Immunotherapy Success Rate Head And Neck Cancer
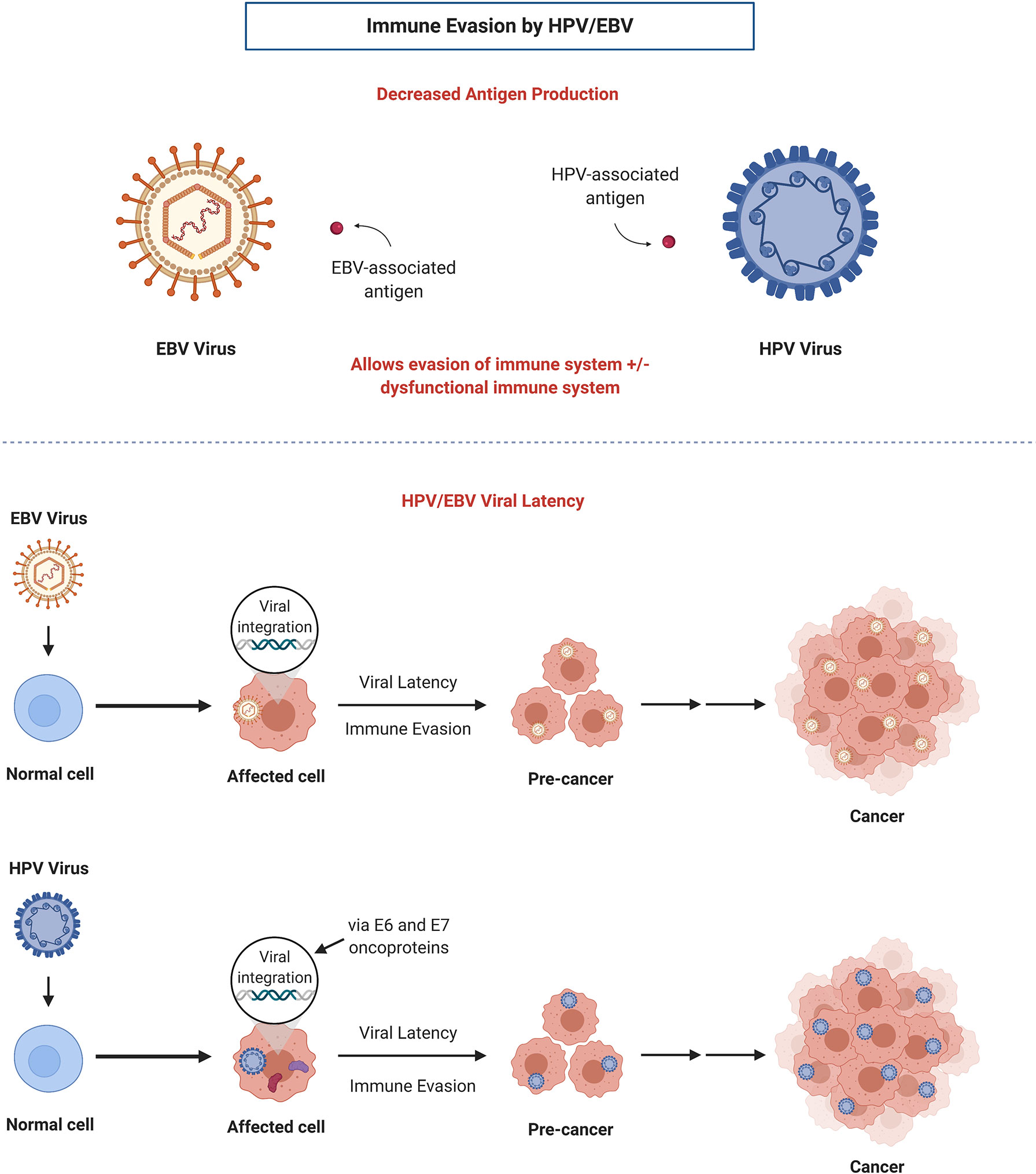
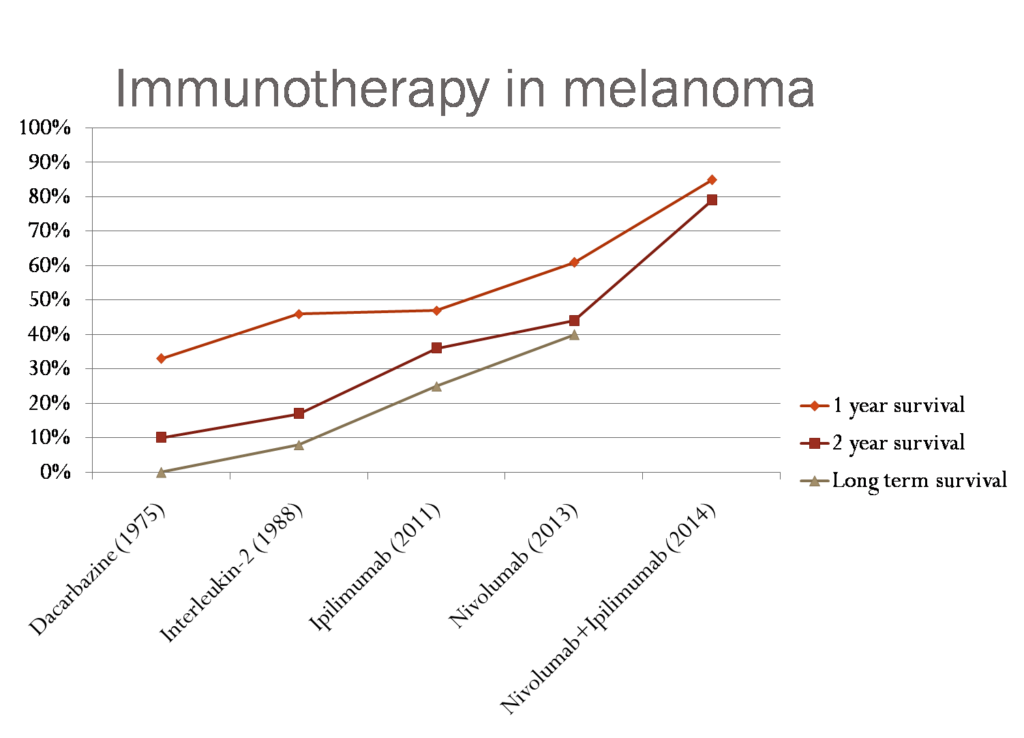
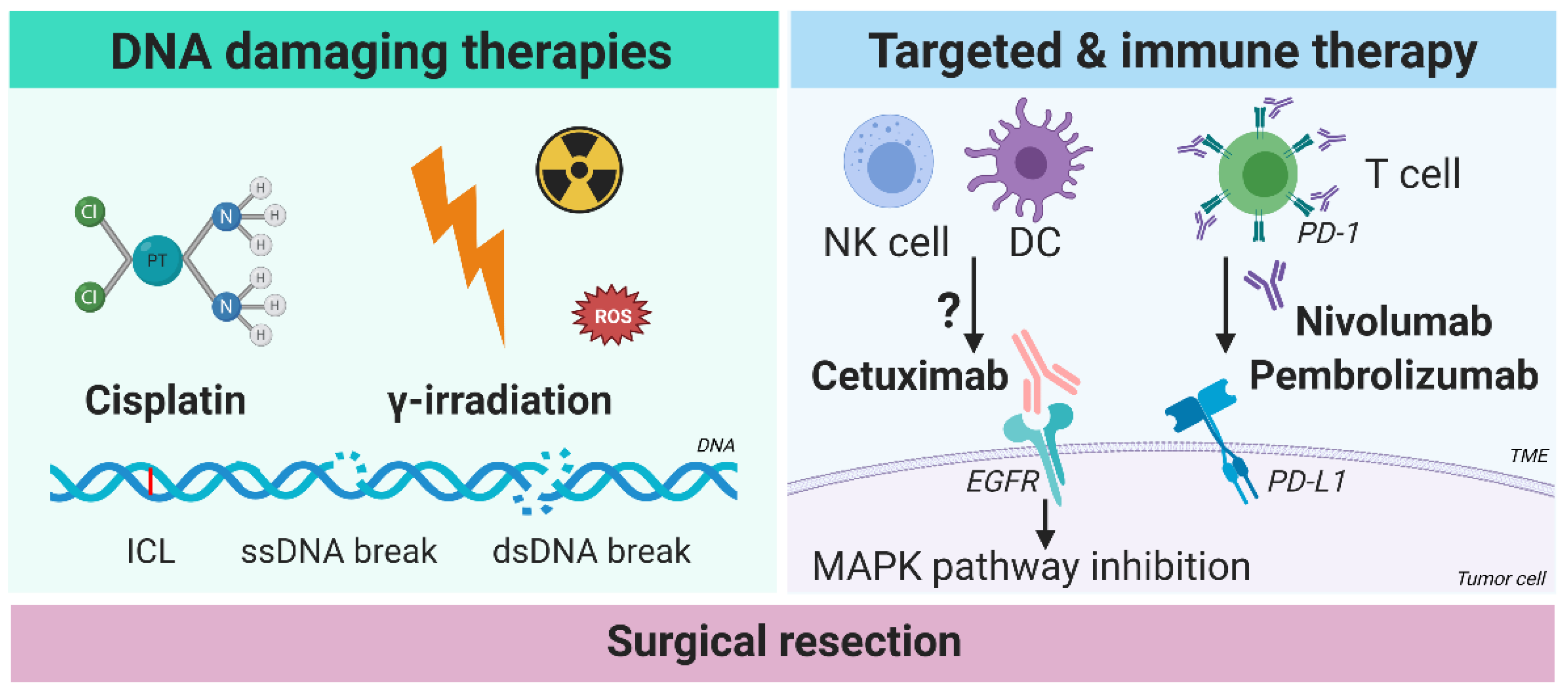
The relentless battle against head and neck cancers is witnessing a surge of hope, fueled by encouraging advancements in immunotherapy. For decades, treatment options remained largely confined to surgery, radiation, and chemotherapy, each fraught with debilitating side effects and often limited success, particularly in recurrent or metastatic cases. Now, a new wave of immunotherapy approaches is