Which Of The Following Represents Drug Tolerance

For many individuals, the repeated use of medications or substances can lead to a perplexing phenomenon known as drug tolerance. Understanding the mechanisms behind this process is crucial for both patients and healthcare professionals alike. This article explores the defining characteristics of drug tolerance, drawing on scientific understanding and practical examples.
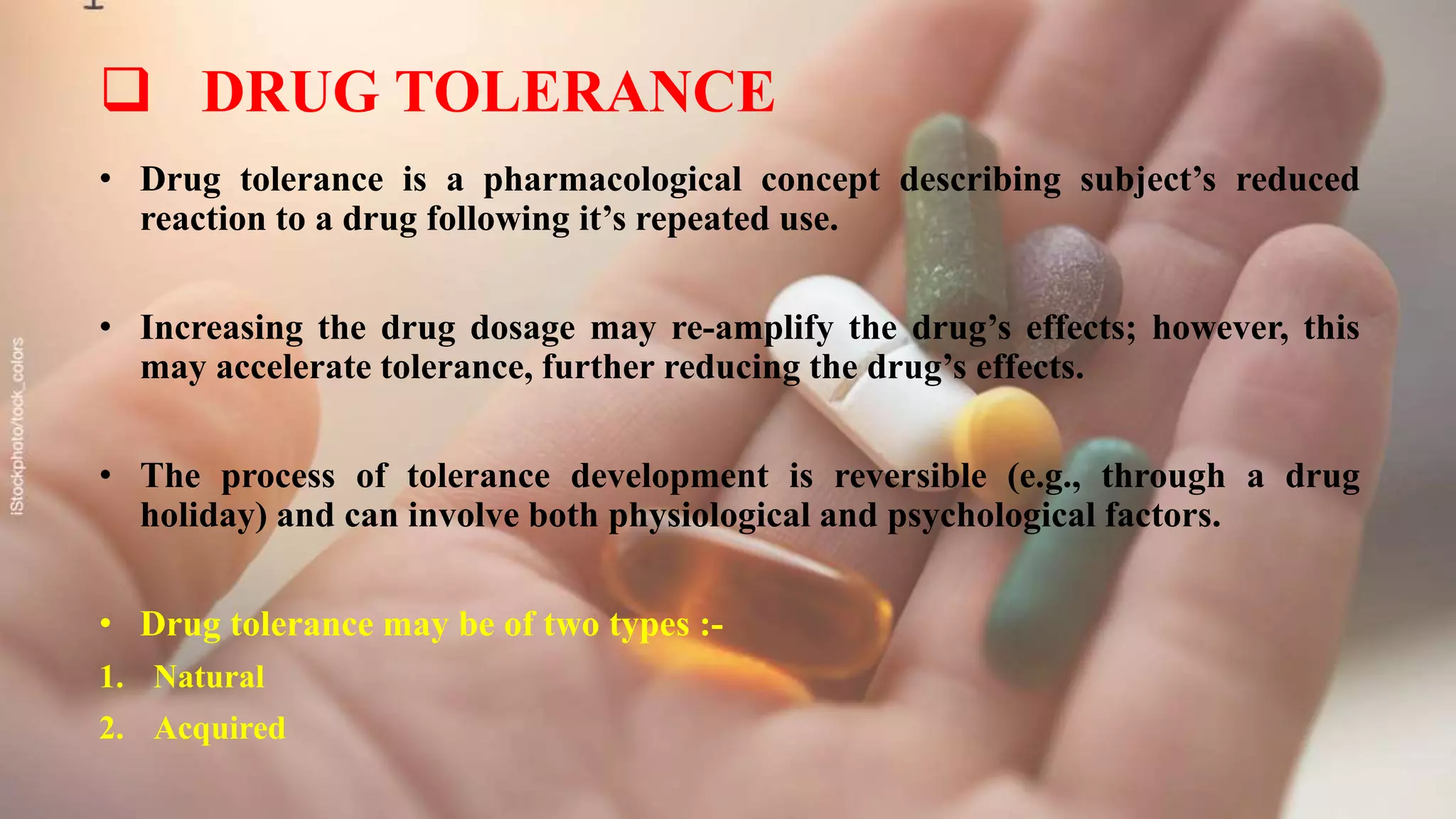
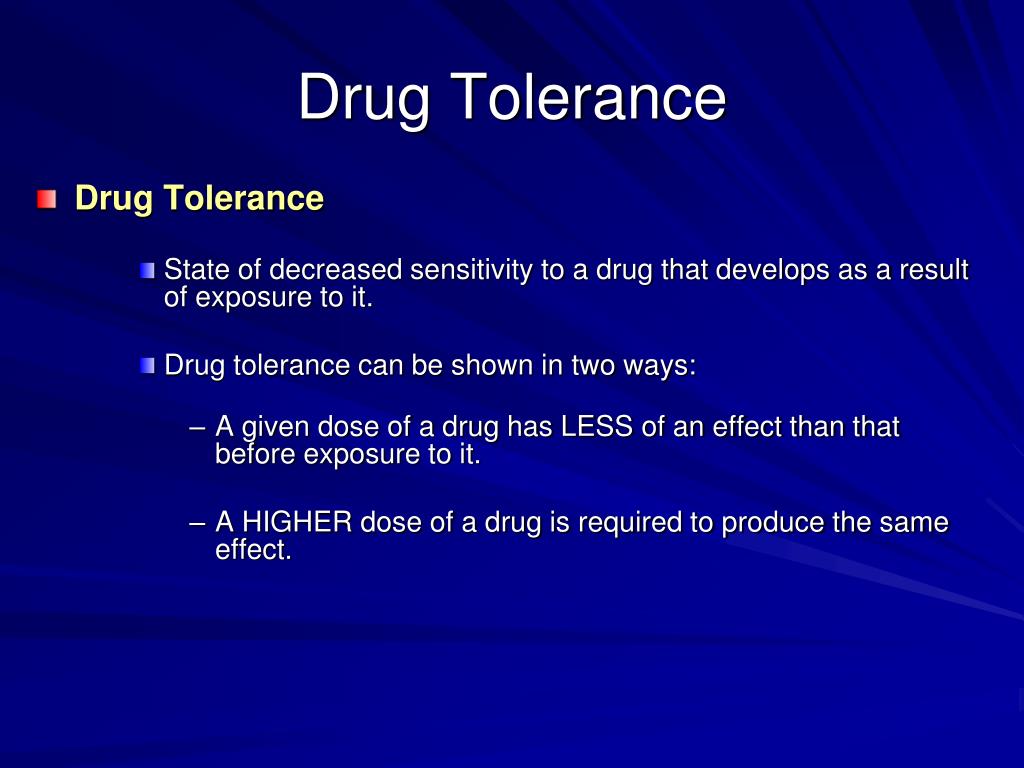
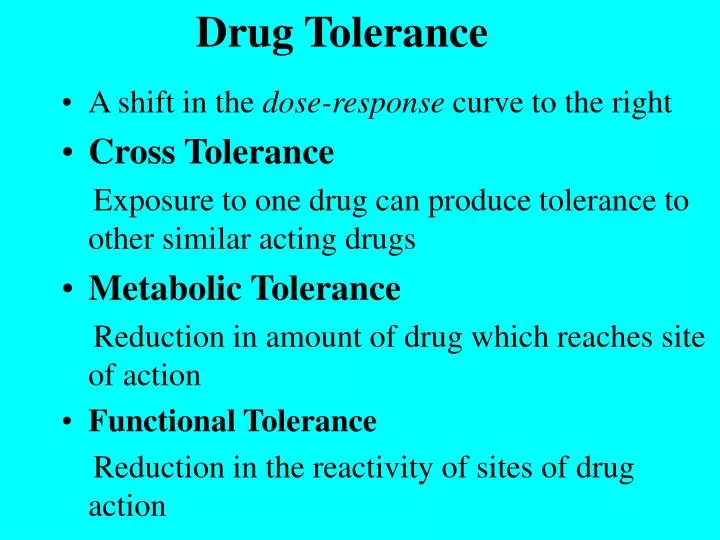
Drug tolerance, in its simplest form, refers to the body's reduced response to a drug following repeated exposure. The National Institute on Drug Abuse (NIDA) defines tolerance as needing more of a substance to get the same effect. This happens when the body adapts to the continuous presence of the drug.
What is Drug Tolerance?
Drug tolerance is a pharmacological concept that describes a decrease in response to a drug after prolonged use. It is important to understand that drug tolerance is not addiction. It is a physiological adaptation by the body.
