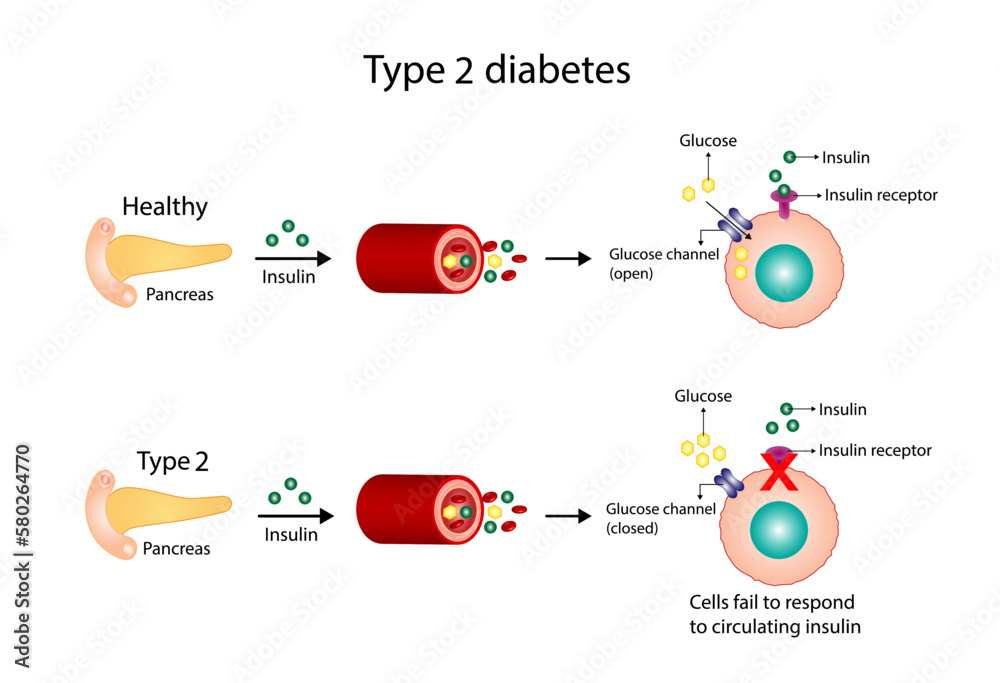
In Diabetes Target Cells Do Not Respond Normally To Insulin

Urgent reports confirm a fundamental flaw in diabetes: target cells, responsible for regulating blood sugar, exhibit impaired response to insulin, the hormone crucial for glucose uptake.
This resistance at the cellular level undermines the body's ability to effectively utilize insulin, leading to elevated blood sugar