Established The First Medicare Prospective Payment System

A seismic shift in healthcare financing occurred when the first Medicare Prospective Payment System (PPS) was established. This landmark reform fundamentally altered how hospitals were reimbursed, moving from a retrospective, cost-based model to a prospective, fixed-rate system.
The establishment of the PPS marked a turning point in controlling healthcare costs and incentivizing efficiency within the Medicare program. Implemented to curb escalating hospital expenditures, the system reimbursed hospitals based on pre-determined rates for specific diagnoses, rather than actual costs incurred.
The Genesis of PPS
The driving force behind the PPS was the soaring cost of healthcare under the traditional cost-based reimbursement system. This system, implemented since the inception of Medicare in 1965, incentivized hospitals to increase spending, leading to unsustainable growth in Medicare outlays.
Lawmakers and healthcare experts recognized the need for a more structured and predictable payment mechanism. The goal was to create a system that would promote cost-effectiveness and accountability in hospital care.
Key Legislation: The Social Security Amendments of 1983
The foundation for the PPS was laid with the enactment of the Social Security Amendments of 1983. This legislation, specifically Section 601, mandated the implementation of a prospective payment system for inpatient hospital services under Medicare.
This legislative act provided the legal and structural framework for the radical change in Medicare reimbursement.
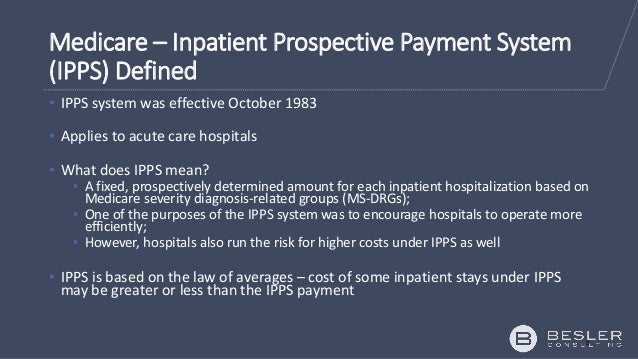
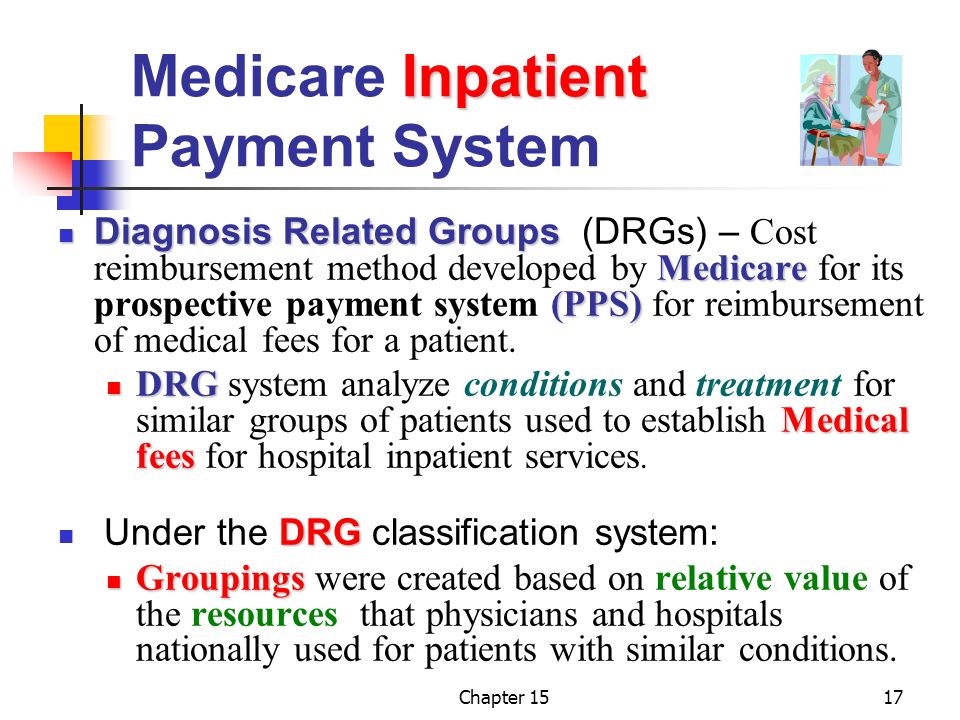
The Diagnosis-Related Group (DRG) System
At the heart of the PPS was the adoption of the Diagnosis-Related Group (DRG) system. DRGs categorized illnesses and conditions into distinct groups, assigning a fixed payment rate to each group based on the average cost of treating that condition.