The underlying mechanisms of drug tolerance are varied and complex. They can involve changes in drug metabolism, receptor sensitivity, and cellular adaptation. Understanding these mechanisms is crucial for effectively managing treatment and minimizing potential risks.
Key Characteristics
Several key characteristics define drug tolerance. The most notable is the need for increasing doses of a substance to achieve the originally experienced effects. This escalation can lead to various complications, including potential overdose.
Tolerance can develop at different rates depending on the drug and individual factors. Some individuals may develop tolerance relatively quickly, while others may experience a more gradual process. Genetic predisposition, body weight, and overall health can all influence the rate of tolerance development.
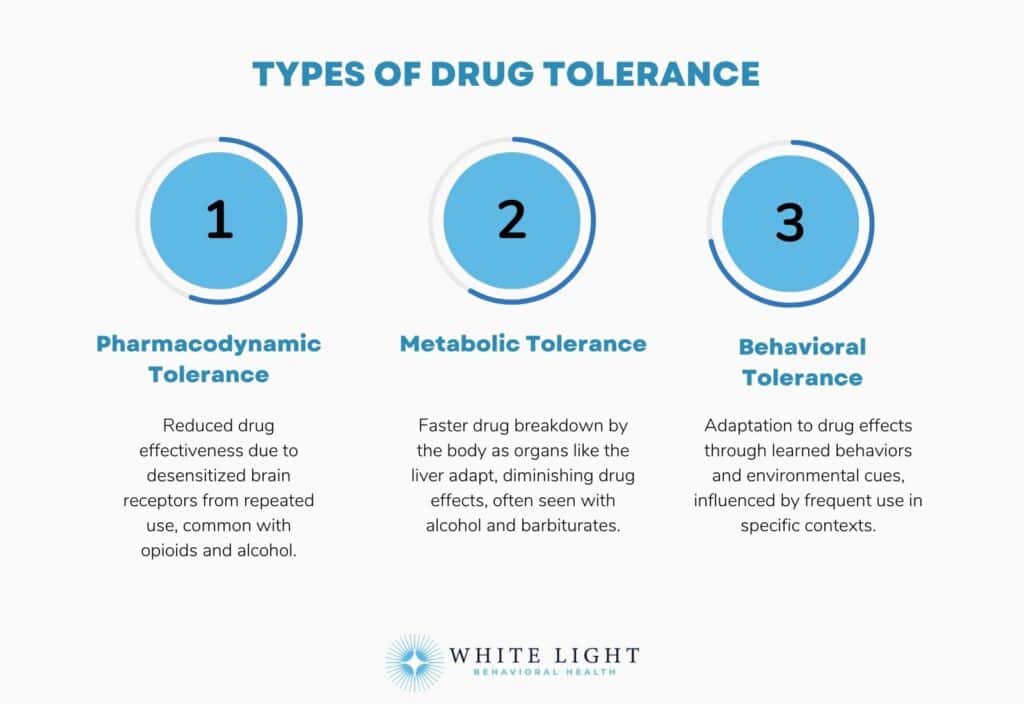
There are three main types of drug tolerance. These include metabolic tolerance, pharmacodynamic tolerance, and behavioral tolerance. Each type represents a different mechanism through which the body adapts to the presence of a drug.