rewriting the narrative, offering extended survival and improved quality of life for a growing subset of patients.
This article delves into the emerging role of immunotherapy in head and neck cancer treatment, exploring recent clinical trial data, the mechanisms behind its effectiveness, the challenges that remain, and the promising future directions of research in this dynamic field. The data reveals a marked improvement in outcomes for certain patient populations, offering a much-needed alternative to traditional therapies and sparking a revolution in how these complex cancers are managed.
Immunotherapy: A New Frontier in Head and Neck Cancer Treatment
Immunotherapy harnesses the power of the body's own immune system to fight cancer. Unlike chemotherapy, which directly targets cancer cells but often harms healthy cells in the process, immunotherapy aims to stimulate the immune system to recognize and destroy cancer cells specifically.
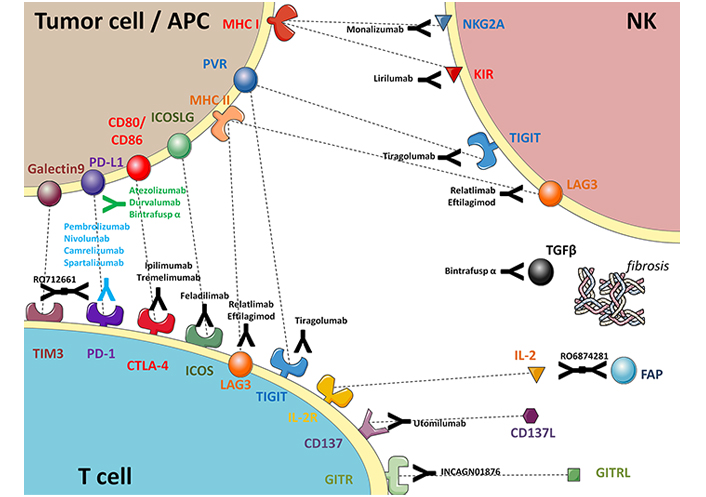
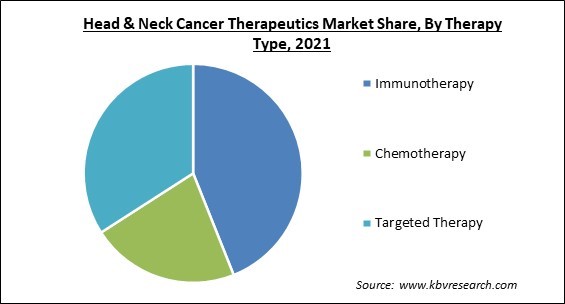
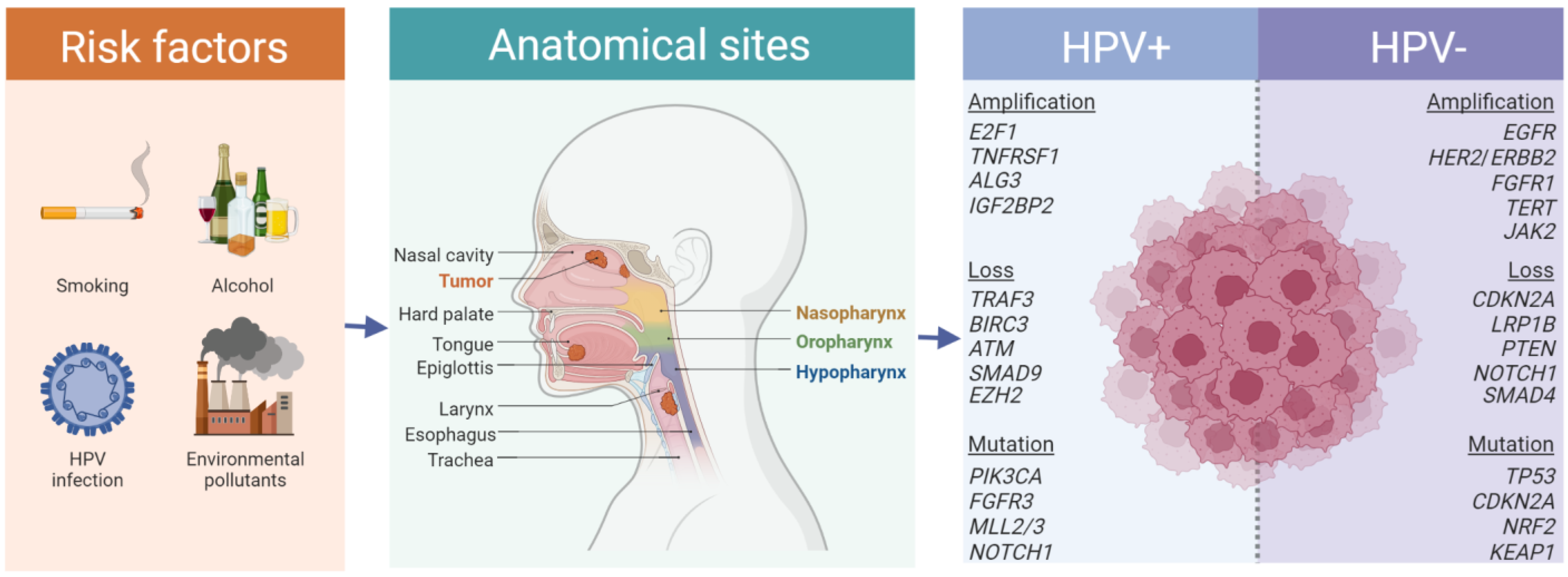
The two primary immunotherapy strategies currently used in head and neck cancer treatment are checkpoint inhibitors and, to a lesser extent, adoptive cell therapies. Checkpoint inhibitors work by blocking proteins that prevent immune cells from attacking cancer cells, effectively releasing the brakes on the immune system.
The Rise of Checkpoint Inhibitors
Checkpoint inhibitors targeting the PD-1 and PD-L1 pathways have become the cornerstone of immunotherapy in head and neck cancer. Keytruda (pembrolizumab) and Opdivo (nivolumab) are two prominent examples of these drugs that have demonstrated significant clinical benefit.
