Fluid And Electrolyte Imbalance Nursing Care Plan

Imagine a sweltering summer day. You're sweating profusely after a vigorous workout, feeling parched and lightheaded. This experience, though common, offers a glimpse into the critical importance of maintaining the delicate balance of fluids and electrolytes within our bodies. When this balance is disrupted, the consequences can range from mild discomfort to life-threatening complications.
This article explores the intricacies of fluid and electrolyte imbalances, shedding light on their significance, causes, assessment, and the crucial role of nursing care plans in addressing them effectively. We'll delve into how nurses develop personalized strategies to restore equilibrium and prevent further complications, ensuring optimal patient outcomes.
The Foundation: Understanding Fluid and Electrolyte Balance
Our bodies are finely tuned machines, and fluid and electrolyte balance is a cornerstone of their proper functioning. Fluids, primarily water, act as a transport medium for nutrients and waste products, regulate body temperature, and lubricate joints.
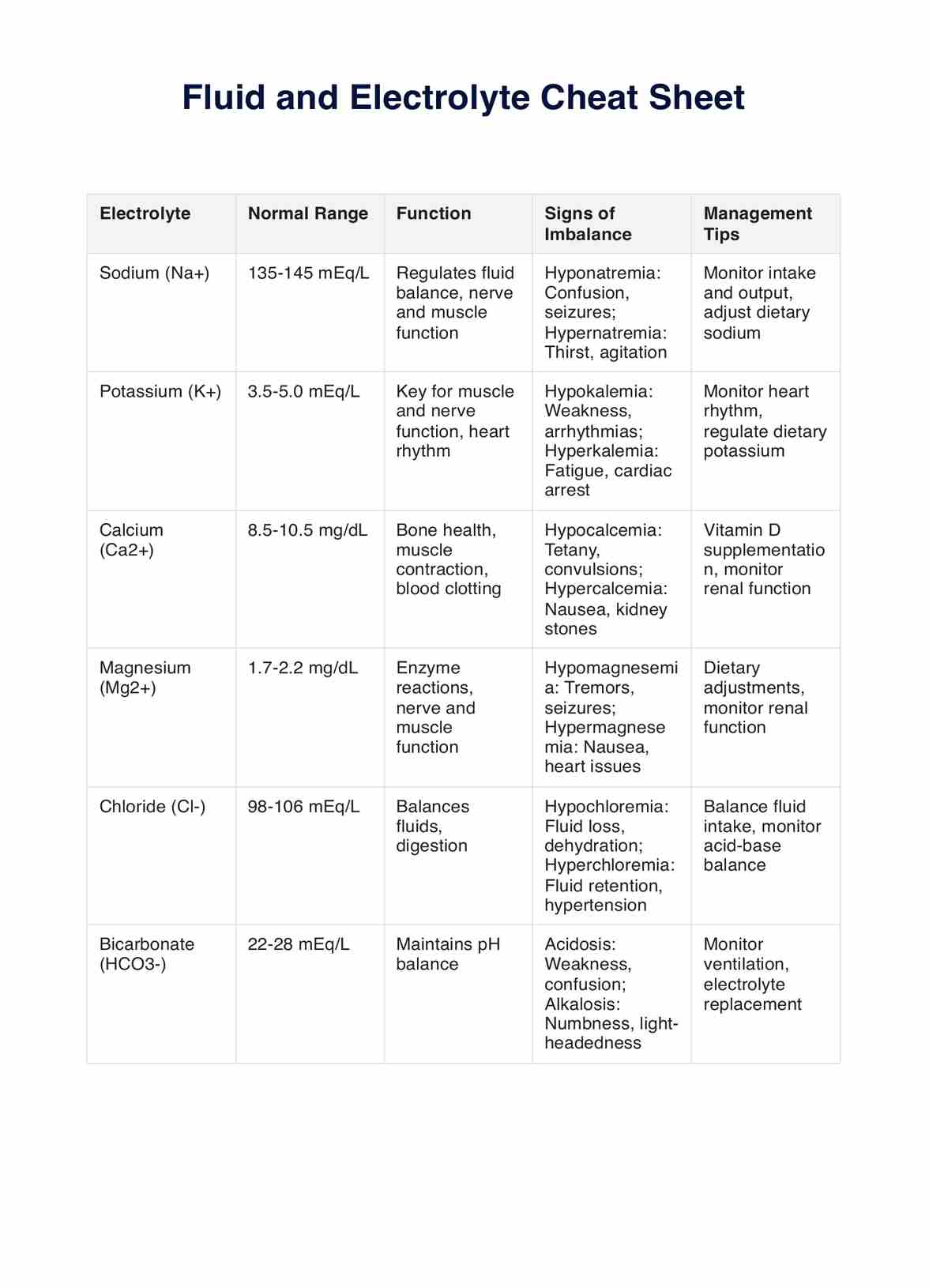
Electrolytes, such as sodium, potassium, calcium, and magnesium, are minerals that carry an electrical charge and play vital roles in nerve impulse transmission, muscle contraction, and maintaining cell function.
