Drug Therapy Requiring Intensive Monitoring For Toxicity
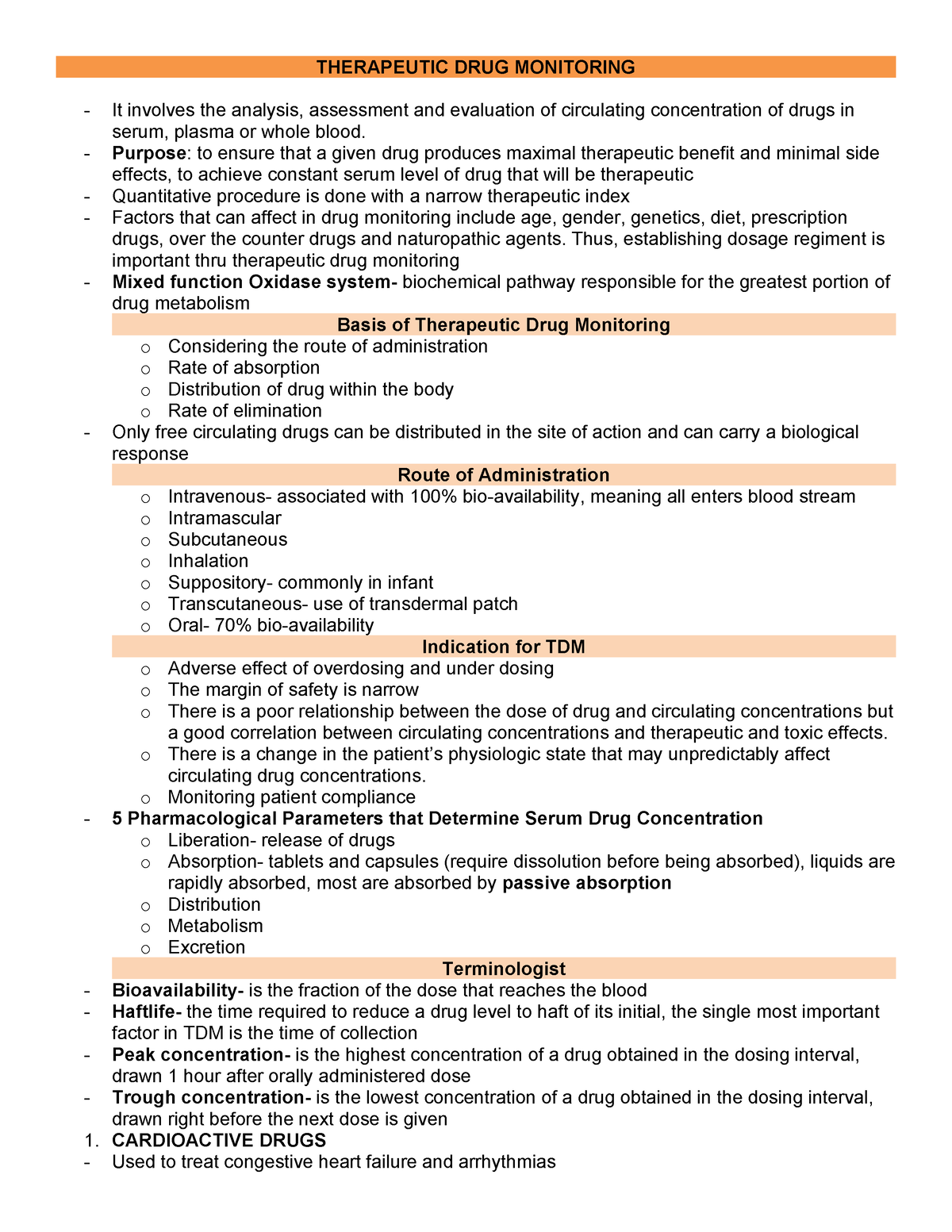
The promise of modern medicine often comes with a caveat: powerful drugs can offer life-altering benefits but may also carry the risk of severe toxicity. This delicate balance necessitates intensive monitoring, creating a complex landscape for patients, physicians, and healthcare systems alike.
For a subset of medications, the line between therapeutic efficacy and dangerous side effects is razor thin, demanding careful observation and proactive intervention.
