Factors That Supported The Development Of Advanced Nursing Practice

Advanced Practice Registered Nurses (APRNs) are rapidly reshaping healthcare delivery, filling critical gaps and driving innovation. Multiple forces have converged to fuel this expansion, demanding immediate attention to regulatory and educational frameworks.
This article dissects the key factors propelling the growth of advanced nursing practice, emphasizing the urgent need for adaptation and strategic planning within the healthcare landscape.
The Rising Demand for Healthcare Services
The aging population is significantly increasing the demand for chronic disease management and geriatric care. This demographic shift necessitates readily accessible and cost-effective healthcare solutions.
APRNs, with their expanded scope of practice, are uniquely positioned to address these evolving needs, particularly in underserved areas.
Physician Shortages and Uneven Distribution
The United States continues to face critical physician shortages, especially in primary care and rural settings. These shortages create significant barriers to access, hindering timely and effective healthcare delivery.
APRNs are stepping in to bridge these gaps, providing essential primary and specialty care services to communities in need.
Emphasis on Cost-Effective Care Delivery
Healthcare costs are spiraling, prompting a relentless search for innovative and cost-effective care models. APRNs offer a compelling solution, often providing comparable or even superior outcomes at a lower cost.
Studies have demonstrated the cost-effectiveness of APRN-led interventions in managing chronic conditions and preventing hospital readmissions.
Advancements in Nursing Education
The increasing rigor and specialization of nursing education are producing highly skilled and knowledgeable APRNs. Master's and doctoral programs are equipping nurses with advanced clinical skills and leadership capabilities.
This enhanced educational foundation enables APRNs to practice at the forefront of healthcare, implementing evidence-based practices and driving quality improvement initiatives. The National Organization of Nurse Practitioner Faculties (NONPF) has played a crucial role in standardizing NP education.
Legislative and Regulatory Changes
State-level legislation and regulations significantly impact the scope of practice for APRNs. Full practice authority, which allows APRNs to practice to the full extent of their education and training, is a critical enabler.
States granting full practice authority generally experience improved access to care, especially in rural and underserved communities. Organizations like the American Association of Nurse Practitioners (AANP) actively advocate for these changes.
The Evolution of Healthcare Technology
The rapid adoption of telehealth and other digital health technologies is expanding the reach and efficiency of APRNs. Telehealth allows APRNs to provide remote consultations, manage chronic conditions, and deliver timely interventions.
These technologies enhance access to care, improve patient engagement, and facilitate collaborative practice among healthcare professionals.
Increased Patient Acceptance and Satisfaction
Patients are increasingly recognizing and appreciating the value that APRNs bring to healthcare. Studies consistently show high levels of patient satisfaction with APRN-provided care.
This positive perception fosters trust and collaboration, contributing to improved health outcomes and enhanced patient experiences.
Focus on Preventative Care and Wellness
The healthcare system is shifting its focus from reactive treatment to proactive prevention and wellness promotion. APRNs are well-equipped to lead these efforts, providing health education, screening services, and lifestyle counseling.
Their emphasis on holistic care and patient empowerment aligns perfectly with the goals of preventive medicine.
Collaborative Practice Models
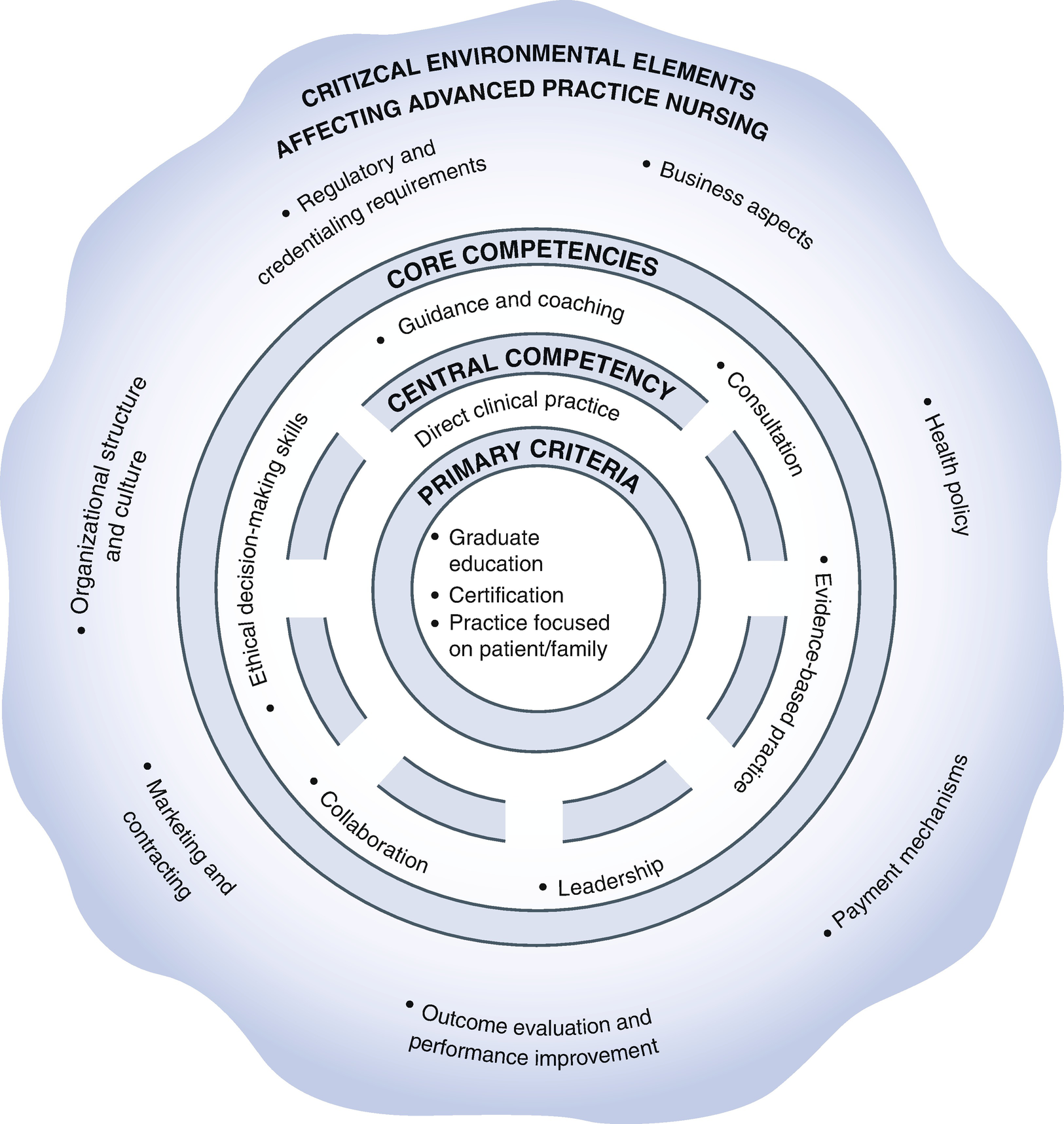
Collaborative practice models, where APRNs work in partnership with physicians and other healthcare professionals, are becoming increasingly common. These models leverage the unique skills and expertise of each provider, optimizing patient care and improving team efficiency.