Maintaining this equilibrium requires a delicate interplay between fluid intake, fluid output (through urine, sweat, respiration, and feces), and electrolyte regulation. Any disruption to these processes can lead to an imbalance.
Why Does It Matter? The Ripple Effect of Imbalance
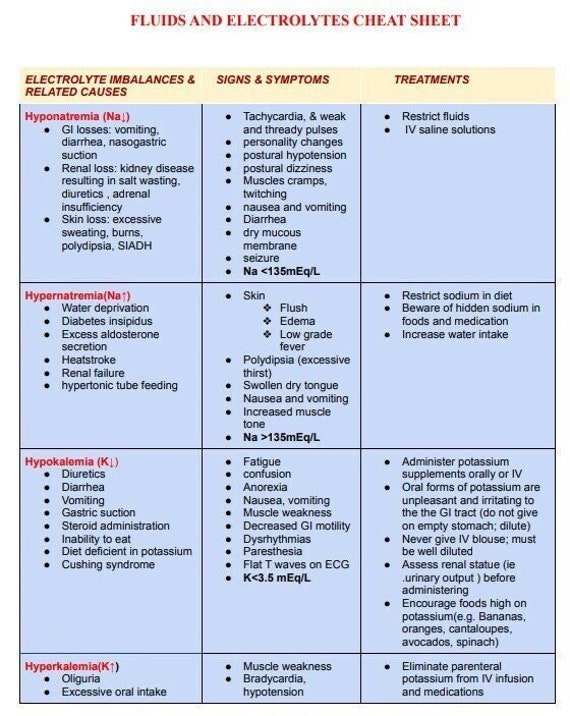
Fluid and electrolyte imbalances can stem from a variety of underlying conditions. Conditions like vomiting, diarrhea, excessive sweating, kidney disease, heart failure, and certain medications can all throw off the body's delicate balance.
The consequences of these imbalances are far-reaching. Dehydration, a common fluid deficit, can lead to dizziness, fatigue, and even organ damage. Overhydration, on the other hand, can cause swelling, shortness of breath, and heart problems.
Electrolyte imbalances can be equally serious. For example, low potassium levels (hypokalemia) can disrupt heart rhythm, while high potassium levels (hyperkalemia) can lead to cardiac arrest.
The Nurse's Perspective: Assessment is Key
Nurses play a pivotal role in identifying and managing fluid and electrolyte imbalances. Their assessments are crucial for early detection and intervention.
A thorough assessment includes a comprehensive review of the patient's medical history, current medications, and any symptoms they are experiencing. Accurate intake and output monitoring are also essential.
Physical examination findings, such as skin turgor (elasticity of the skin), mucous membrane moisture, and presence of edema (swelling), provide valuable clues. Additionally, laboratory tests, including serum electrolyte levels, blood urea nitrogen (BUN), creatinine, and urine specific gravity, help confirm the diagnosis and determine the severity of the imbalance.