The Tightrope Walk: Balancing Benefit and Risk
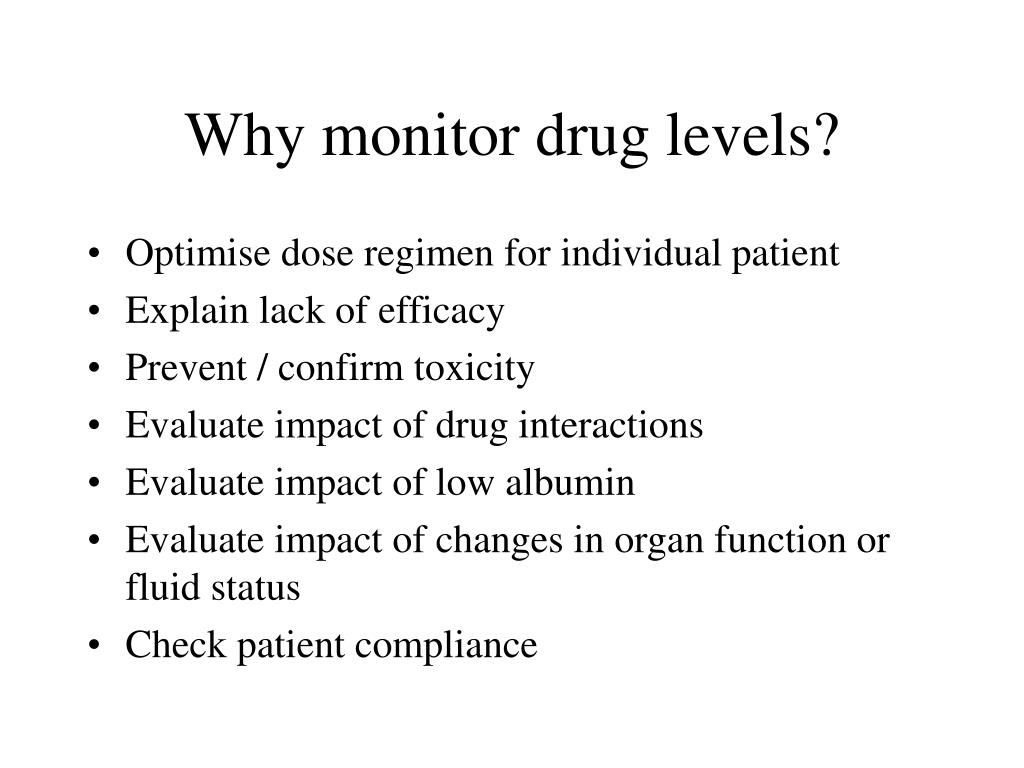
The challenge lies in maximizing the therapeutic effect while minimizing the potential harm. This tightrope walk requires constant vigilance, frequent laboratory tests, and a deep understanding of individual patient factors.
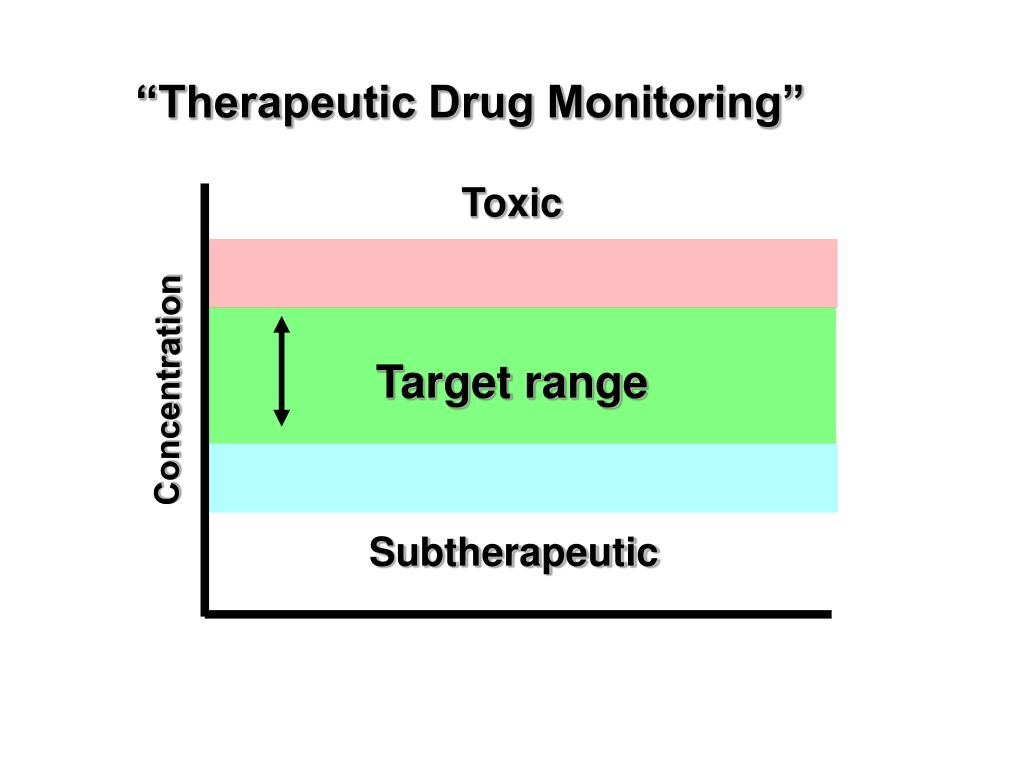
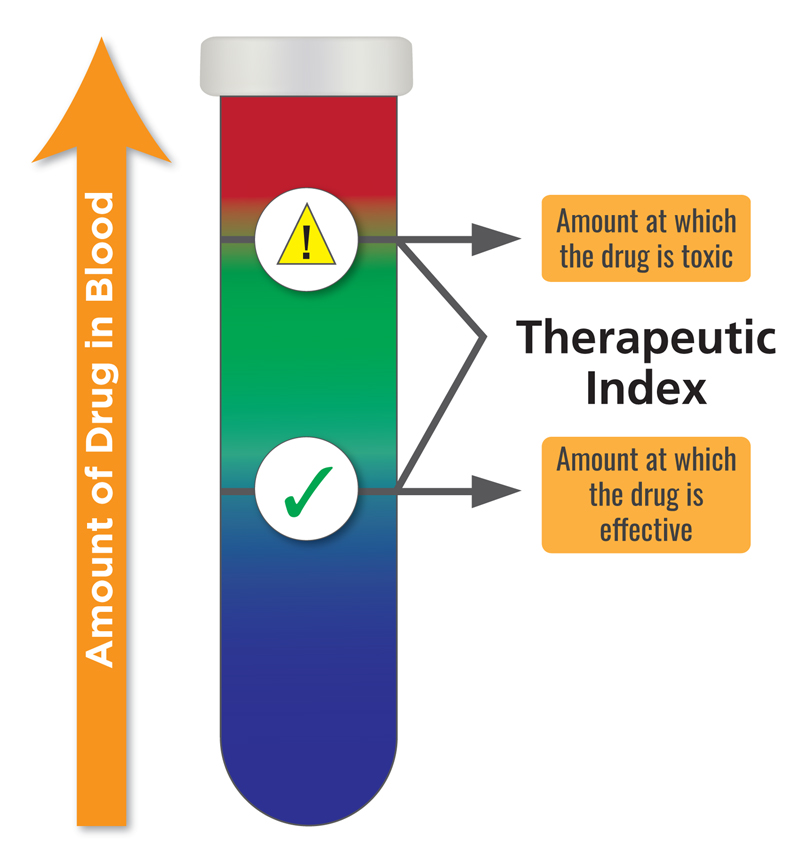