levels and the cascade of complications associated with diabetes.
Cellular Resistance: The Core of the Crisis
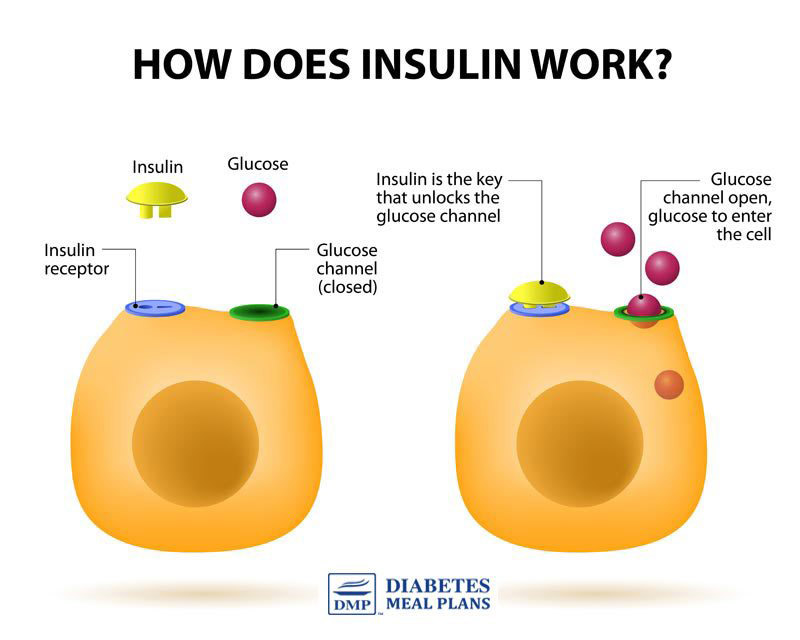
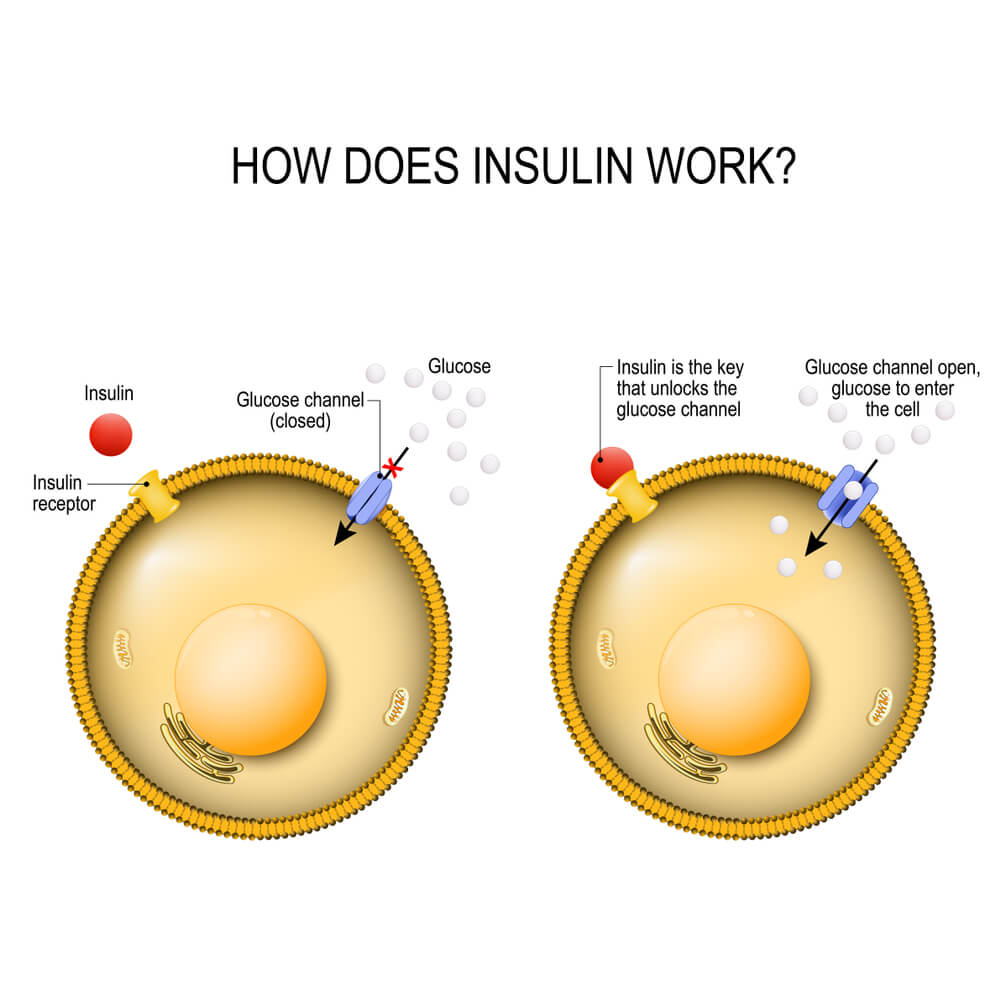
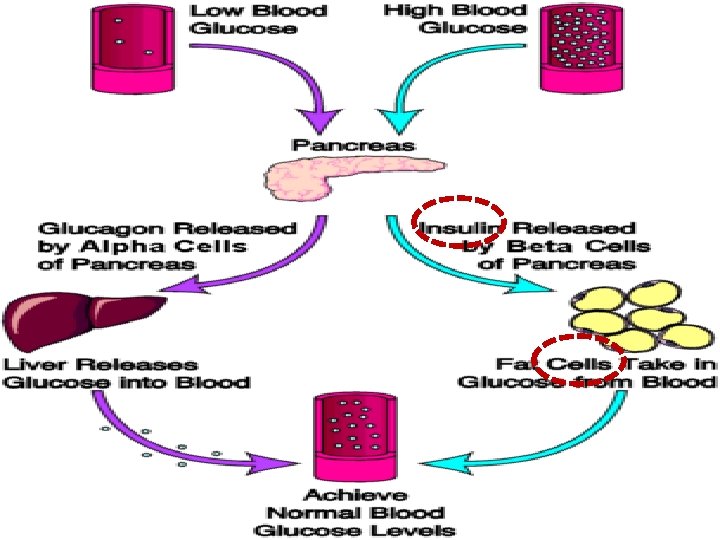
At the heart of diabetes lies insulin resistance. This means cells in the muscles, liver, and fat tissues do not respond adequately to insulin's signal to absorb glucose from the bloodstream.
