How Many Days Into Placebo Pills Does Period Start

For many women on the combined oral contraceptive pill, the arrival of their period during the placebo week is a familiar monthly event. However, the exact timing of this withdrawal bleed can vary, leading to questions and sometimes anxiety. Understanding the factors that influence when a period starts during the placebo pill phase can empower women to better manage their expectations and reproductive health.
The timing of the withdrawal bleed during the placebo week is a common concern for women taking combined oral contraceptives. It's important to understand the typical timeframe, the influencing factors, and when to seek medical advice. This article will delve into the specifics of how many days into the placebo pills a period usually starts, providing evidence-based information to help readers navigate this aspect of hormonal contraception.
Typical Timing of Withdrawal Bleeding
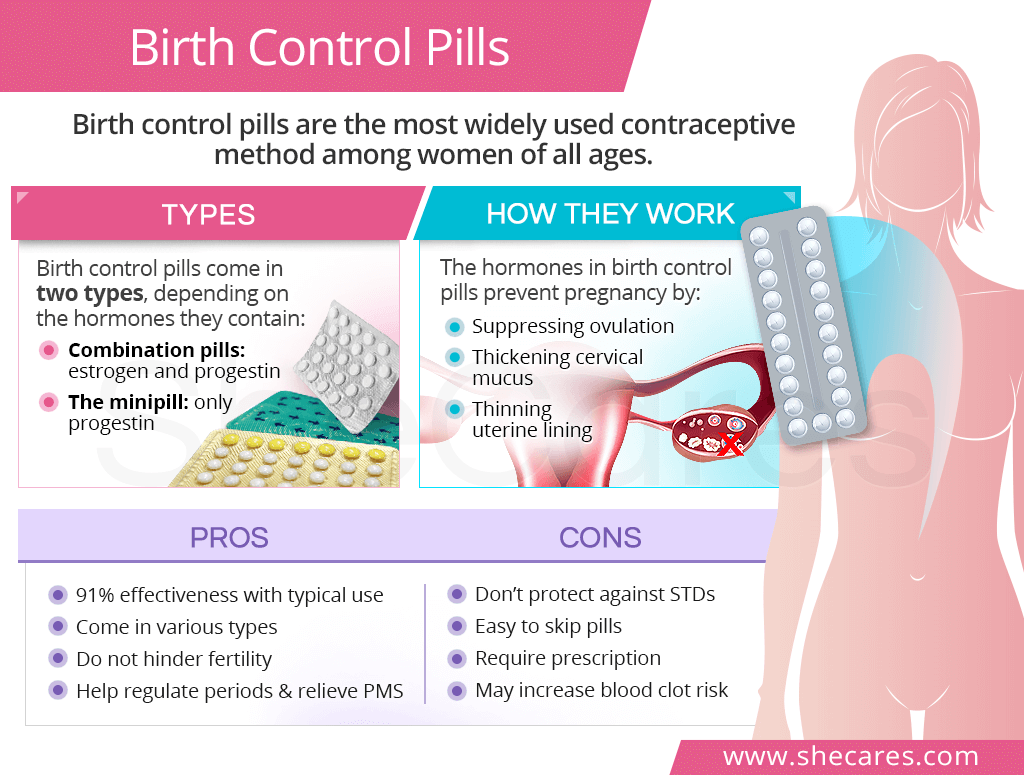
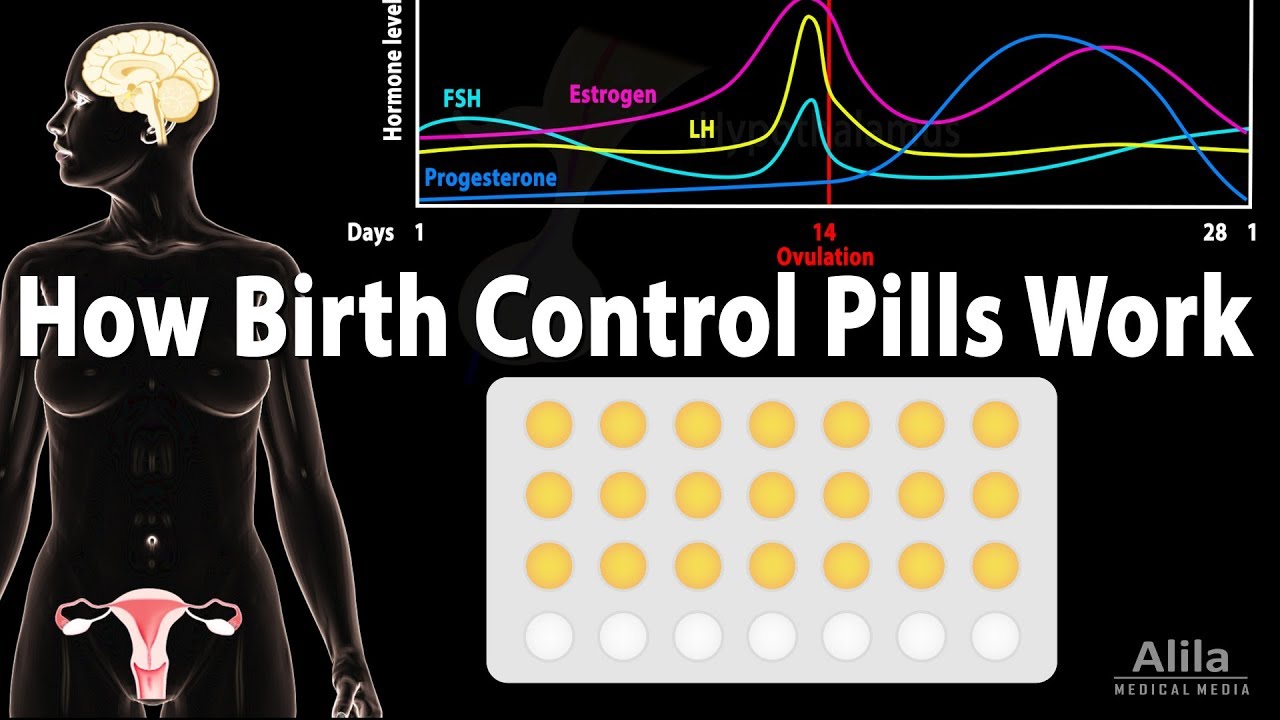
The "period" experienced during the placebo week isn't a true menstrual period, but rather a withdrawal bleed. This bleeding occurs because the drop in hormones (estrogen and progestin) triggers the shedding of the uterine lining. Generally, the withdrawal bleed starts within two to four days after taking the last active pill.
This timeframe isn't set in stone, and variations are normal. Some women might experience bleeding sooner, while others might not see any bleeding until the very end of the placebo week or even not at all. A study published in the European Journal of Contraception and Reproductive Health Care highlighted that the timing can be influenced by several factors.
Factors Influencing Bleeding Onset
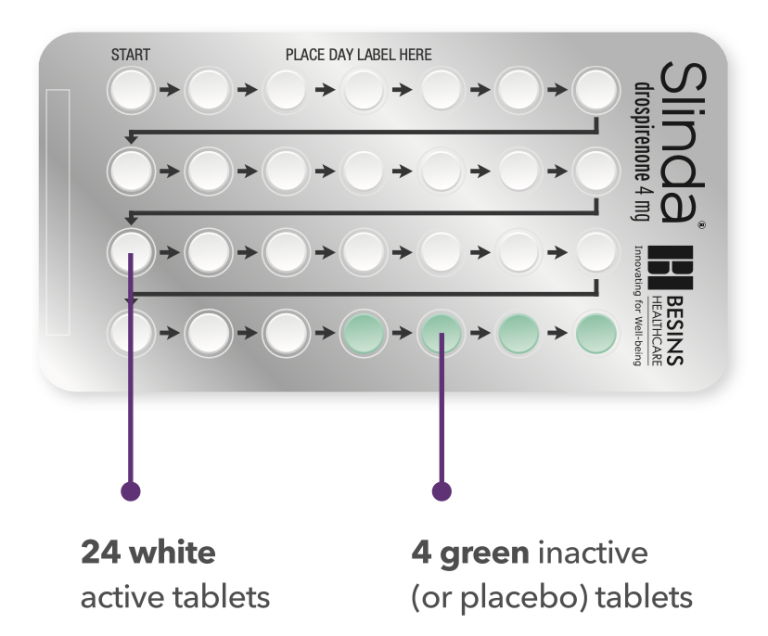
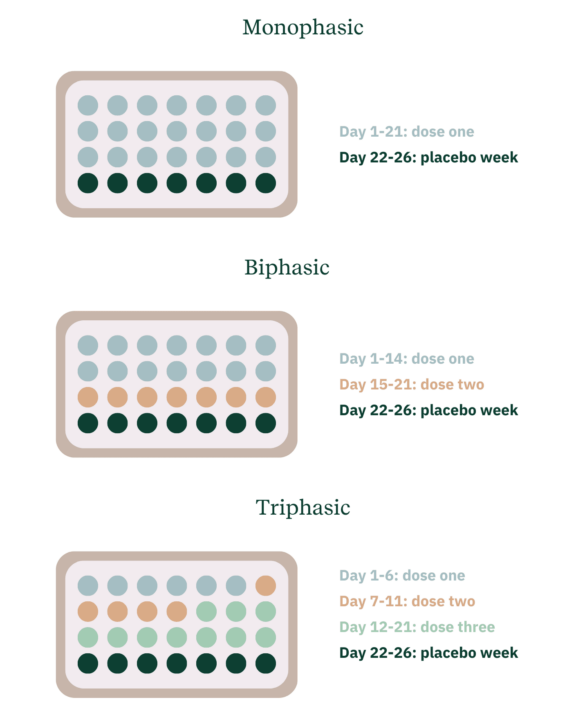