The consequences of inadequate monitoring can be dire, ranging from organ damage and disability to, in extreme cases, death. Many drugs, while highly effective in treating serious conditions, possess a narrow therapeutic index.
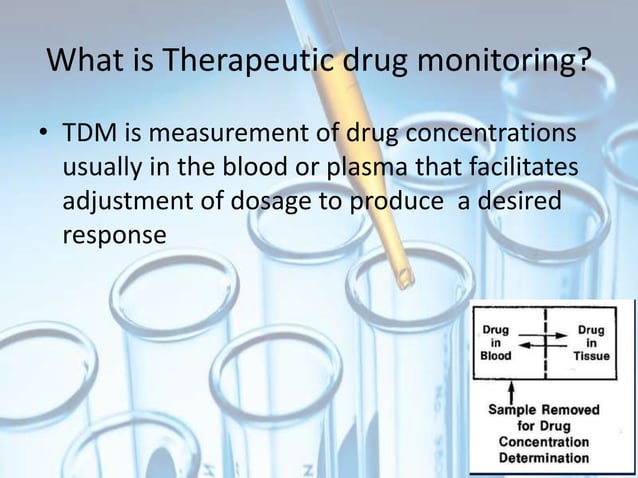
A narrow therapeutic index means that the difference between the effective dose and the toxic dose is small. Drugs with this property, require careful titration and vigilant monitoring to ensure patient safety.