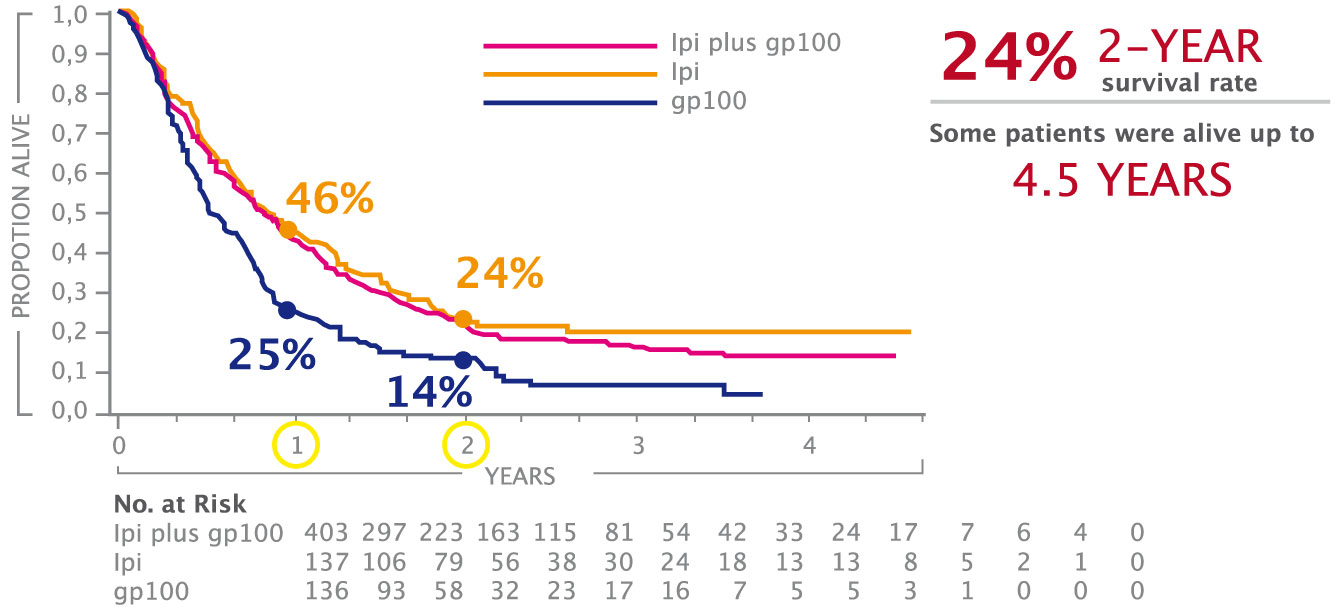
Clinical trials, such as the KEYNOTE-048 and CheckMate 141 studies, have shown that these agents can significantly improve overall survival in patients with recurrent or metastatic head and neck squamous cell carcinoma (HNSCC), especially those with high PD-L1 expression.
"The impact of checkpoint inhibitors has been transformative," says Dr. Eleanor Higgins, an oncologist specializing in head and neck cancers at the University of California, San Francisco. "We are seeing patients who would have had very limited options just a few years ago now living longer and with a better quality of life."
"Immunotherapy has fundamentally changed the treatment paradigm for advanced head and neck cancer. It offers a chance at durable responses that we rarely saw with traditional chemotherapy regimens." - Dr. David Lee, Head of Oncology, Massachusetts General Hospital.
Understanding the Success Rates
While the overall survival benefits of immunotherapy are encouraging, it's important to acknowledge that not all patients respond equally. The success rate of immunotherapy in head and neck cancer varies depending on factors such as PD-L1 expression, tumor mutational burden (TMB), and the patient's overall health.
Studies have shown that patients with high PD-L1 expression (defined as a PD-L1 combined positive score [CPS] of 1 or higher) are more likely to respond to pembrolizumab as a first-line treatment. However, even patients with low PD-L1 expression can still benefit from immunotherapy, especially when combined with chemotherapy.
The KEYNOTE-048 trial demonstrated that pembrolizumab plus chemotherapy significantly improved overall survival compared to chemotherapy alone, regardless of PD-L1 expression. This suggests that a combination approach may be beneficial for a wider range of patients.
