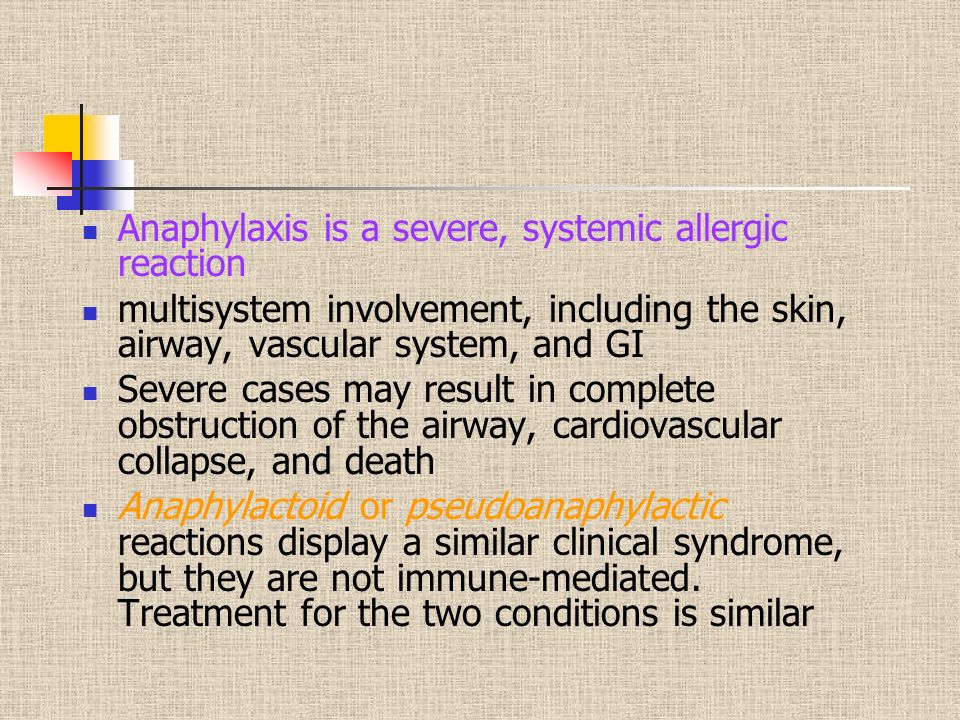
Systemic anaphylaxis is a severe, potentially fatal allergic reaction that affects multiple organ systems simultaneously. It's characterized by a rapid onset and widespread inflammation, leading to a variety of symptoms.
It occurs when the immune system overreacts to an allergen, releasing a flood of chemicals, including histamine, that cause widespread vasodilation and increased vascular permeability.
Common Triggers
The most common triggers of systemic anaphylaxis vary depending on age and geographic location. However, certain allergens consistently rank high on the list.
These include foods like peanuts, tree nuts, shellfish, milk, and eggs. Insect stings from bees, wasps, and hornets are also frequent culprits, as are certain medications like penicillin and other antibiotics.
Potential Outcomes of Systemic Anaphylaxis
The consequences of systemic anaphylaxis can range from mild discomfort to life-threatening emergencies. The severity of the reaction depends on factors such as the individual's sensitivity, the amount of allergen exposure, and the speed of intervention.
Prompt recognition and treatment are crucial to preventing the most dire outcomes.
Respiratory Distress
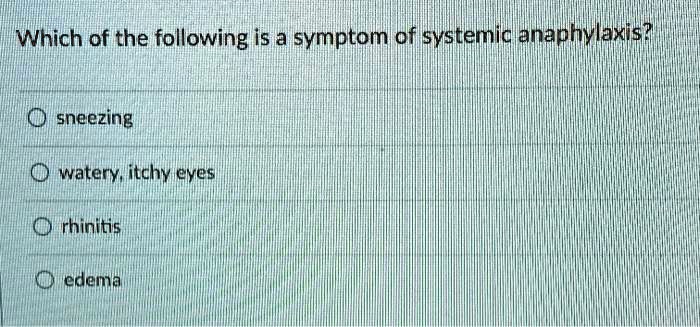
One of the most immediate and dangerous outcomes of systemic anaphylaxis is respiratory distress. The release of inflammatory mediators causes swelling in the upper airways, including the larynx and trachea.