Specific Drugs Requiring Intensive Monitoring
Several classes of medications are notorious for their potential toxicity and require particularly close monitoring. Immunosuppressants, for example, are crucial for preventing organ rejection in transplant recipients, but they can also suppress the immune system to the point of increasing susceptibility to infections and cancer.
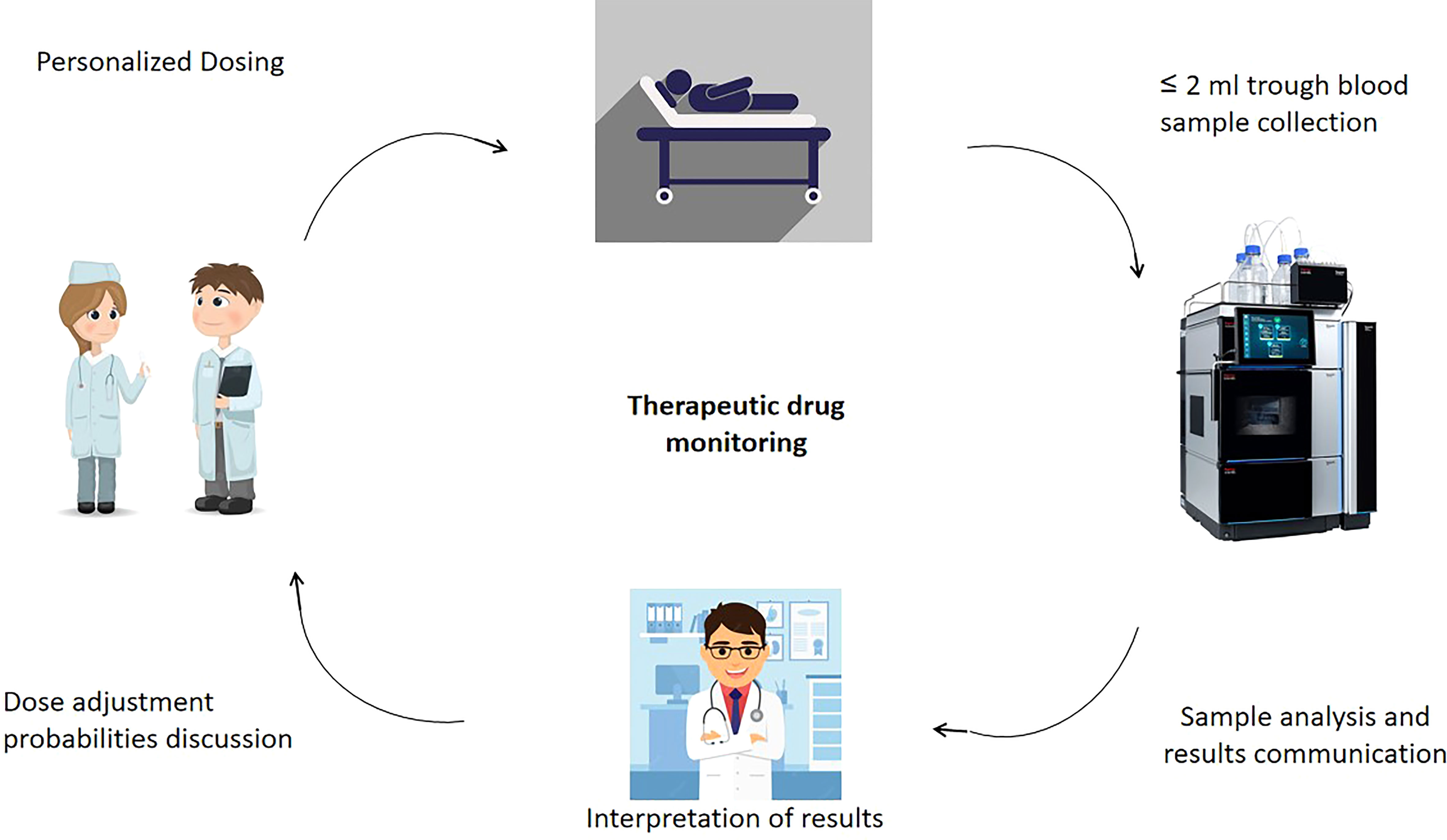
Tacrolimus and cyclosporine are common immunosuppressants whose levels in the blood must be routinely measured to ensure they are within the therapeutic range.
Another example is warfarin, an anticoagulant used to prevent blood clots. Warfarin, while effective, requires regular monitoring of the International Normalized Ratio (INR) to prevent both bleeding and clotting complications.