Challenges and Limitations
Despite the promising results, immunotherapy is not without its challenges. One of the main concerns is the development of immune-related adverse events (irAEs), which can affect various organs and systems in the body.
These irAEs can range from mild skin rashes to more severe complications such as pneumonitis, colitis, and endocrinopathies. Careful monitoring and prompt management are crucial to minimizing the impact of these side effects.
Another limitation is the lack of reliable biomarkers to predict which patients are most likely to respond to immunotherapy. While PD-L1 expression is currently the most widely used biomarker, it is not perfect, and other factors may also play a role.
Future Directions and Research
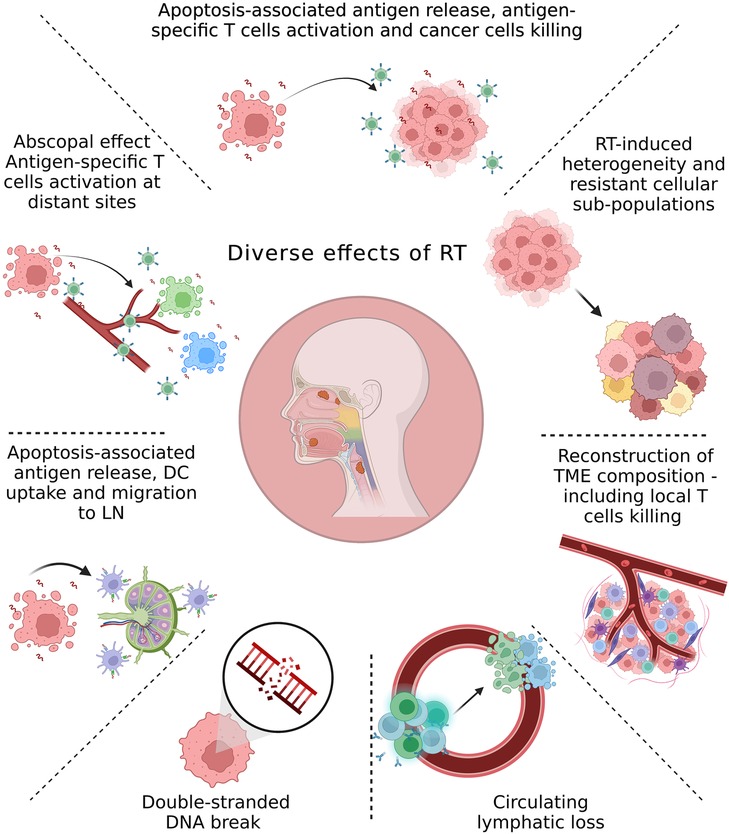
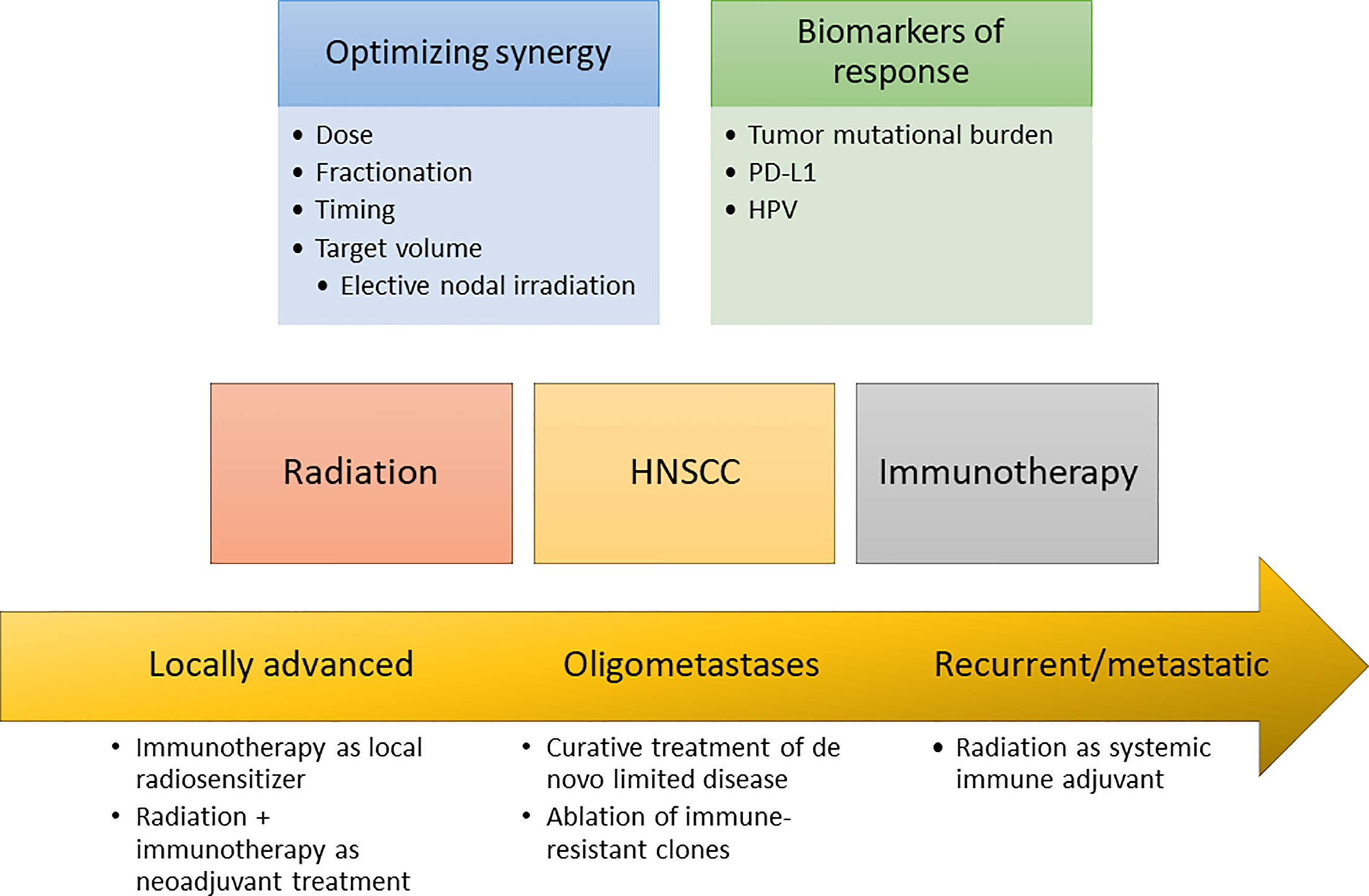
Research in head and neck cancer immunotherapy is rapidly evolving, with a focus on developing new and improved strategies to enhance its effectiveness. One promising area is the development of combination therapies that combine immunotherapy with other treatments, such as radiation therapy, targeted therapy, and even other immunotherapeutic agents.
Clinical trials are also exploring the use of adoptive cell therapies, such as CAR-T cell therapy, in head and neck cancer. This approach involves engineering a patient's own immune cells to specifically target cancer cells.
"We are exploring novel combinations and strategies to overcome resistance to immunotherapy," explains Dr. James Carter, a leading researcher in head and neck cancer immunotherapy at Johns Hopkins University. "The goal is to make immunotherapy work for more patients and to improve the durability of responses."
Furthermore, research is focused on identifying new biomarkers that can better predict response to immunotherapy and help personalize treatment decisions. This includes exploring the role of the tumor microenvironment, the gut microbiome, and other factors that may influence the immune response.
Hope for the Future
Immunotherapy represents a significant advance in the treatment of head and neck cancer, offering hope to patients who previously had limited options. While challenges remain, ongoing research and clinical trials are paving the way for even more effective and personalized immunotherapy approaches.
The future of head and neck cancer treatment is likely to involve a combination of immunotherapy and other therapies, tailored to the individual characteristics of each patient's cancer. This personalized approach holds the promise of improving outcomes and enhancing the quality of life for those affected by this challenging disease.
The ongoing development and refinement of immunotherapeutic strategies offers a powerful tool in the fight against head and neck cancers, signaling a new era of optimism and progress in oncology.