Fatty Infiltration Of Pancreas Means

The pancreas, a vital organ tucked behind the stomach, plays a crucial role in digestion and blood sugar regulation. Increasingly, this organ is facing a silent threat: fatty infiltration, also known as pancreatic steatosis. What was once considered a relatively benign finding is now emerging as a potential risk factor for serious health complications, demanding closer attention from both researchers and clinicians.
Fatty infiltration of the pancreas, the accumulation of fat within the pancreatic tissue, is no longer seen as a mere bystander. It's now understood to be potentially linked to pancreatitis, diabetes, and even pancreatic cancer. This condition warrants closer examination and proactive management, presenting a call to action for improved diagnostics and preventative strategies. This article delves into the intricacies of pancreatic steatosis, exploring its causes, potential consequences, diagnostic approaches, and current management strategies.
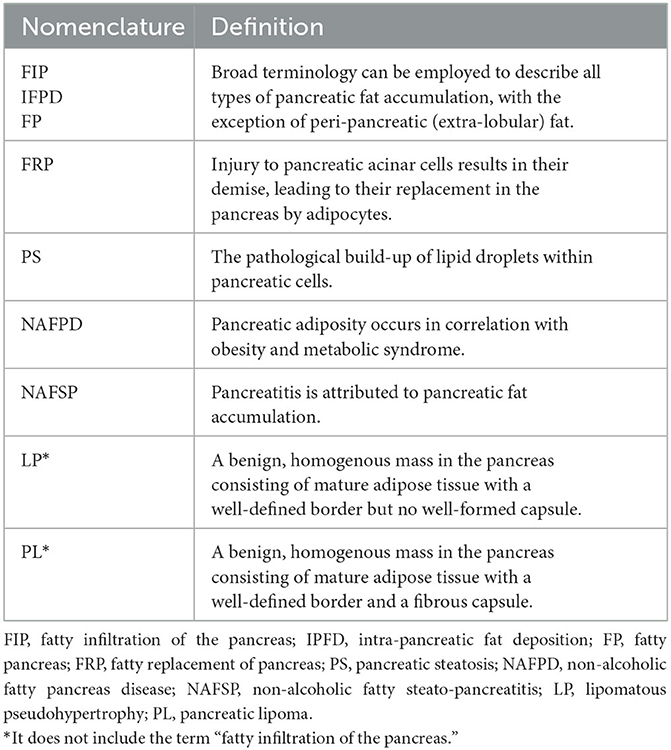
Understanding Pancreatic Steatosis
Fatty infiltration of the pancreas occurs when 5-10% of the pancreas weight is from fat. It happens when triglycerides accumulate in the organ's cells. Several factors can contribute to this buildup, including obesity, metabolic syndrome, type 2 diabetes, and high alcohol consumption.
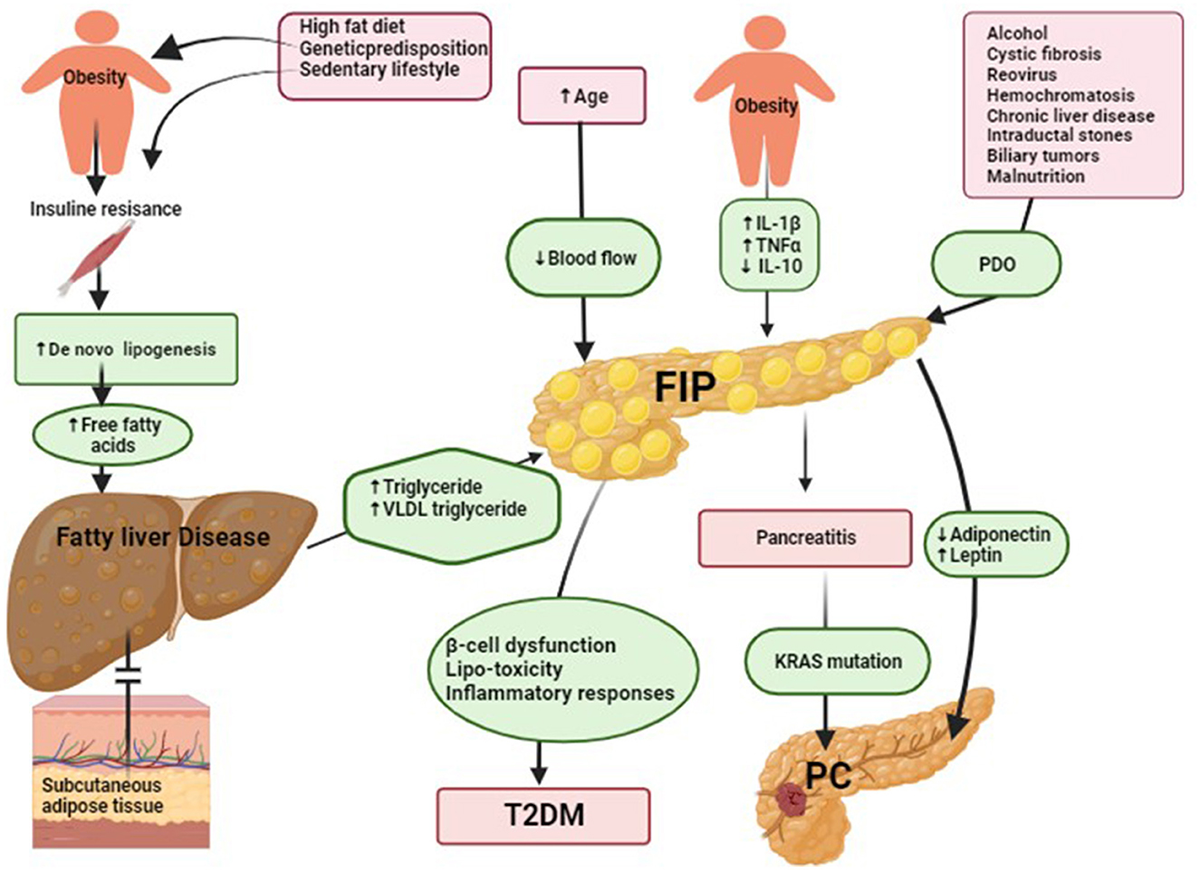
Causes and Risk Factors
Obesity is a leading cause, as excess body fat often leads to fat deposition in various organs, including the pancreas. Metabolic syndrome, a cluster of conditions including high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, also significantly increases the risk. Type 2 diabetes, often linked to insulin resistance, further exacerbates the problem. Chronic alcohol abuse is another well-established risk factor.
Other potential causes include certain medications, genetic predispositions, and specific medical conditions like cystic fibrosis. Age also plays a role, with the prevalence of pancreatic steatosis generally increasing with age. Interestingly, rapid weight loss, while generally beneficial, can sometimes temporarily increase fat accumulation in the pancreas.
Potential Consequences
While some individuals with fatty infiltration of the pancreas may experience no symptoms, others may face serious health consequences. The most significant concern is an increased risk of acute pancreatitis, a painful inflammation of the pancreas. Studies have shown a clear association between pancreatic steatosis and the severity of acute pancreatitis episodes.
Furthermore, fatty infiltration can impair the pancreas's ability to produce insulin, potentially leading to or worsening type 2 diabetes. Emerging research suggests a possible link between pancreatic steatosis and an increased risk of pancreatic cancer. The exact mechanisms behind this association are still being investigated, but the findings warrant serious attention.