Crafting the Care Plan: A Personalized Approach
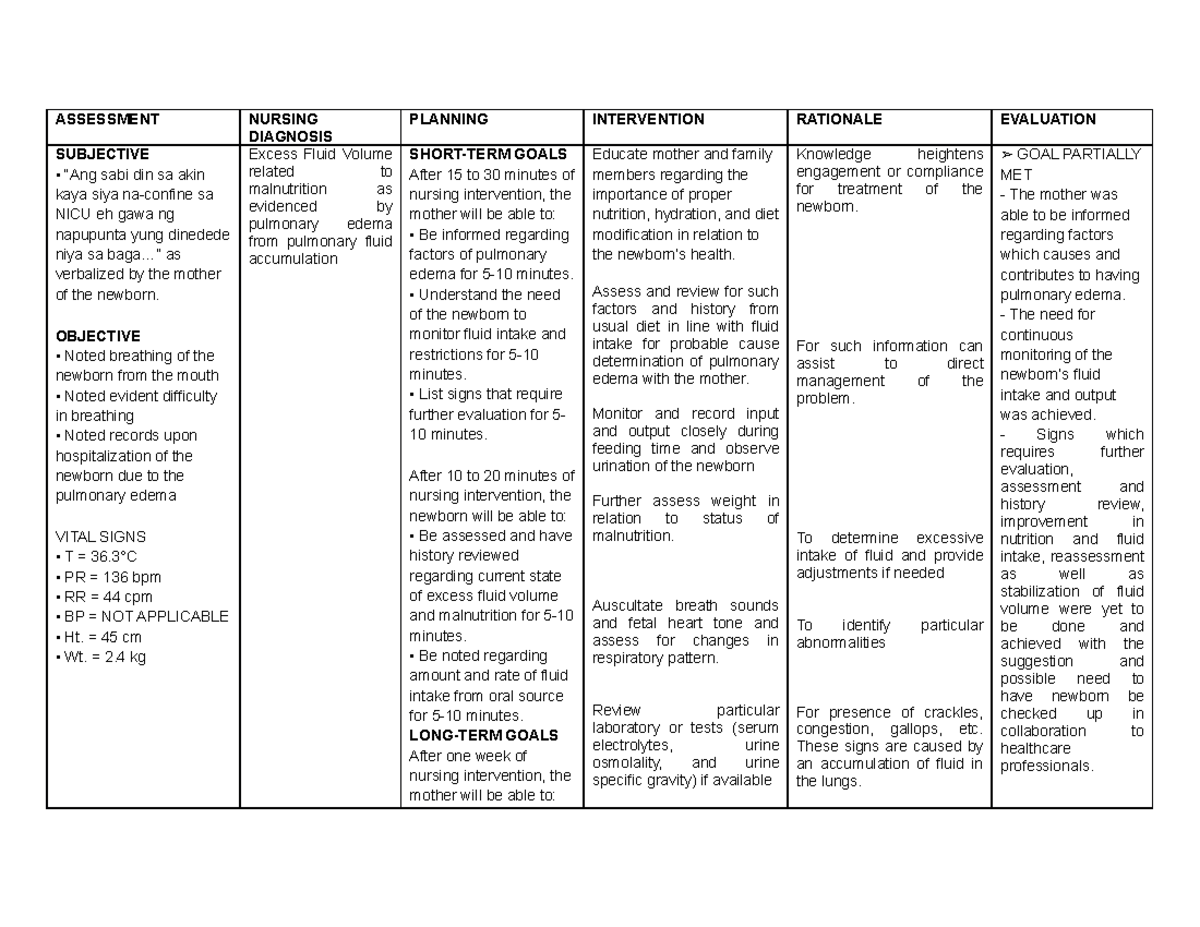
Once a fluid and electrolyte imbalance is identified, nurses develop individualized care plans to address the specific needs of each patient. These plans are based on nursing diagnoses, which are clinical judgments about the patient's response to actual or potential health problems.
For example, a patient with dehydration due to diarrhea might have the nursing diagnosis of "Deficient Fluid Volume related to excessive fluid loss as evidenced by decreased urine output and dry mucous membranes." The care plan would then outline specific interventions to address this problem.