Hospitals would receive a pre-determined payment based on the patient’s DRG, regardless of the actual cost of treatment. This incentivized hospitals to manage resources efficiently and reduce unnecessary expenditures.
Implementation and Impact
The PPS was phased in starting in 1983, initially affecting inpatient hospital services. Over time, it was expanded to other areas of healthcare, including skilled nursing facilities, home health agencies, and outpatient services.
The immediate impact was a significant slowdown in the growth of Medicare hospital expenditures. Data showed a marked decrease in the rate of increase in hospital costs compared to the pre-PPS era.
Hospitals, faced with fixed payment rates, began to implement cost-saving measures, such as reducing length of stay and improving efficiency in resource utilization.
Criticisms and Challenges
Despite its success in controlling costs, the PPS faced criticism from various quarters. Some argued that it incentivized hospitals to discharge patients prematurely or to skimp on necessary care to maximize profits.
Concerns were also raised about the accuracy of DRG classifications and the potential for hospitals to "game" the system by manipulating diagnoses to receive higher payments.
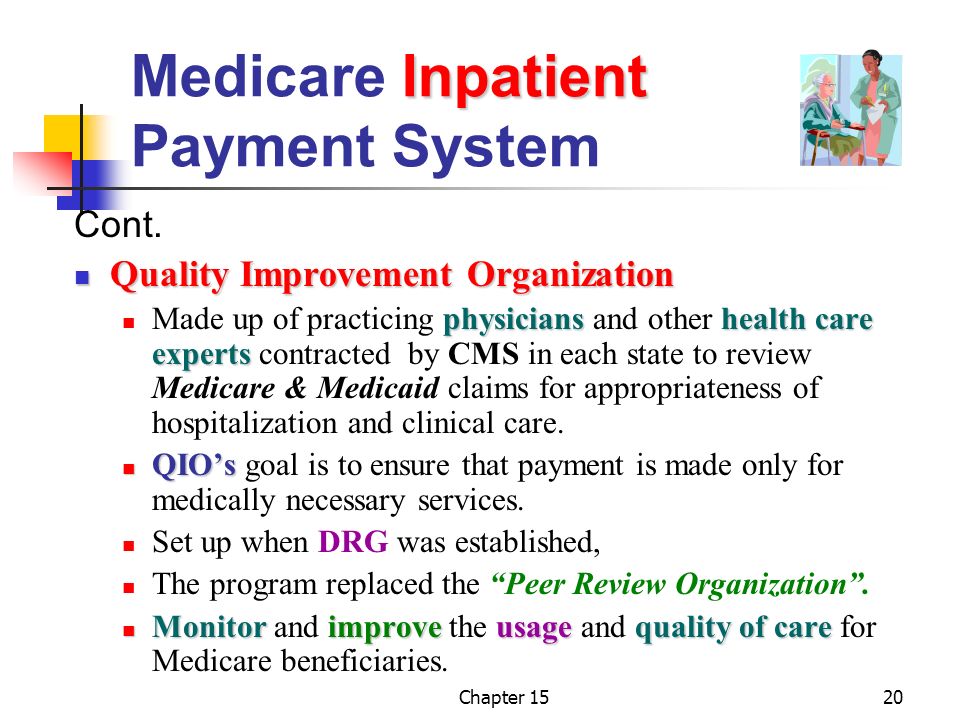
Adjustments and refinements have been continuously made to the PPS to address these concerns and ensure that quality of care is not compromised.
The Ongoing Evolution of Medicare Reimbursement
The establishment of the PPS was not a one-time event, but rather the beginning of an ongoing evolution in Medicare reimbursement methodologies. The system continues to be refined and adapted to address emerging challenges in the healthcare landscape.
Efforts are underway to incorporate value-based payment models that reward hospitals for providing high-quality, cost-effective care. This involves tying reimbursement to patient outcomes and satisfaction, rather than simply the volume of services provided.
Looking Ahead
The legacy of the first Medicare PPS is profound, having fundamentally reshaped healthcare financing in the United States. Its impact continues to be felt as policymakers and healthcare providers grapple with the challenge of balancing cost containment and quality of care.
Ongoing research and innovation are crucial to ensuring that the Medicare reimbursement system remains sustainable and effective in meeting the evolving needs of the nation’s aging population.
Future developments are expected to focus on further refining DRG classifications, incorporating measures of patient outcomes and satisfaction, and promoting greater collaboration and coordination of care across different healthcare settings. The ultimate goal is to create a healthcare system that delivers high-quality, affordable care for all beneficiaries.





.jpg)