Does Semaglutide Show Up In Routine Blood Work

Urgent concerns are emerging about the detection of semaglutide in routine blood work. Can this increasingly popular weight loss drug be identified without specific testing?
This article addresses whether standard blood panels flag semaglutide use, and what implications this has for individuals and healthcare providers.
The Core Question: Detection or Not?
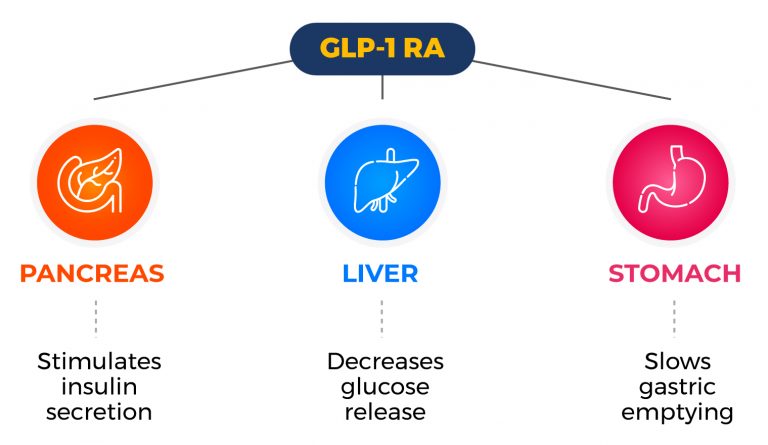
The central question is straightforward: does semaglutide, a GLP-1 receptor agonist marketed as Ozempic and Wegovy, routinely appear in standard blood tests?
The consensus among medical professionals and lab specialists is generally no.
Standard blood panels typically assess basic metabolic functions, liver function, kidney function, and blood cell counts, not specific drug compounds like semaglutide.
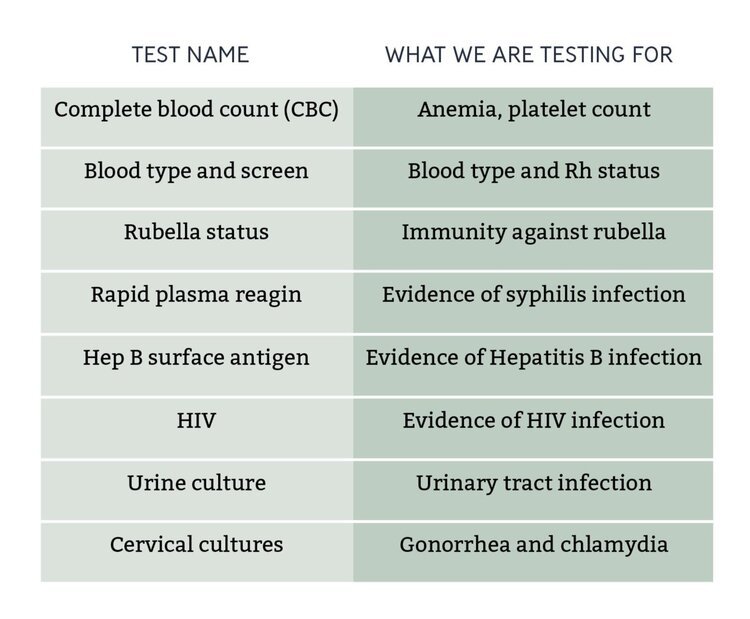
Routine Blood Work Defined
Routine blood work usually encompasses a complete blood count (CBC), a comprehensive metabolic panel (CMP), and lipid panel.
These tests look at markers like glucose, electrolytes, cholesterol, and liver enzymes.
They are designed to evaluate overall health and screen for common conditions such as diabetes, high cholesterol, and liver or kidney problems.
Specific Testing Required
To detect semaglutide directly, a specialized assay is required.
These assays, often utilizing liquid chromatography-mass spectrometry (LC-MS), are not part of routine screening.
They are employed in specific clinical or research settings where knowledge of semaglutide levels is critical.
Circumstantial Evidence and Indirect Effects
While semaglutide doesn't show up directly, its effects can sometimes be inferred from changes in routine blood work.
For example, improved glucose control (lower blood sugar levels) in a diabetic patient could suggest semaglutide use, although it could also be due to other factors like diet or other medications.
Weight loss itself can improve lipid profiles (cholesterol levels), which could also indirectly point to semaglutide but is not conclusive evidence.
Who Needs to Know?
Patients should always inform their healthcare providers about all medications and supplements they are taking, including semaglutide.
This is crucial for accurate diagnosis and treatment decisions, especially if unusual results appear in routine blood work.
Healthcare providers need to be aware to interpret blood test results correctly in the context of semaglutide use.
Why This Matters
The implications of undetected semaglutide use in routine blood work are significant.
Doctors may misinterpret results if they are unaware a patient is taking the drug.
Additionally, the lack of routine detection impacts drug monitoring and adherence, especially in cases where patients are not forthcoming about their medication use.
When Could This Be a Problem?
This becomes particularly relevant in pre-operative settings.
Delayed gastric emptying, a known side effect of semaglutide, can increase the risk of aspiration during anesthesia.
If a patient is unknowingly taking semaglutide and doesn't disclose it, anesthesiologists may not take appropriate precautions.
How to Ensure Proper Disclosure
Open communication between patients and healthcare providers is paramount.
Clinics are encouraged to proactively ask about semaglutide and similar medications during patient intake.
Standardized questionnaires including specific questions about weight loss medications can help prevent unintentional omissions.
Ongoing Research and Future Directions
Research into the long-term effects of semaglutide continues.
As the drug's use becomes more widespread, the need for more sensitive and specific detection methods may increase.
Some labs are developing more comprehensive panels that could potentially include semaglutide markers, but these are not yet standard.
The Bottom Line
Semaglutide does not appear in routine blood work.
Specific testing is required to detect the drug directly.
Therefore, transparent communication between patients and their healthcare providers is vital to ensure accurate medical assessments and patient safety.
Next Steps
Patients should be proactive in informing their doctors about their semaglutide use.
Healthcare providers should incorporate questions about GLP-1 receptor agonists into their standard patient history intake.
Monitor for updated guidelines from medical organizations regarding semaglutide use and pre-operative protocols.