Several factors can influence when a withdrawal bleed begins. The type of birth control pill is a key factor. Monophasic pills, which deliver the same dose of hormones each day, tend to produce more predictable bleeding patterns compared to multiphasic pills where the hormone dosages fluctuate.
Adherence to the pill schedule also plays a crucial role. Inconsistent pill-taking, especially missing pills, can disrupt hormone levels and lead to earlier or irregular bleeding. Additionally, individual differences in metabolism and sensitivity to hormones can affect the timing and intensity of the withdrawal bleed.
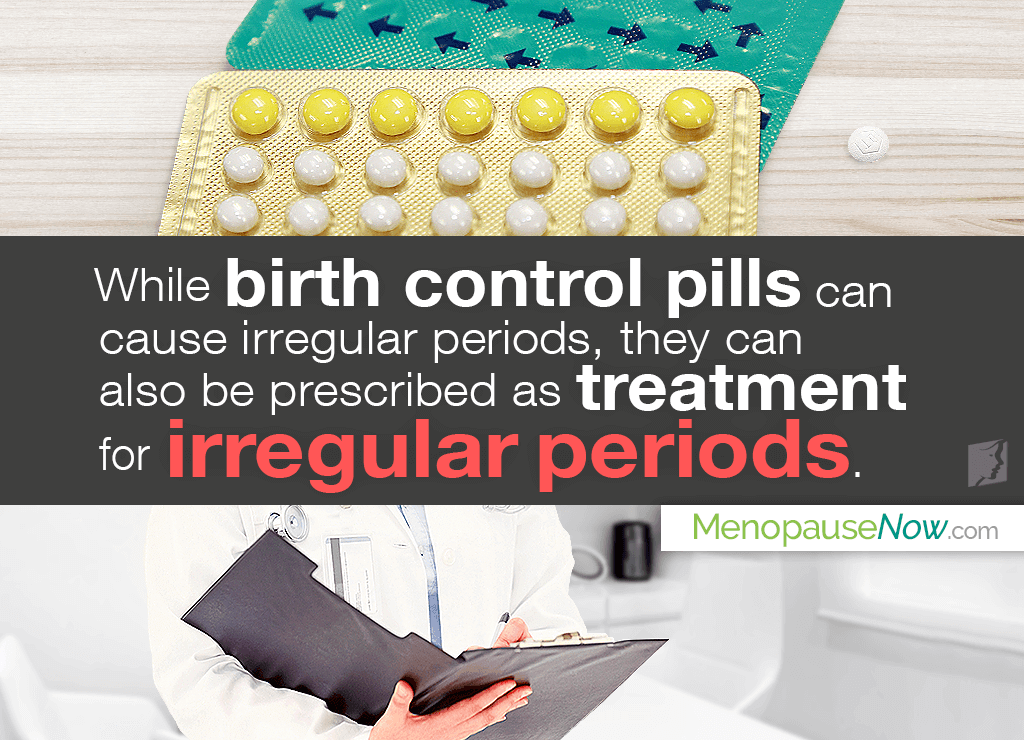
Other medications and supplements can also interfere with the pill's effectiveness and impact bleeding patterns. Conditions like Polycystic Ovary Syndrome (PCOS) can also have an impact on irregular bleeding regardless if someone is on birth control or not.