Diagnosis and Management
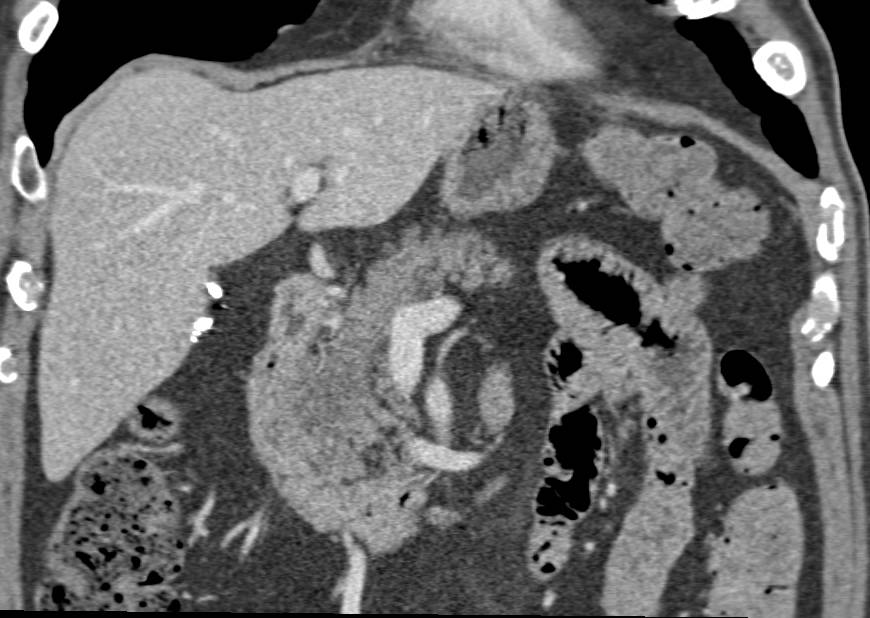
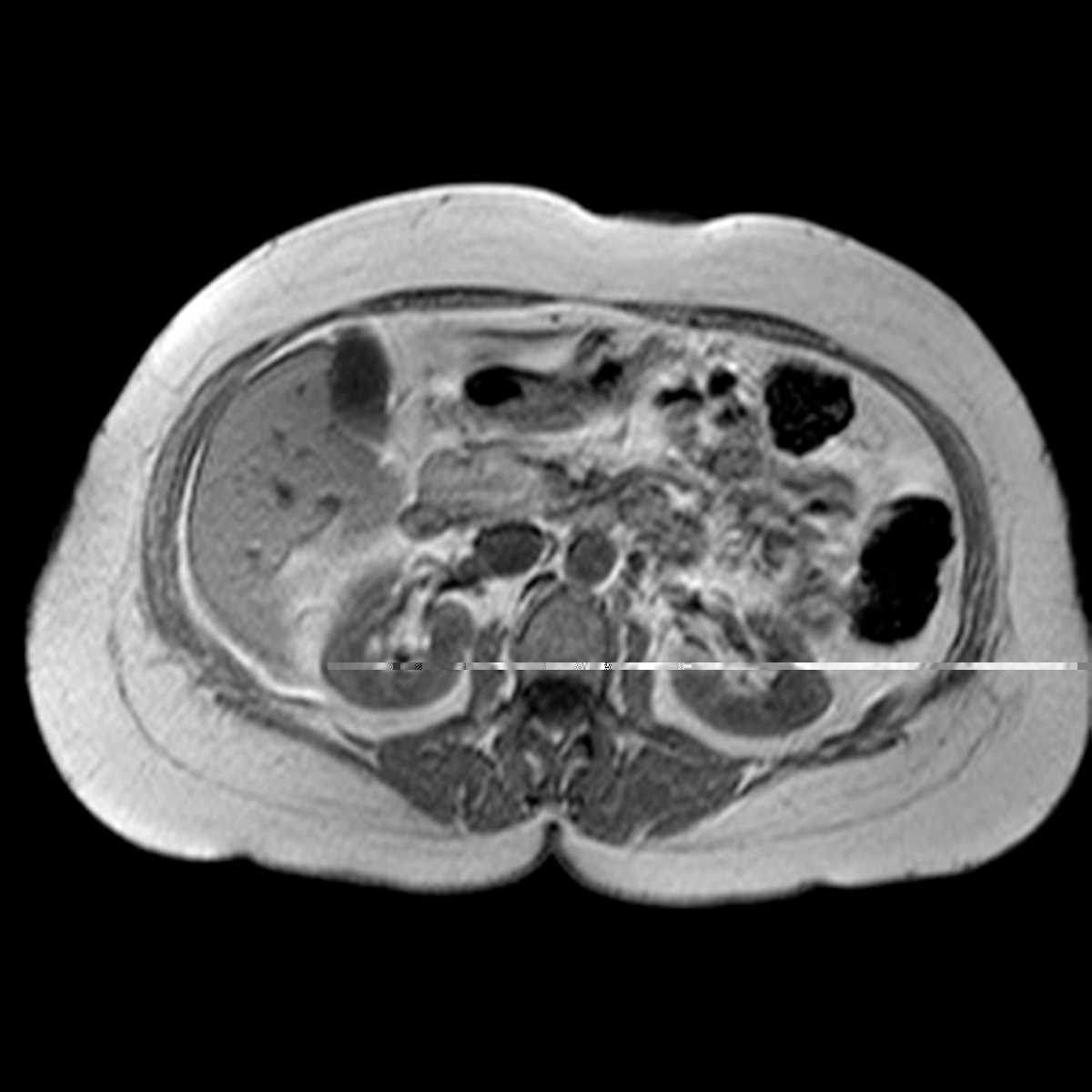
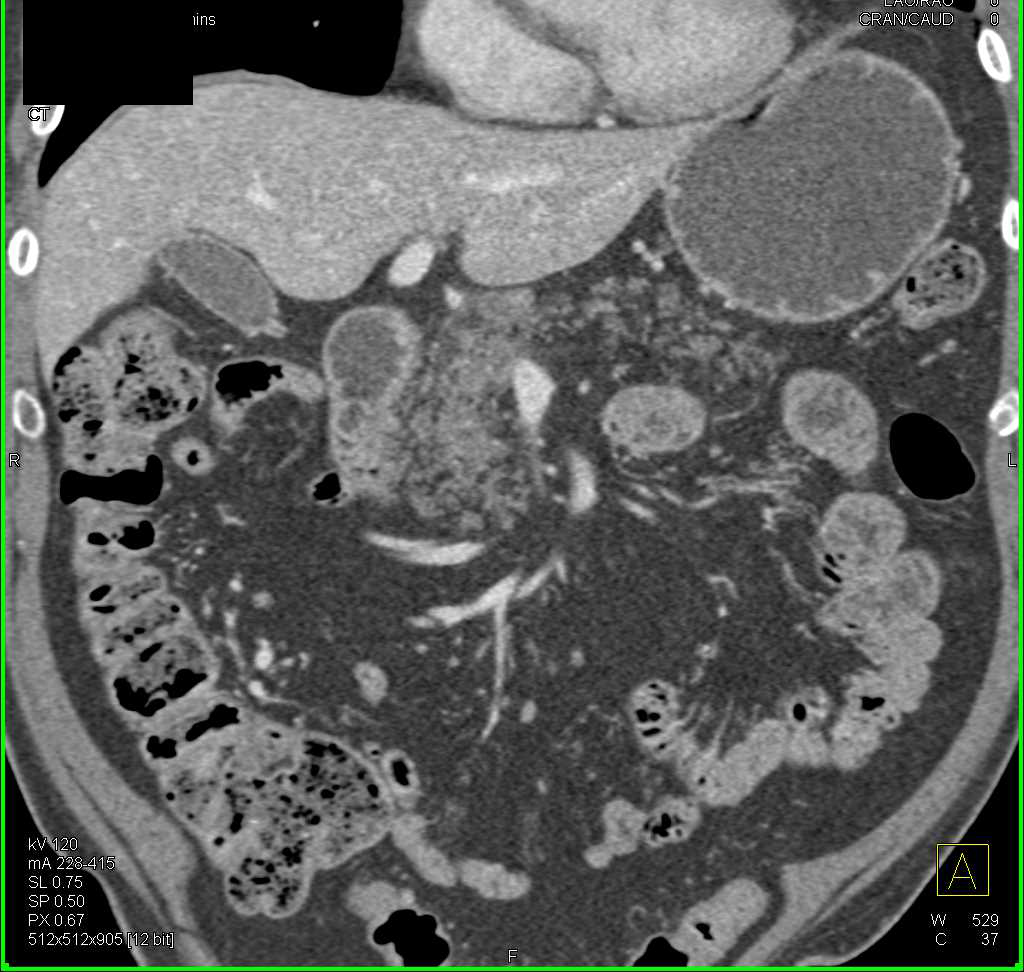
Diagnosing fatty infiltration of the pancreas can be challenging, as it often presents without specific symptoms. Imaging techniques such as computed tomography (CT) scans and magnetic resonance imaging (MRI) are commonly used to detect fat accumulation in the pancreas. Newer techniques like magnetic resonance spectroscopy (MRS) offer more precise quantification of fat content.
