An Indication Of Aging Of The Urinary System Is

The subtle shift from predictable routines to urgent dashes. The anxiety of long journeys, the constant awareness of bathroom locations. These are the realities creeping into the lives of millions as the aging urinary system begins to make its presence known. It's a silent, often embarrassing, decline that demands greater attention.
This article delves into the complex world of the aging urinary system, focusing on one key indicator: increased urinary frequency. This seemingly innocuous symptom, often dismissed as a minor inconvenience, can signify underlying physiological changes and potential health risks. We will explore the causes, consequences, and management strategies associated with age-related urinary frequency, drawing on expert opinions and scientific data to provide a comprehensive understanding of this widespread concern.
Understanding Increased Urinary Frequency
Increased urinary frequency, defined as the need to urinate more often than usual during the day or night, is a common complaint among older adults. While occasional variations are normal, persistent and bothersome frequency warrants investigation. This can significantly impact quality of life, disrupting sleep, limiting social activities, and contributing to feelings of anxiety and social isolation.
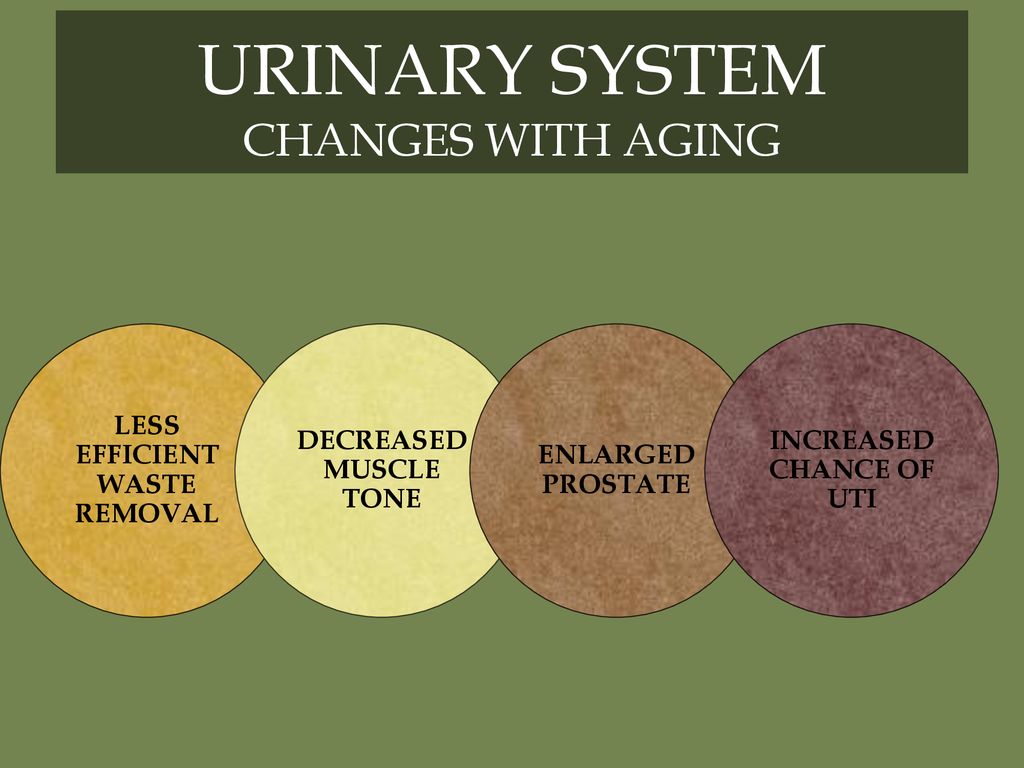
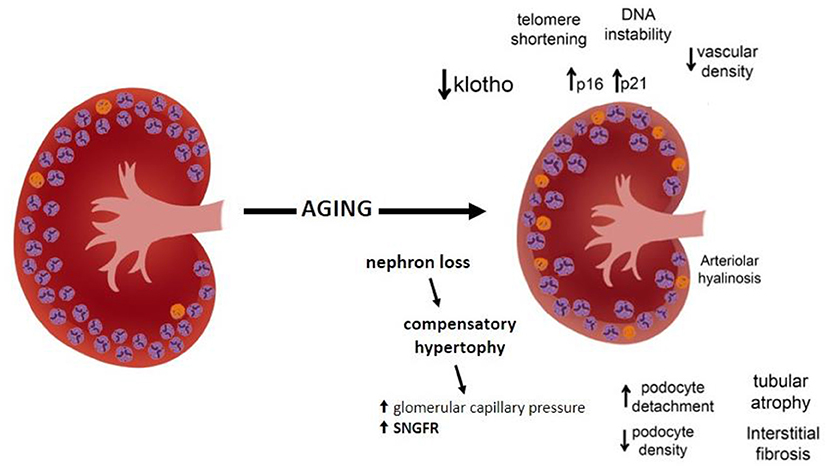
Physiological Changes
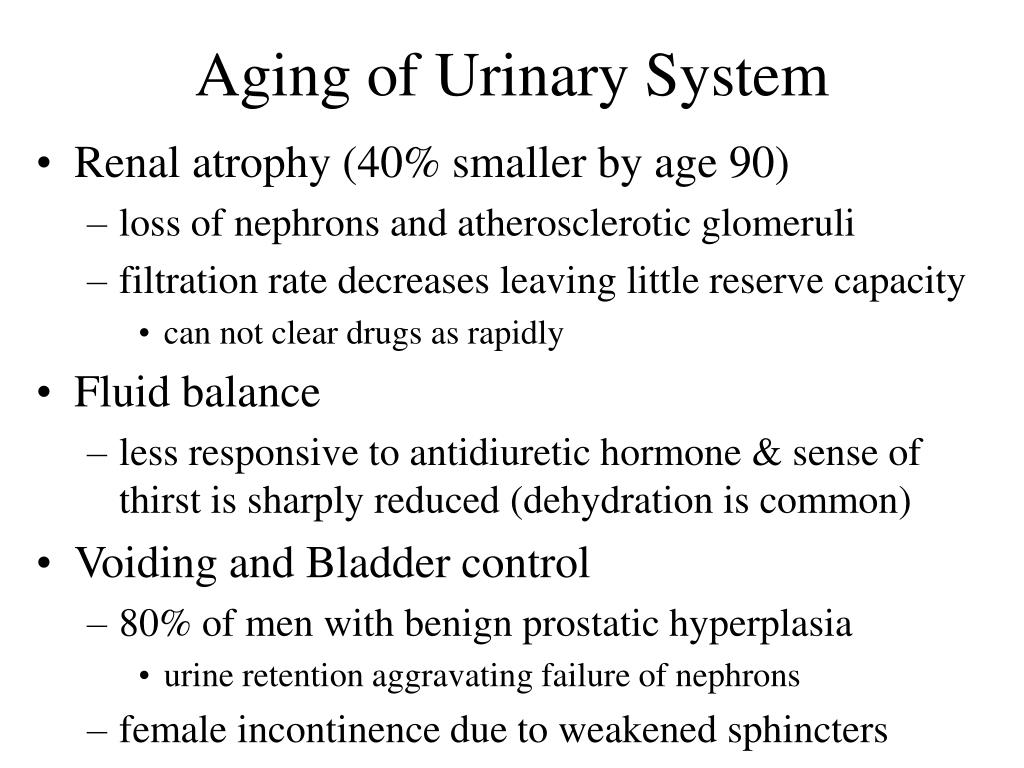
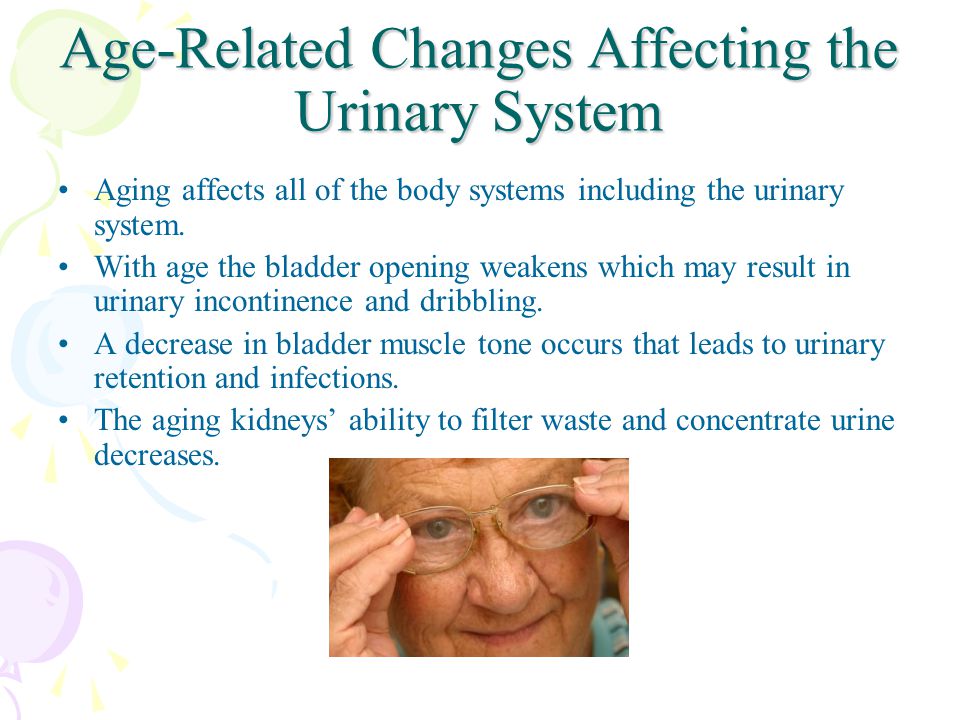
Several age-related physiological changes contribute to increased urinary frequency. The bladder's capacity to hold urine naturally decreases with age, leading to more frequent urges. The detrusor muscle, responsible for bladder contraction, may become overactive, causing involuntary contractions and a sense of urgency.