When to Consult a Healthcare Provider
While variations in the timing of withdrawal bleeding are usually normal, there are situations when consulting a healthcare provider is recommended. If you consistently experience bleeding outside of the placebo week, it could indicate breakthrough bleeding, which might require a change in pill formulation. Similarly, if you consistently miss periods during the placebo week, it is crucial to rule out pregnancy or other underlying medical conditions.
According to the American College of Obstetricians and Gynecologists (ACOG), if you miss two or more periods in a row while on the pill, you should take a pregnancy test. It’s also important to consult with a doctor if you experience heavy or prolonged bleeding, severe pain, or any other unusual symptoms during the placebo week.
Managing Expectations and Reducing Anxiety
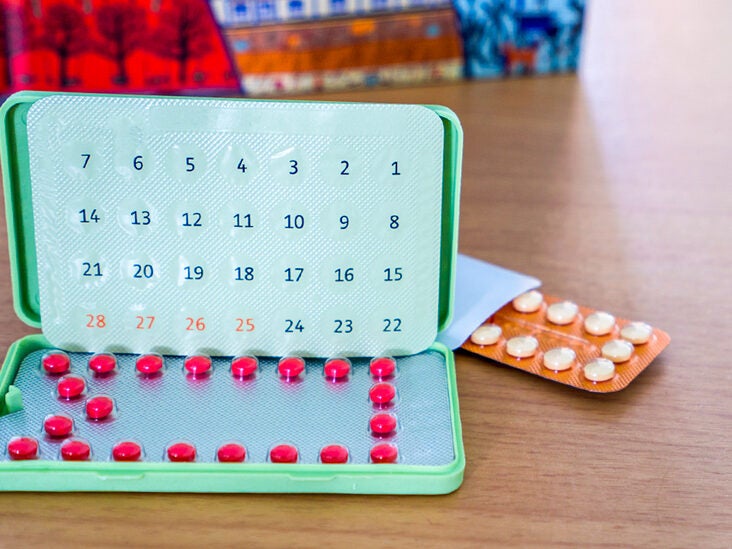
Understanding that the timing of withdrawal bleeding can vary and is not always perfectly predictable is key to managing expectations and reducing anxiety. Keeping a menstrual diary or using a period tracking app can help monitor bleeding patterns and identify any significant changes.
If you are concerned about the timing or intensity of your withdrawal bleed, discussing your concerns with your healthcare provider is the best course of action. They can provide personalized advice based on your individual medical history and the specific type of birth control pill you are taking. Remember, knowledge is power when it comes to managing your reproductive health.
The Evolution of Pill Formulations and Bleeding Patterns
The development of oral contraceptives has continually evolved, with newer formulations aiming to minimize side effects and optimize bleeding patterns. Some pills are designed for extended cycles, allowing women to have fewer periods per year. Others are low-dose pills that may result in lighter or less frequent bleeding.
It’s essential to discuss your preferences and concerns about bleeding patterns with your doctor when choosing a birth control pill. They can help you select a formulation that aligns with your individual needs and lifestyle. The key is open communication and informed decision-making.
Ultimately, understanding the nuances of withdrawal bleeding during the placebo week empowers women to take control of their reproductive health. Staying informed, tracking your cycle, and consulting with a healthcare provider when needed are crucial steps towards a more confident and comfortable experience with hormonal contraception.






:max_bytes(150000):strip_icc()/GettyImages-1297131187-75714278ff3f497bbc386276e195e484.jpg)