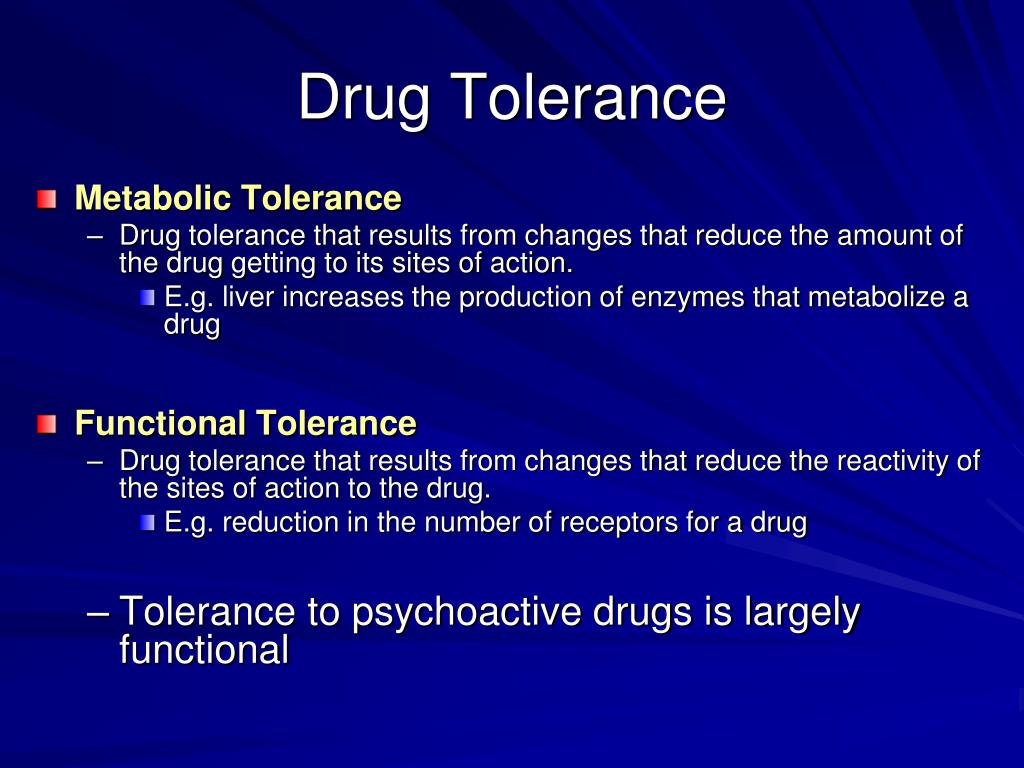
Metabolic tolerance occurs when the body becomes more efficient at metabolizing and eliminating the drug. Pharmacodynamic tolerance involves changes in the drug's receptors in the body, decreasing their sensitivity. Behavioral tolerance involves the user compensating for the effects of the drug through learned behaviors.
Metabolic Tolerance
Metabolic tolerance, also known as pharmacokinetic tolerance, is often related to enzyme induction. The body produces more of the enzymes responsible for breaking down the drug. This leads to a faster clearance rate and reduced drug concentration in the bloodstream.
For instance, chronic alcohol consumption can induce the production of liver enzymes involved in alcohol metabolism. This means that over time, a person who drinks regularly may need to consume more alcohol to experience the same level of intoxication. The liver is working more efficiently to break down the alcohol.
Pharmacodynamic Tolerance
Pharmacodynamic tolerance, also known as cellular tolerance, involves changes at the site of drug action. The number or sensitivity of receptors for the drug may decrease. This reduces the drug's ability to exert its effects.
Opioids are a classic example. With repeated exposure, opioid receptors can become desensitized or down-regulated. This is where there are fewer receptors available. The result is a diminished analgesic effect requiring higher doses to achieve pain relief.
Behavioral Tolerance
Behavioral tolerance involves learned adaptations to the effects of a drug. The user learns to compensate for the drug's impairment through practice and experience. This type of tolerance can be influenced by environmental cues and behavioral strategies.
For example, someone who frequently drinks alcohol might learn to compensate for impaired coordination by adjusting their movements. While behavioral tolerance may mask some of the drug's effects, it does not eliminate the underlying physiological impairment.
Implications and Risks
Drug tolerance is a significant issue with serious implications. The need for escalating doses can increase the risk of adverse effects and overdose. It also complicates treatment strategies for various medical conditions.
Healthcare providers must carefully monitor patients on long-term medications that can lead to tolerance. This includes opioids, benzodiazepines, and certain psychiatric drugs. Dose adjustments and alternative treatment strategies may be necessary to manage tolerance effectively.
Furthermore, tolerance can mask the signs of addiction, making it more difficult to identify individuals who are developing substance use disorders. It is crucial to distinguish between tolerance and addiction. While tolerance is a physiological adaptation, addiction involves compulsive drug-seeking behavior.
Conclusion
Drug tolerance is a complex physiological adaptation characterized by a diminished response to a drug following repeated exposure. Understanding the different types of tolerance and their underlying mechanisms is essential for managing medication use and minimizing the risks associated with escalating doses. Recognizing the need for increasing doses to achieve the same effect is a key indicator. It highlights the importance of consulting with healthcare professionals to adjust treatment plans accordingly.
By staying informed and vigilant, both patients and healthcare providers can effectively navigate the challenges of drug tolerance. This ensures the safe and responsible use of medications. Further research into the mechanisms of tolerance is crucial. It will lead to the development of more effective strategies for managing this phenomenon and improving patient outcomes.