Instead of opening their "doors" to glucose when insulin arrives, these cells remain largely closed, forcing glucose to accumulate in the blood.
This resistance triggers a vicious cycle, pushing the pancreas to produce even more insulin in an attempt to overcome the cellular blockade.
Who is Affected?
Millions worldwide are affected. According to the World Health Organization (WHO), an estimated 422 million adults globally were living with diabetes in 2014.
The Centers for Disease Control and Prevention (CDC) reports that in the United States, 37.3 million adults have diabetes, and alarmingly, 1 in 5 don't know they have it.
This resistance manifests differently in individuals, influenced by factors like genetics, lifestyle, and underlying health conditions.
What Happens When Cells Resist?
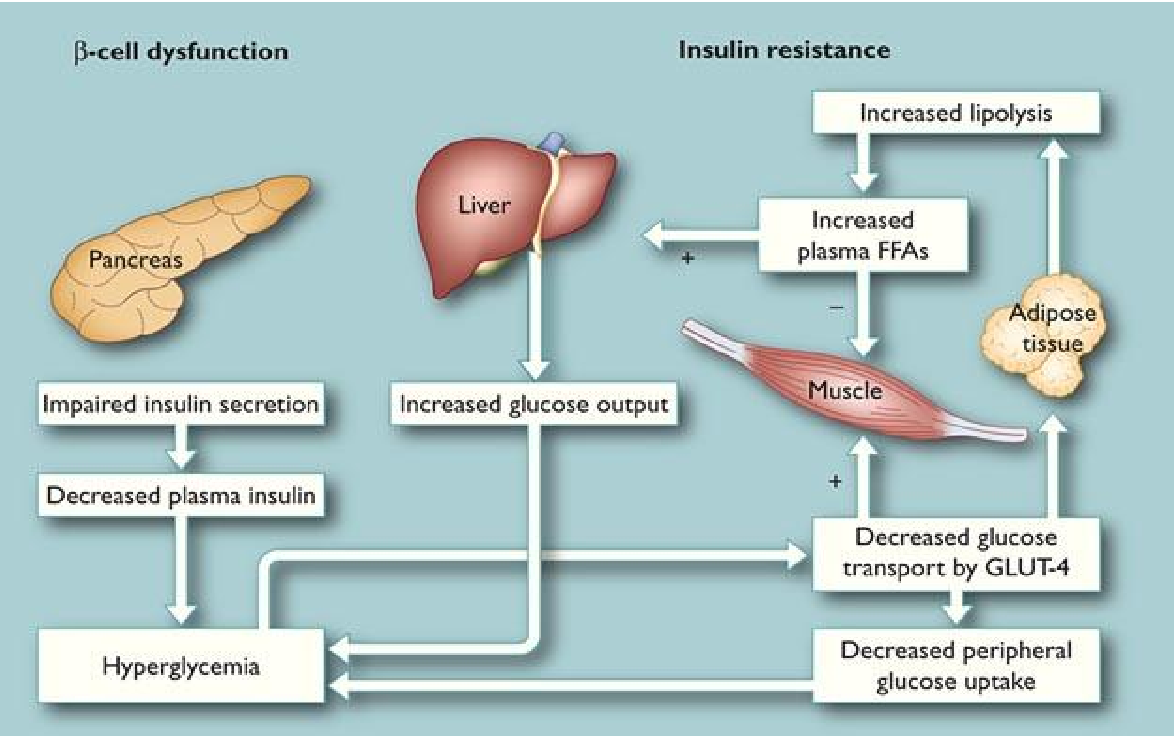
Insulin resistance disrupts the delicate balance of glucose metabolism. The excess glucose circulating in the blood, termed hyperglycemia, wreaks havoc on the body.