Hormonal changes, particularly in women following menopause, also play a role. Decreased estrogen levels can weaken the pelvic floor muscles and the urethral lining, increasing the risk of urinary incontinence and frequency. In men, an enlarged prostate (benign prostatic hyperplasia or BPH) is a frequent culprit, obstructing urine flow and leading to bladder irritation and frequent urination, especially at night (nocturia).
Underlying Medical Conditions
While aging is a primary factor, increased urinary frequency can also be a symptom of various underlying medical conditions. Diabetes, both type 1 and type 2, can cause increased thirst and urine production. Urinary tract infections (UTIs) irritate the bladder lining, leading to frequent and urgent urination.
Overactive bladder (OAB) syndrome, characterized by urinary urgency, frequency, and sometimes urge incontinence, is another common condition. Neurological disorders such as stroke, Parkinson's disease, and multiple sclerosis can also affect bladder control and contribute to increased frequency.
Impact and Management
The impact of increased urinary frequency extends beyond mere inconvenience. The constant need to find a restroom can lead to anxiety and limit participation in social activities. Sleep disruption due to nocturia can contribute to fatigue, decreased cognitive function, and an increased risk of falls, especially in older adults.
Behavioral Modifications
Simple behavioral modifications can often provide significant relief. Bladder training, involving gradually increasing the time between urination, can help improve bladder capacity. Reducing fluid intake before bedtime and avoiding caffeine and alcohol, known bladder irritants, can also be beneficial.
Pelvic floor exercises, also known as Kegel exercises, can strengthen the muscles that support the bladder and urethra, improving bladder control. Maintaining a healthy weight can also reduce pressure on the bladder.
Medical Interventions
When behavioral modifications are insufficient, medical interventions may be necessary. Medications, such as antimuscarinics and beta-3 agonists, can help relax the bladder muscle and reduce urgency and frequency. In men with BPH, medications such as alpha-blockers and 5-alpha reductase inhibitors can help relax the prostate and improve urine flow.
In some cases, surgery may be considered. Surgical options for BPH include transurethral resection of the prostate (TURP) and laser prostatectomy. For women with stress urinary incontinence, surgical procedures can strengthen the pelvic floor and support the urethra.
Seeking Professional Help
It is crucial to consult a healthcare professional if increased urinary frequency is persistent, bothersome, or accompanied by other symptoms such as pain, blood in the urine, or fever. A thorough medical evaluation can help identify the underlying cause and guide appropriate treatment. Ignoring the problem can lead to further complications and a reduced quality of life.
Future Directions
Research into the aging urinary system is ongoing, with a focus on developing more effective and less invasive treatments. New medications targeting specific bladder pathways are being investigated. Minimally invasive surgical techniques are also being refined to reduce recovery time and improve outcomes.
Furthermore, there is a growing emphasis on preventative measures. Promoting healthy lifestyle choices, such as regular exercise and a balanced diet, can help maintain bladder health and reduce the risk of age-related urinary problems. Early detection and management of underlying medical conditions such as diabetes and hypertension are also crucial.
Increased urinary frequency is a significant indicator of aging within the urinary system, demanding recognition and proactive management. By understanding the underlying causes, implementing appropriate lifestyle modifications, and seeking timely medical attention, individuals can mitigate its impact and maintain a higher quality of life as they age. This isn't just about managing symptoms; it's about empowering individuals to take control of their health and well-being throughout their lifespan.