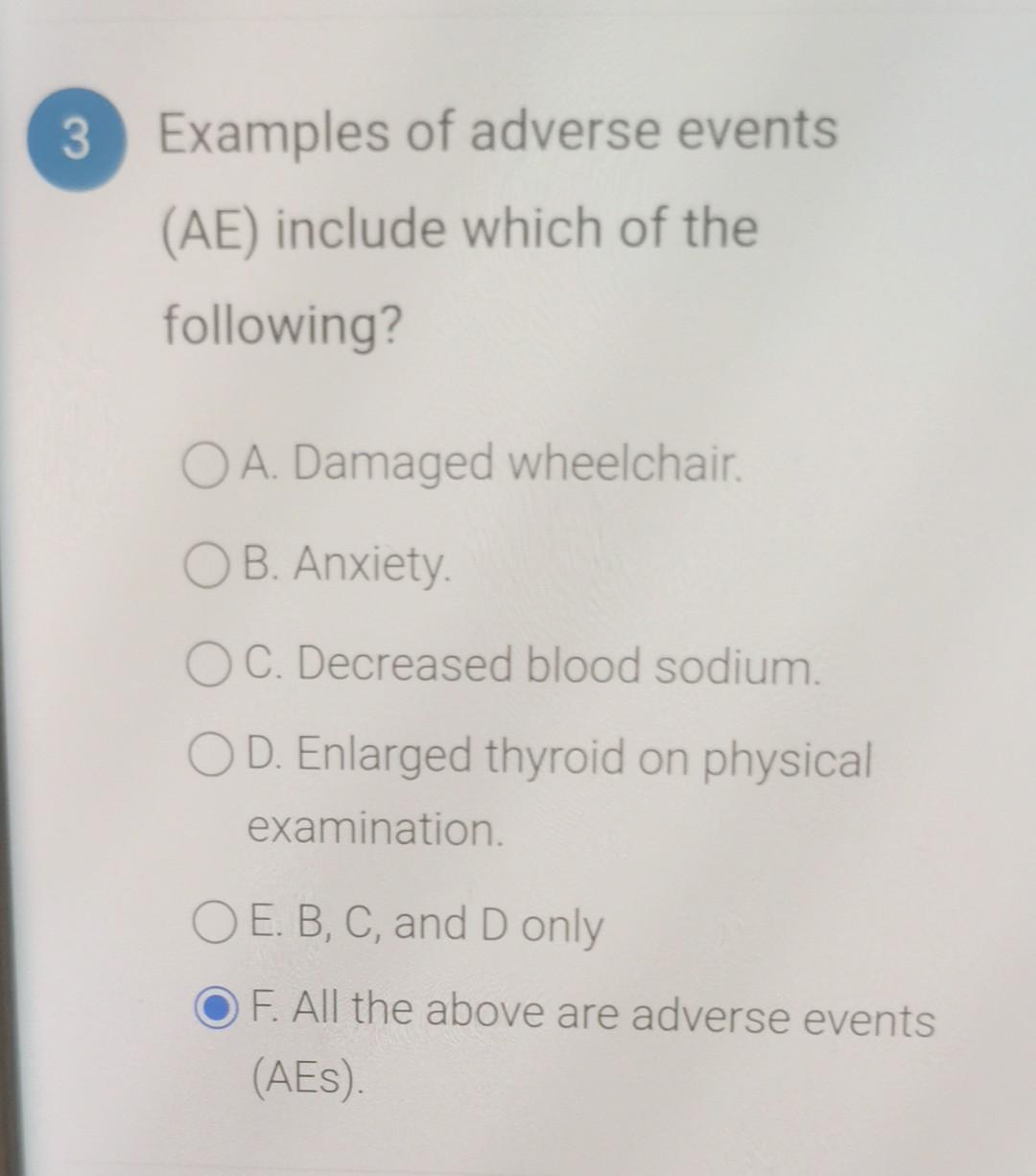
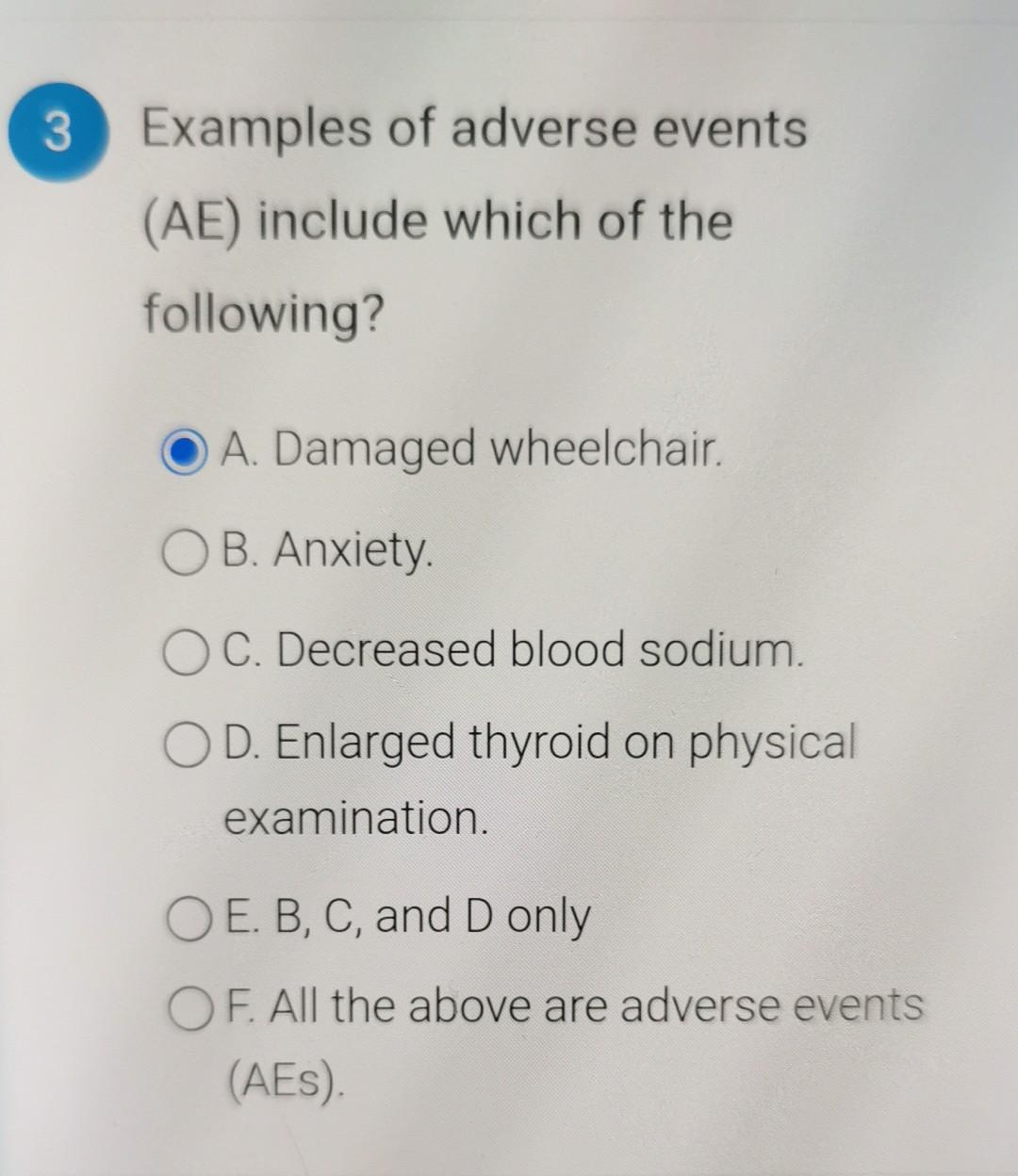
Examples Of Adverse Events Ae Include Which Of The Following
A surge in adverse event reports has triggered a nationwide investigation into the understanding and recognition of potential harms across healthcare settings. Understanding what constitutes an adverse event (AE) is critical for patient safety and effective reporting, yet confusion persists, leading to underreporting and potentially compromised care.
The core issue centers on defining and recognizing adverse events (AEs). Discrepancies in identifying AEs hamper data collection and analysis, vital for preventing future incidents and improving patient outcomes. The lack of clarity impacts healthcare providers, patients, and regulatory bodies alike.