Effective communication and mutual respect are essential components of successful collaborative practice.
Data Demonstrating Impact
Research consistently shows that APRNs provide high-quality care comparable to physicians, often with better patient satisfaction scores. For example, a 2018 study published in Health Affairs found that nurse practitioners could effectively manage chronic conditions like diabetes and hypertension.
Furthermore, data suggests that expanding APRN scope of practice is linked to improved access in underserved areas.
Conclusion: Navigating the Future of Advanced Practice Nursing
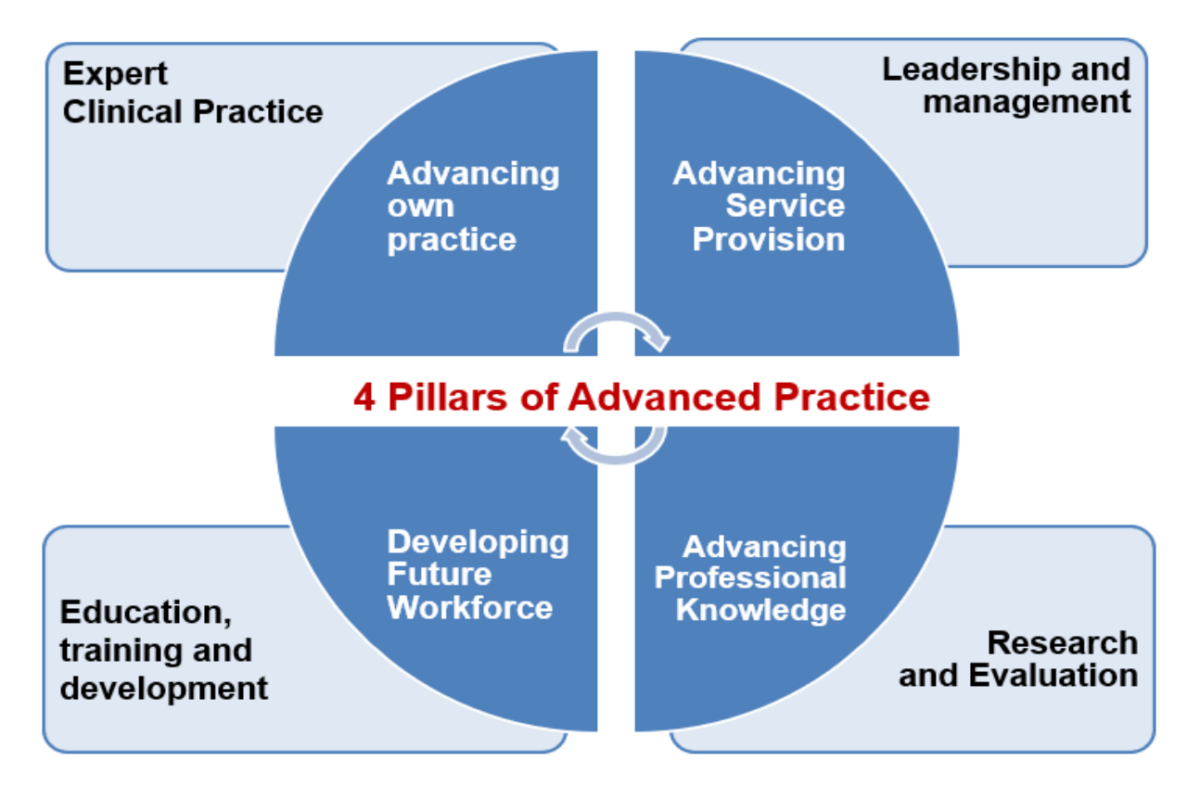
The factors supporting the growth of advanced nursing practice are multifaceted and interconnected. Ongoing efforts must focus on standardizing education, advocating for full practice authority, and promoting collaborative care models.
Continued research is crucial to demonstrate the value of APRNs and inform policy decisions. Failing to address these issues will compromise access to quality healthcare and hinder the ongoing evolution of the healthcare system. Immediate action is needed to optimize the role of APRNs and ensure they can effectively meet the growing demands of a changing healthcare landscape.