Medical Ethics Accounts Of Ground Breaking Cases

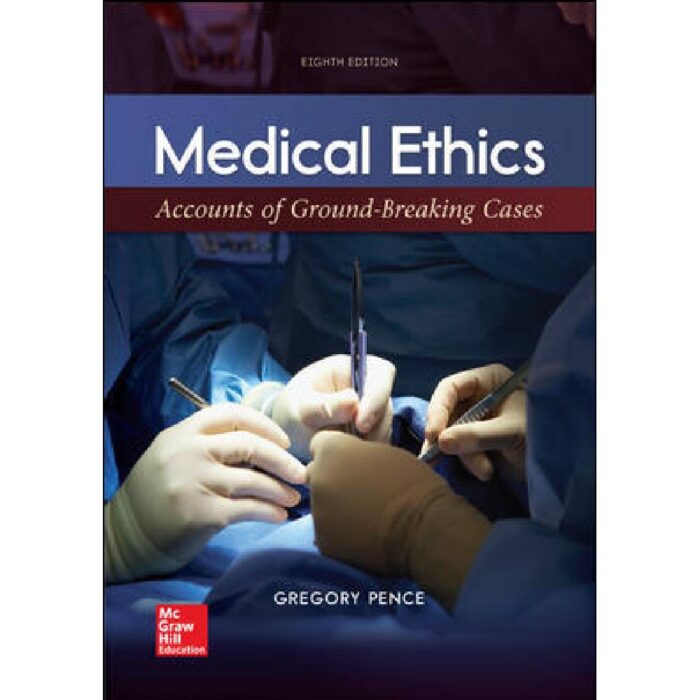
The operating room hummed with sterile efficiency, a battleground where science confronted the very definition of life and death. In the annals of medicine, certain cases stand as stark reminders of the ethical tightrope walked by practitioners. These landmark events, fraught with moral complexities, have not only shaped medical protocols but have also ignited public discourse, forcing society to confront its values and biases.
This article delves into the ethically challenging stories behind groundbreaking medical cases that have profoundly impacted the field. We will explore the pivotal questions they raised, the agonizing decisions made, and the enduring legacies they have left on patient care, medical research, and legal frameworks. By examining these historical turning points, we gain a crucial understanding of the ongoing evolution of medical ethics and its indispensable role in safeguarding human dignity within the ever-advancing realm of healthcare.
The Case of Henrietta Lacks: A Legacy of Exploitation and Scientific Advancement
Henrietta Lacks, an African American woman who died of cervical cancer in 1951, unknowingly became a cornerstone of modern medicine. Her cells, dubbed HeLa cells, were harvested without her consent and have since been used in countless research projects. These cells have been instrumental in developing the polio vaccine, understanding cancer, and advancing gene mapping, making them an invaluable scientific resource.
However, the story of Henrietta Lacks is also a chilling account of exploitation and racial injustice. Neither she nor her family were informed about the use of her cells, and they received no compensation for the immense profits generated from their proliferation. This case sparked outrage and ignited a debate about informed consent, patient rights, and the ethical obligations of researchers.
The Lacks family has fought for recognition and control over Henrietta's legacy. Public acknowledgment of the ethical breaches surrounding the HeLa cells has grown over time, with institutions like the National Institutes of Health (NIH) establishing guidelines for researchers using the cells. The Henrietta Lacks Enhancing Cancer Research Act, signed into law in 2023, further protects patient privacy in research. Still, the question remains: can scientific progress justify a violation of personal autonomy?
The Willowbrook Hepatitis Study: A Questionable Pursuit of Knowledge
From the mid-1950s to the 1970s, researchers at the Willowbrook State School, an institution for children with intellectual disabilities, conducted controversial hepatitis studies. New admissions were intentionally infected with hepatitis to track the disease's progression and test potential treatments. The justification, in part, was that the children would likely contract hepatitis anyway due to the unsanitary conditions at the overcrowded facility.
The Willowbrook study raised serious ethical concerns about informed consent, vulnerability, and the exploitation of a particularly susceptible population. Parents were often pressured to consent to their children's participation in the study as a condition of admission to the school. The children themselves were unable to provide informed consent, raising questions about the validity of parental consent in such circumstances.
The Willowbrook case became a watershed moment in the development of regulations governing research involving human subjects. The National Research Act of 1974, which mandated the establishment of Institutional Review Boards (IRBs) to review research proposals, was a direct response to the ethical lapses exposed by the Willowbrook study. This emphasized the necessity of protecting vulnerable populations and ensuring ethical research practices.
The First Heart Transplant: Defining Death and the Boundaries of Innovation
In December 1967, Dr. Christiaan Barnard performed the world's first human-to-human heart transplant in South Africa. While a technological marvel, the procedure ignited a firestorm of ethical debate. One of the central issues was the definition of death itself.
Prior to the transplant, the donor, Denise Darvall, was kept on a ventilator while her heart was still beating. The question arose: when is it ethical to remove organs from a person whose heart is still functioning, even if brain activity has ceased? The controversy surrounding the first heart transplant contributed to the development of brain death criteria, providing a more precise and ethically sound standard for organ donation.
Beyond the definition of death, the case also sparked discussions about resource allocation and the risks associated with experimental procedures. Critics questioned whether the resources invested in a single heart transplant could have been better used to benefit a larger number of patients. The success of Dr. Barnard's procedure fueled organ transplantation programs globally, yet the ethical questions surrounding informed consent, organ procurement, and equitable access continue to be debated.
The Oregon Death with Dignity Act: Autonomy and End-of-Life Care
In 1997, Oregon enacted the Death with Dignity Act, legalizing physician-assisted suicide for terminally ill patients. This landmark legislation ignited a national debate about patient autonomy, end-of-life care, and the role of physicians in assisting death. The Act allows competent adult residents with a terminal illness and a prognosis of six months or less to live to request a prescription for medication to end their life.
Proponents of the Death with Dignity Act argue that it empowers individuals to make autonomous decisions about their own bodies and to alleviate suffering in the face of terminal illness. They emphasize the importance of patient choice and the right to control one's own destiny. Opponents, however, raise concerns about the sanctity of life, the potential for abuse, and the slippery slope towards euthanasia.
The Oregon Death with Dignity Act has served as a model for similar legislation in other states, including Washington, Vermont, and California. The debate surrounding physician-assisted suicide highlights the complex ethical considerations involved in end-of-life care. It forces society to grapple with fundamental questions about the meaning of life, the nature of suffering, and the limits of medical intervention.
Looking Ahead: Navigating the Ethical Frontier
As medical technology continues to advance at an exponential pace, ethical dilemmas will only become more complex. Gene editing, artificial intelligence in healthcare, and personalized medicine present unprecedented opportunities and challenges. Maintaining a strong ethical compass is crucial to navigate this new frontier.
Open dialogue, ongoing education, and robust regulatory frameworks are essential to ensure that medical advancements are used responsibly and ethically. Protecting patient rights, promoting informed consent, and addressing disparities in access to care must remain at the forefront of medical ethics. Only through thoughtful consideration and unwavering commitment to ethical principles can we harness the full potential of medicine while safeguarding the dignity and well-being of all individuals.