What Constitutes an Adverse Event?
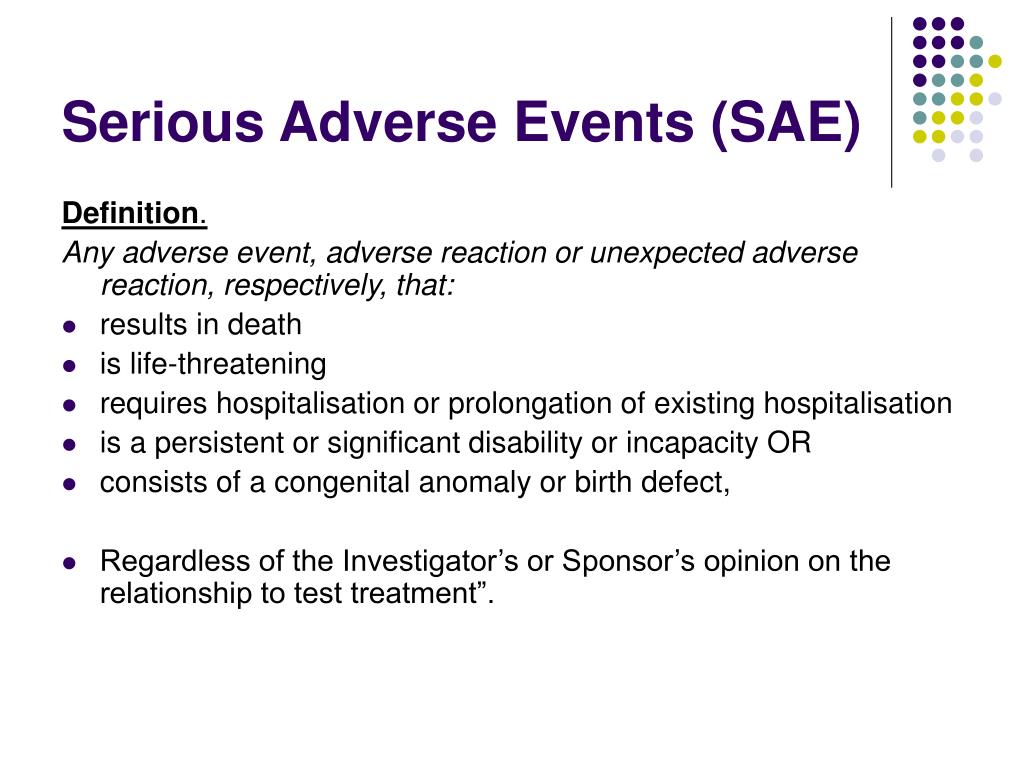
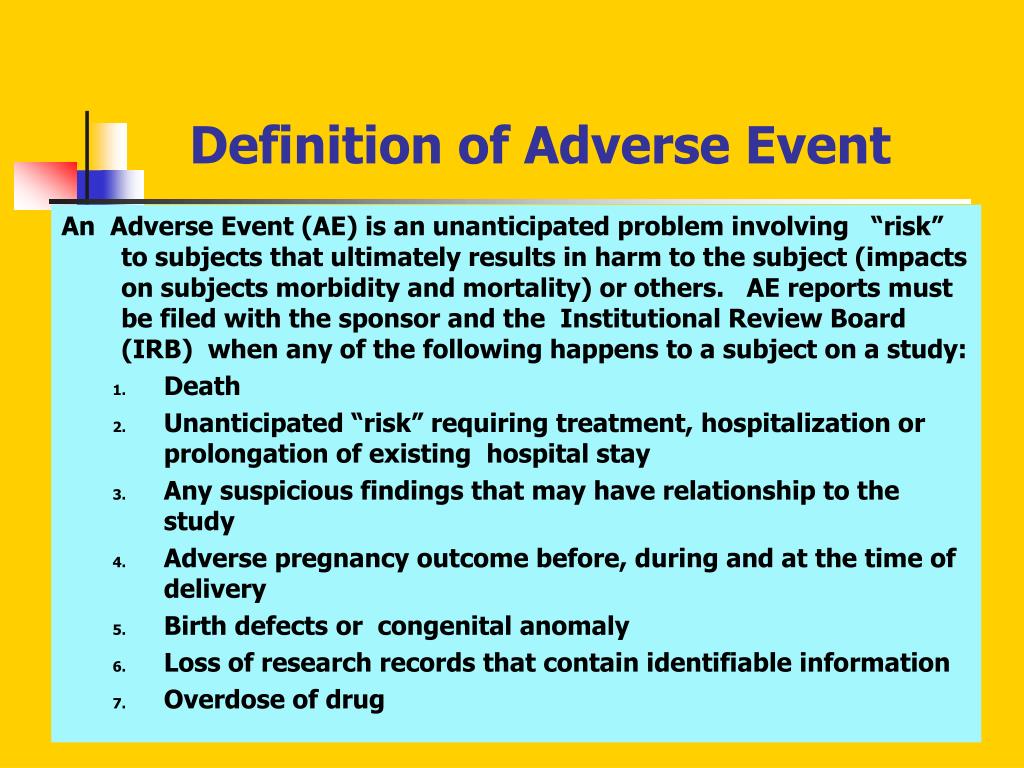
An adverse event, in its simplest form, is any undesirable experience associated with the use of a medical product or procedure. It's important to understand examples include medication side effects, surgical complications, device malfunctions, and diagnostic errors.
However, the nuances are often complex. An adverse event doesn't necessarily imply negligence or an error. It simply means an unexpected and undesirable outcome occurred during or after medical intervention.
Common Examples of Adverse Events
Medication Errors: These range from prescribing the wrong dose to administering the wrong medication, or failing to account for drug interactions. These errors can result in serious harm, including organ damage or death.
Surgical Complications: This includes infections, bleeding, nerve damage, and anesthesia-related problems. While some complications are unavoidable risks of surgery, others may stem from procedural errors or inadequate post-operative care.
Healthcare-Associated Infections (HAIs): Infections acquired in a hospital or other healthcare setting are a significant concern. Common HAIs include pneumonia, bloodstream infections, and surgical site infections.
Diagnostic Errors: Delayed, inaccurate, or missed diagnoses can have devastating consequences. These errors can lead to delayed treatment, inappropriate treatment, or disease progression.