Over time, this persistent high blood sugar damages blood vessels, nerves, and organs.
This cellular dysfunction contributes to the development of serious complications, including heart disease, kidney disease, nerve damage (neuropathy), and vision loss (retinopathy).
Where Does This Resistance Occur?
The primary sites of insulin resistance are the muscles, liver, and adipose tissue (fat). These tissues are crucial for glucose uptake and storage.
Muscle cells, responsible for utilizing glucose for energy, become less responsive to insulin's signal to take up glucose.
The liver, which normally regulates glucose production, may continue to produce excess glucose even when blood sugar levels are already high.
When Does This Resistance Develop?
Insulin resistance often develops gradually over time. It's often linked to lifestyle factors like obesity, physical inactivity, and a diet high in processed foods and sugars.
Prediabetes, a condition characterized by higher-than-normal blood sugar levels, is often a precursor to type 2 diabetes and a sign that insulin resistance is already present.
The onset can also be influenced by genetic predisposition and certain medical conditions, such as polycystic ovary syndrome (PCOS).
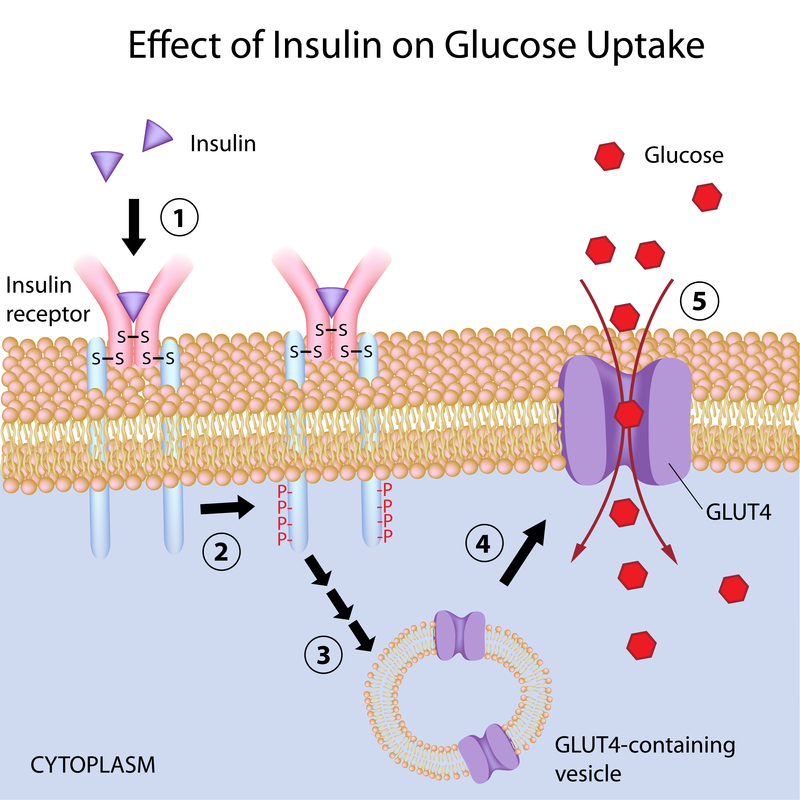
How Does Insulin Resistance Work at the Molecular Level?
The exact mechanisms behind insulin resistance are complex and still being actively researched. It involves a cascade of molecular events within the cell.