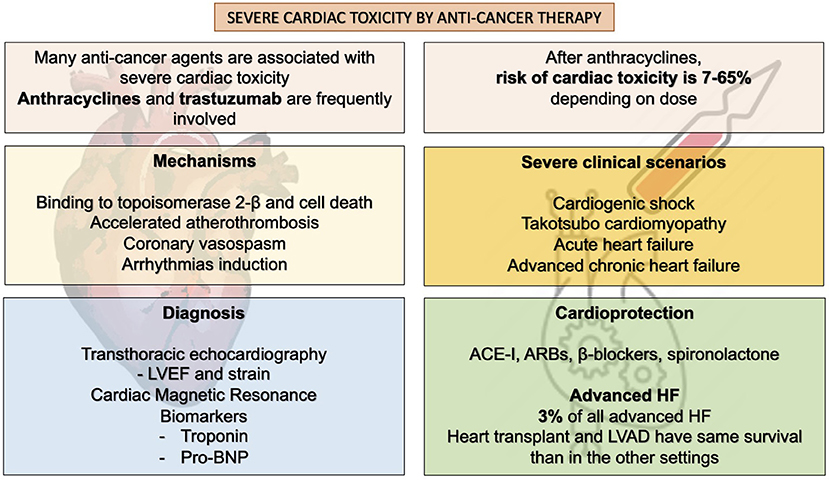
Furthermore, chemotherapeutic agents, while targeting cancer cells, can also damage healthy cells, leading to a range of toxicities, including bone marrow suppression, nausea, and hair loss. Regular blood counts and liver function tests are essential for patients undergoing chemotherapy.
Antiarrhythmic drugs like amiodarone, used to treat irregular heartbeats, can cause thyroid, lung, and liver problems. Routine monitoring of thyroid function, pulmonary function, and liver enzymes is recommended for patients on amiodarone.
The Role of Pharmacovigilance
Pharmacovigilance, the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other drug-related problem, plays a crucial role in identifying and managing drug toxicities.
Regulatory agencies like the Food and Drug Administration (FDA) in the United States and the European Medicines Agency (EMA) in Europe rely on pharmacovigilance data to make informed decisions about drug safety and labeling.
These agencies also issue warnings and recommendations based on emerging safety concerns. Hospitals and healthcare providers also have their own pharmacovigilance programs to track and report adverse drug events.
Challenges and Solutions in Monitoring
Monitoring drug toxicity is not without its challenges. Patient adherence to monitoring schedules can be a major obstacle, as can access to timely laboratory testing, especially in underserved areas.
Moreover, the complexity of drug interactions and individual patient variability can make it difficult to predict who will experience toxicity and at what dose. Technological advancements offer promising solutions.
Point-of-care testing, for instance, allows for rapid blood level monitoring in the clinic or even at home, improving patient convenience and adherence. Electronic health records (EHRs) can also be used to track patient medication histories and lab results, alerting providers to potential drug interactions and toxicities.
Pharmacogenomics, the study of how genes affect a person's response to drugs, holds promise for personalizing drug therapy and predicting who is at higher risk of toxicity.
By identifying genetic markers associated with drug metabolism and toxicity, healthcare providers can tailor drug selection and dosing to individual patients, minimizing the risk of adverse events.
The Patient Perspective
For patients taking medications requiring intensive monitoring, the process can be burdensome and anxiety-provoking. Frequent blood draws, doctor visits, and the constant awareness of potential side effects can take a toll on their quality of life.
It is essential that healthcare providers communicate clearly and compassionately with patients about the risks and benefits of their medications, as well as the importance of adherence to monitoring schedules.
Patient education and engagement are critical for ensuring successful drug therapy. Patients who understand their medications and the potential side effects are more likely to adhere to monitoring schedules and report any concerning symptoms promptly.
The Future of Drug Safety
The field of drug safety is constantly evolving, with new technologies and strategies emerging to improve patient outcomes. Artificial intelligence (AI) and machine learning (ML) are being used to analyze large datasets of patient information and identify patterns that may predict drug toxicity.
These tools can help healthcare providers proactively identify patients at risk and intervene before serious adverse events occur. Furthermore, research into new drug delivery systems, such as targeted nanoparticles, aims to deliver drugs directly to affected tissues, reducing systemic exposure and minimizing toxicity.
Ultimately, the goal is to develop safer and more effective medications that can improve patient health without compromising their well-being. As medical science advances, the hope is that the need for intensive monitoring will diminish, replaced by more personalized and less toxic therapies.