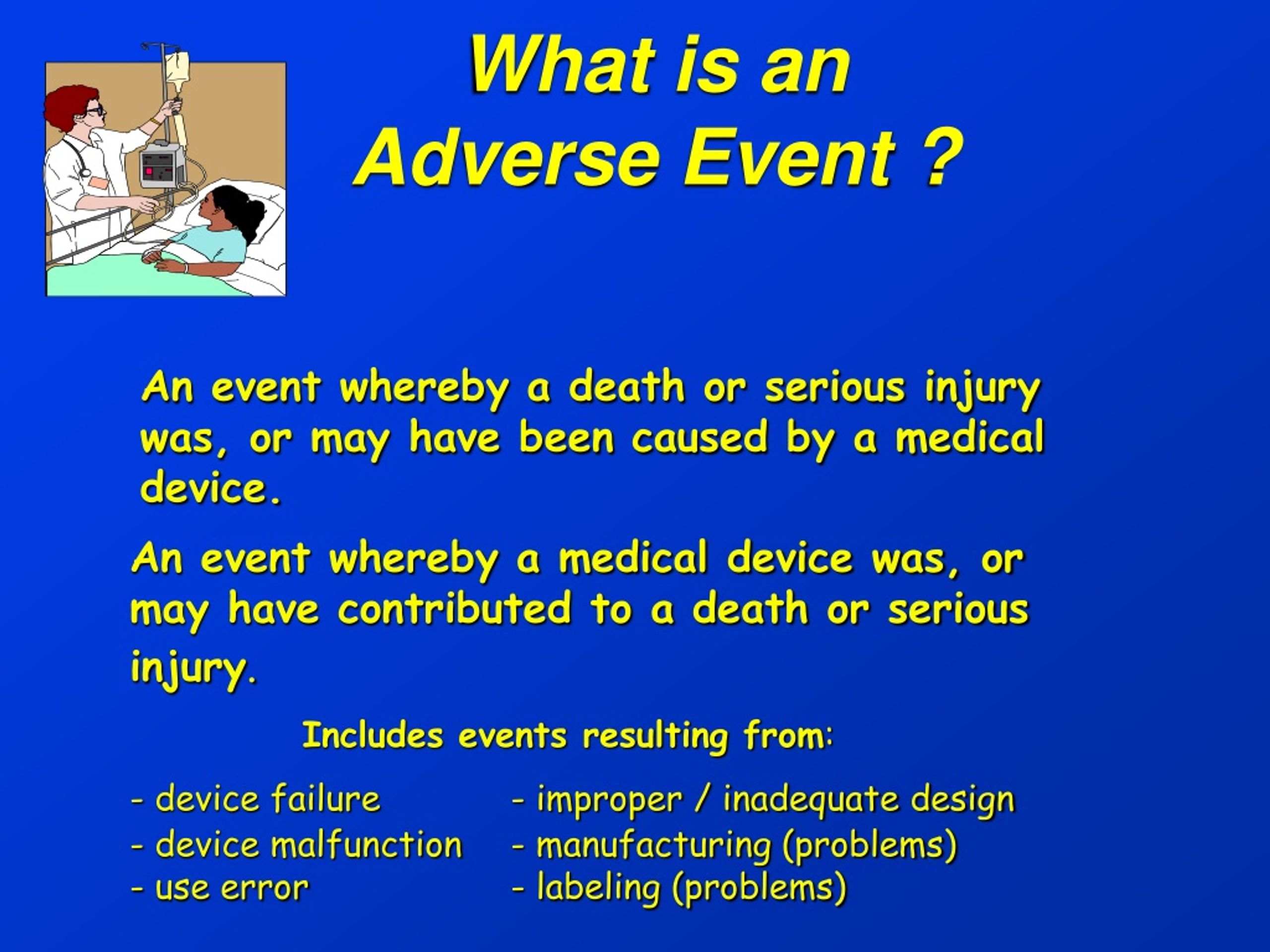
Medical Device Malfunctions: When medical devices fail to function as intended, it can cause serious harm. This includes implanted devices, monitoring equipment, and surgical instruments.
Falls: Particularly common in elderly patients, falls can lead to fractures, head injuries, and other complications. Healthcare facilities are obligated to implement fall prevention programs.
Pressure Ulcers (Bedsores): These develop when pressure is applied to the skin for prolonged periods, often in immobile patients. Proper preventative measures are crucial.
The Critical Need for Accurate Reporting
Accurate and timely reporting of adverse events is paramount. It allows healthcare providers and regulatory agencies to identify trends, implement corrective actions, and prevent future occurrences.
Underreporting is a significant obstacle. Fear of legal repercussions, lack of time, and complex reporting procedures often deter healthcare professionals from reporting AEs.
The FDA (Food and Drug Administration) maintains a database for adverse event reporting called MedWatch. This system allows healthcare professionals and consumers to voluntarily report AEs associated with medical products.
Who Is Affected?
The impact of unclear AE understanding reaches across the healthcare spectrum. Patients are directly affected by preventable harm stemming from these events.
Healthcare providers face increased liability risks. Institutions bear the burden of managing and mitigating the consequences of AEs.
Ongoing Efforts and Next Steps
Several initiatives are underway to improve AE identification and reporting. These include standardized definitions, simplified reporting processes, and enhanced training programs for healthcare professionals.
The National Quality Forum (NQF) and other organizations are developing standardized measures. The goal is to track and reduce the incidence of AEs across various healthcare settings.
Further research is needed to fully understand the scope and impact of AEs. This research should focus on identifying risk factors, developing effective prevention strategies, and improving patient safety outcomes.
Healthcare organizations must prioritize a culture of safety. This includes promoting transparency, encouraging open communication, and fostering a blame-free environment for reporting AEs.
Continued vigilance and collaborative efforts are crucial to mitigating the risk of adverse events. Improved understanding and reporting are essential steps in safeguarding patient well-being.

.jpg)
.jpg)
+is….jpg)
-Adverse+Reaction+(AR).jpg)

.jpg)


+Reporting:+Finding+Appropriate+AE+Terms.jpg)
+Serious+Adverse+Event+(SAE).jpg)