This swelling can lead to stridor (a high-pitched wheezing sound), difficulty breathing, and even complete airway obstruction. Bronchospasm, the constriction of the muscles surrounding the airways, further exacerbates the difficulty in breathing, leading to wheezing and shortness of breath.
Cardiovascular Collapse
Systemic anaphylaxis can also lead to cardiovascular collapse, a life-threatening condition characterized by a sudden drop in blood pressure. The widespread vasodilation caused by histamine and other mediators reduces blood volume returning to the heart.
This, combined with increased capillary permeability, leads to fluid leaking out of the blood vessels into the surrounding tissues. The resulting hypotension can lead to inadequate blood flow to vital organs, including the brain and heart, potentially causing shock and cardiac arrest.
Skin and Mucosal Reactions
Skin and mucosal reactions are common manifestations of systemic anaphylaxis. Hives (urticaria), itching (pruritus), and angioedema (swelling of the deeper layers of the skin, often around the face and lips) are frequently observed.
While these reactions are often distressing, they are not usually life-threatening on their own. However, they can serve as important warning signs of a more severe reaction to come.
Gastrointestinal Symptoms
Gastrointestinal symptoms are another potential outcome of systemic anaphylaxis. These can include nausea, vomiting, abdominal pain, and diarrhea.
These symptoms are thought to be caused by the direct effects of inflammatory mediators on the gastrointestinal tract, leading to increased motility and fluid secretion. While uncomfortable, they are typically less immediately life-threatening than respiratory or cardiovascular complications.
Loss of Consciousness
Loss of consciousness can occur as a result of several factors during systemic anaphylaxis. Hypotension and reduced blood flow to the brain can lead to fainting or even a more prolonged loss of consciousness.
Additionally, severe respiratory distress can lead to hypoxia (low oxygen levels in the blood), further impairing brain function and contributing to loss of consciousness. Unconsciousness is a serious sign and requires immediate medical intervention.
Anaphylactic Shock
Anaphylactic shock represents the most severe and life-threatening form of systemic anaphylaxis. It is characterized by a rapid and profound drop in blood pressure, severe respiratory distress, and often loss of consciousness.
Without immediate treatment, anaphylactic shock can lead to organ failure and death. Epinephrine, administered via an auto-injector, is the first-line treatment for anaphylactic shock and can reverse many of the physiological effects of the reaction.
The Importance of Prompt Treatment
The key to preventing the most severe outcomes of systemic anaphylaxis lies in prompt recognition and treatment. Individuals with known allergies should carry an epinephrine auto-injector (like an EpiPen) and be trained in its proper use.
Additionally, it is crucial to seek immediate medical attention after using an epinephrine auto-injector, as further treatment may be necessary. Emergency medical personnel can provide supplemental oxygen, administer medications to reverse bronchospasm, and provide other supportive care as needed.
Looking Ahead
Ongoing research is focused on developing new and improved treatments for systemic anaphylaxis. This includes exploring alternative routes of epinephrine administration, developing more targeted therapies to block the release of inflammatory mediators, and investigating strategies to prevent allergic sensitization in the first place.
Furthermore, improved educational initiatives are needed to raise awareness of anaphylaxis among the general public and healthcare professionals. By increasing understanding and improving access to timely treatment, we can significantly reduce the morbidity and mortality associated with this potentially devastating condition.
Ultimately, understanding the potential consequences of systemic anaphylaxis empowers individuals at risk to take proactive steps to protect their health. With increased awareness, prompt treatment, and ongoing research, we can strive to minimize the impact of this serious allergic reaction.











.jpg)