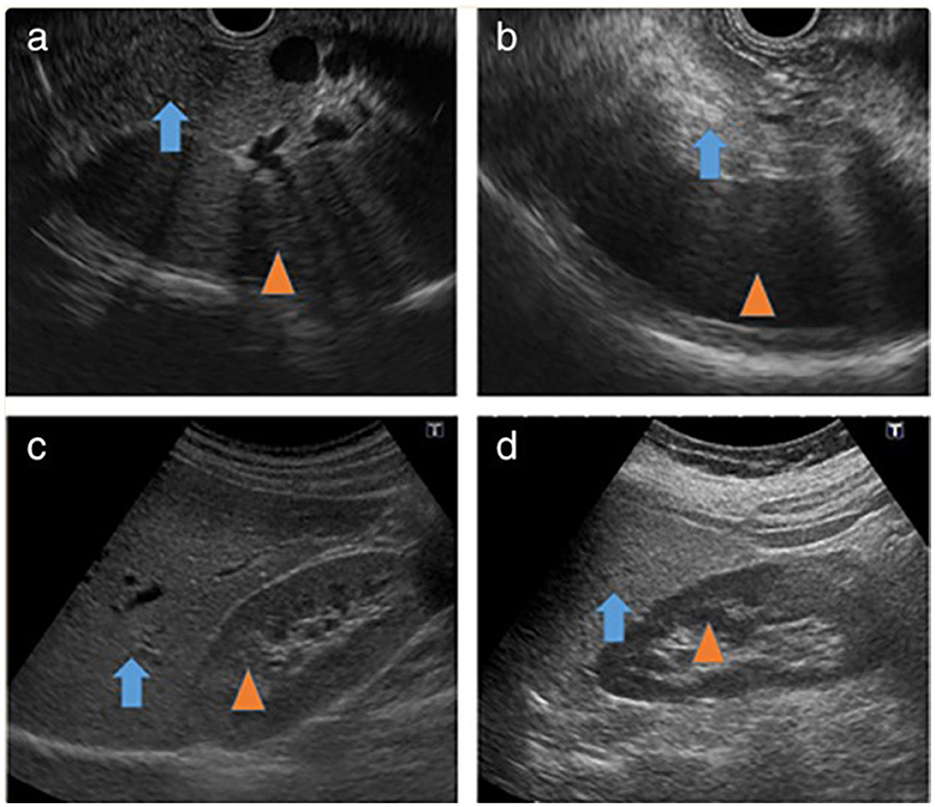
Endoscopic ultrasound (EUS) can also be used, providing detailed images of the pancreas. Currently, there are no specific medications approved to treat fatty infiltration of the pancreas directly. Lifestyle modifications are the cornerstone of management.
Treatment Strategies
Weight loss through diet and exercise is crucial for reducing fat accumulation in the pancreas. A healthy diet rich in fruits, vegetables, and whole grains, and low in processed foods, saturated fats, and added sugars is recommended. Regular physical activity can help improve insulin sensitivity and reduce overall body fat.
For individuals with underlying conditions like diabetes or metabolic syndrome, managing these conditions effectively is essential. This may involve medications to control blood sugar, blood pressure, and cholesterol levels. Abstaining from alcohol is crucial for individuals whose pancreatic steatosis is linked to alcohol abuse.
Close monitoring of pancreatic function is important, especially in individuals with risk factors for pancreatitis or diabetes. Regular follow-up with a healthcare provider is necessary to assess the effectiveness of treatment strategies and detect any potential complications early.
The Future of Research and Treatment
Research into fatty infiltration of the pancreas is rapidly evolving. Scientists are working to better understand the underlying mechanisms that contribute to the development of this condition. They are also exploring potential new therapies that could target fat accumulation in the pancreas directly.
Future research will likely focus on identifying specific biomarkers that can predict the risk of developing pancreatic steatosis and its associated complications. Clinical trials are needed to evaluate the effectiveness of various interventions, including lifestyle modifications, medications, and novel therapeutic approaches.
Ultimately, raising awareness about the risk factors and potential consequences of fatty infiltration of the pancreas is crucial for promoting early detection and prevention. A proactive approach, including healthy lifestyle choices and regular medical check-ups, can help protect the health of this vital organ.