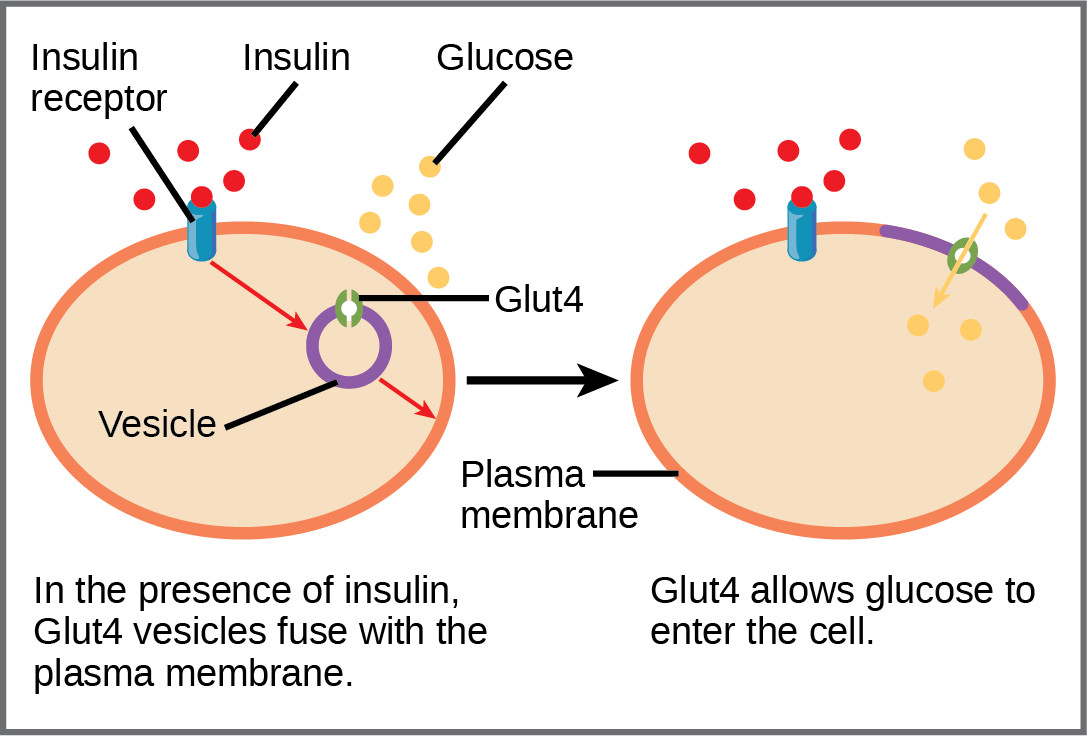
One key factor is impaired insulin signaling. Insulin binds to receptors on the cell surface, triggering a series of intracellular signals that ultimately lead to glucose transporters moving to the cell membrane.
In insulin-resistant cells, these signaling pathways are disrupted, preventing the efficient translocation of glucose transporters and hindering glucose uptake.
The Fight Against Resistance: Current Strategies
Managing insulin resistance is crucial for preventing and controlling diabetes.
Lifestyle modifications, including diet and exercise, remain the cornerstone of treatment. A healthy diet, low in processed foods and saturated fats, can improve insulin sensitivity.
Regular physical activity helps the body utilize glucose more effectively and improve insulin sensitivity.
Medications to Enhance Insulin Sensitivity
Several medications are available to improve insulin sensitivity and lower blood sugar levels. Metformin, a commonly prescribed drug, works primarily by reducing glucose production in the liver and improving insulin sensitivity in muscle tissue.
Thiazolidinediones (TZDs) are another class of drugs that enhance insulin sensitivity in muscle and fat tissue.
These medications are often used in combination with lifestyle modifications to achieve optimal blood sugar control.
Looking Ahead: Future Research and Developments
Research continues to delve deeper into the molecular mechanisms underlying insulin resistance.
Scientists are exploring novel therapeutic targets that could improve insulin sensitivity and prevent the development of diabetes complications.
Ongoing studies are investigating the role of genetics, inflammation, and gut microbiota in the development of insulin resistance.
The urgent need for effective interventions is clear. Addressing insulin resistance is paramount to curbing the global diabetes epidemic and improving the health of millions worldwide.