Interventions: Restoring Balance and Preventing Complications
Nursing interventions for fluid and electrolyte imbalances are multifaceted and tailored to the underlying cause and the severity of the imbalance. Some common interventions include:
- Fluid Replacement: Administering oral or intravenous fluids to correct dehydration. The type and rate of fluid administration are carefully determined based on the patient's condition.
- Electrolyte Replacement: Supplementing electrolytes, such as potassium or magnesium, through oral or intravenous routes. Careful monitoring of electrolyte levels is crucial to prevent overcorrection.
- Dietary Modifications: Recommending dietary changes to promote fluid and electrolyte balance. For example, patients with sodium imbalances may need to restrict or increase their sodium intake.
- Medication Management: Administering medications to address the underlying cause of the imbalance, such as anti-diarrheals for diarrhea or diuretics for fluid overload.
- Monitoring Vital Signs: Closely monitoring vital signs, such as heart rate, blood pressure, and respiratory rate, to detect any signs of complications.
- Patient Education: Educating patients and their families about the importance of fluid and electrolyte balance, the signs and symptoms of imbalances, and how to prevent them.
The Importance of Monitoring and Evaluation
The nursing care plan is not a static document. It is continuously monitored and evaluated to ensure its effectiveness. Nurses regularly assess the patient's response to interventions and make adjustments as needed.
Monitoring includes tracking fluid intake and output, monitoring electrolyte levels, and assessing for any signs of complications. If the patient's condition does not improve as expected, the care plan may need to be revised.
Real-World Examples: Putting the Care Plan into Action
Let's consider a few examples of how nursing care plans are implemented in practice. Mrs. Johnson, an elderly woman with heart failure, is admitted to the hospital with fluid overload. Her nursing diagnosis is "Excess Fluid Volume related to impaired cardiac function as evidenced by edema and shortness of breath."
The care plan includes administering diuretics to promote fluid excretion, restricting sodium intake, monitoring fluid intake and output, and elevating her legs to reduce edema. The nurse also educates Mrs. Johnson about the importance of following a low-sodium diet and monitoring her weight daily.
Another example is Mr. Davis, a young athlete who is dehydrated after a marathon. His nursing diagnosis is "Deficient Fluid Volume related to excessive fluid loss as evidenced by thirst, dizziness, and decreased urine output." The care plan includes administering oral and intravenous fluids, monitoring electrolyte levels, and educating him about the importance of proper hydration during exercise.
The Bigger Picture: Prevention and Education
While effective nursing care is crucial for managing existing imbalances, prevention is always the best approach. Educating patients and communities about healthy lifestyle choices, such as maintaining adequate hydration and consuming a balanced diet, can significantly reduce the risk of fluid and electrolyte imbalances.
For example, individuals at high risk, such as elderly adults and athletes, may benefit from specific guidance on fluid intake and electrolyte replacement. Public health campaigns can also raise awareness about the importance of preventing dehydration during hot weather or strenuous activity.
Looking Ahead: Advancements in Nursing Care
The field of fluid and electrolyte management is constantly evolving. New research and technologies are leading to advancements in nursing care.
For example, continuous electrolyte monitoring devices are becoming increasingly available, allowing for more precise and timely interventions. Telehealth and remote monitoring technologies are also being used to manage fluid and electrolyte balance in patients at home.
As healthcare continues to advance, nurses will continue to play a critical role in ensuring optimal fluid and electrolyte balance for all patients. The dedication, expertise, and personalized care provided by nurses are essential for preventing complications and promoting overall health and well-being.
A Final Thought: The Power of Balance
Maintaining fluid and electrolyte balance is a fundamental aspect of health. While the intricacies of this process may seem complex, the underlying principle is simple: our bodies thrive on equilibrium.
Nurses, with their keen assessment skills, thoughtful care planning, and unwavering commitment to patient well-being, are the guardians of this balance. Their work ensures that our bodies have the necessary building blocks to function optimally, allowing us to live healthier, more vibrant lives. The impact of their efforts ripples far beyond the bedside, contributing to the overall health and well-being of individuals and communities.