Minimal Residual Disease In Acute Myeloid Leukemia

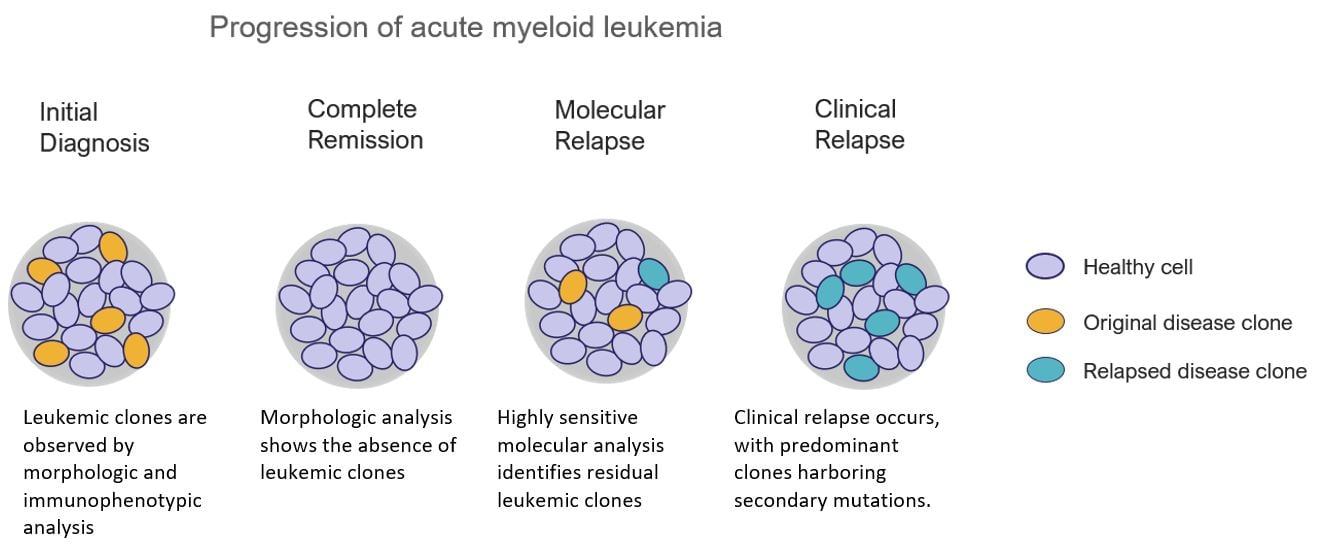
The specter of cancer recurrence looms large for patients battling acute myeloid leukemia (AML), a rapidly progressing cancer of the blood and bone marrow. Even after achieving seemingly successful remission through intensive chemotherapy or stem cell transplant, the disease can stealthily return. Now, a powerful tool is emerging to combat this threat: Minimal Residual Disease (MRD) testing, offering a deeper look into the leukemia's lingering presence.
At its core, MRD testing represents a paradigm shift in how we manage AML. This sophisticated technique detects even trace amounts of leukemia cells that remain in the body despite conventional treatment. By identifying patients at high risk of relapse, MRD monitoring allows for preemptive interventions, potentially improving long-term survival.
Understanding Minimal Residual Disease
MRD, sometimes referred to as measurable residual disease, signifies the presence of leukemia cells below the level of detection by standard methods like bone marrow biopsies. Traditionally, a bone marrow biopsy might indicate complete remission if no abnormal cells are visible under a microscope. MRD testing, however, can identify even one leukemia cell among millions of normal cells, providing a more granular assessment of treatment response.
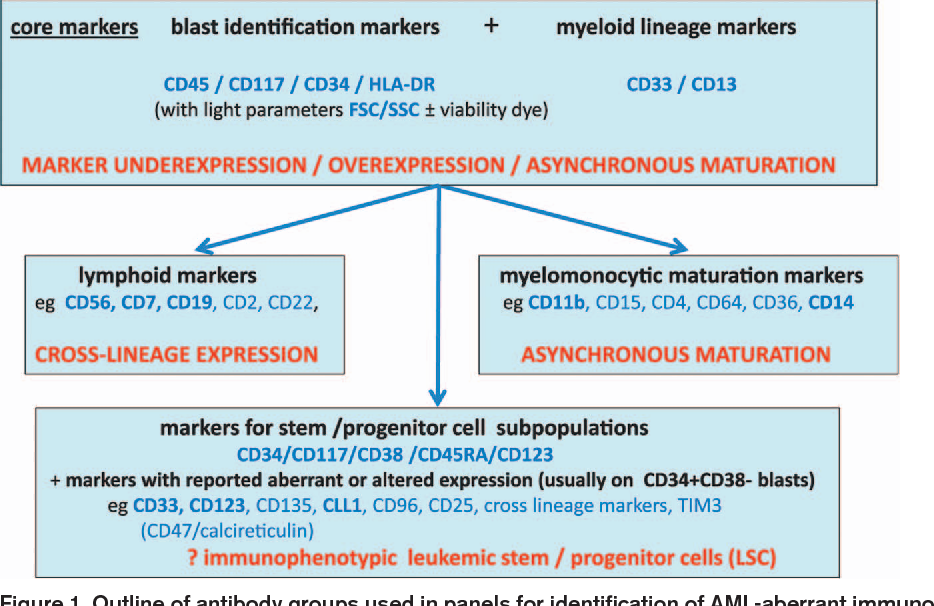
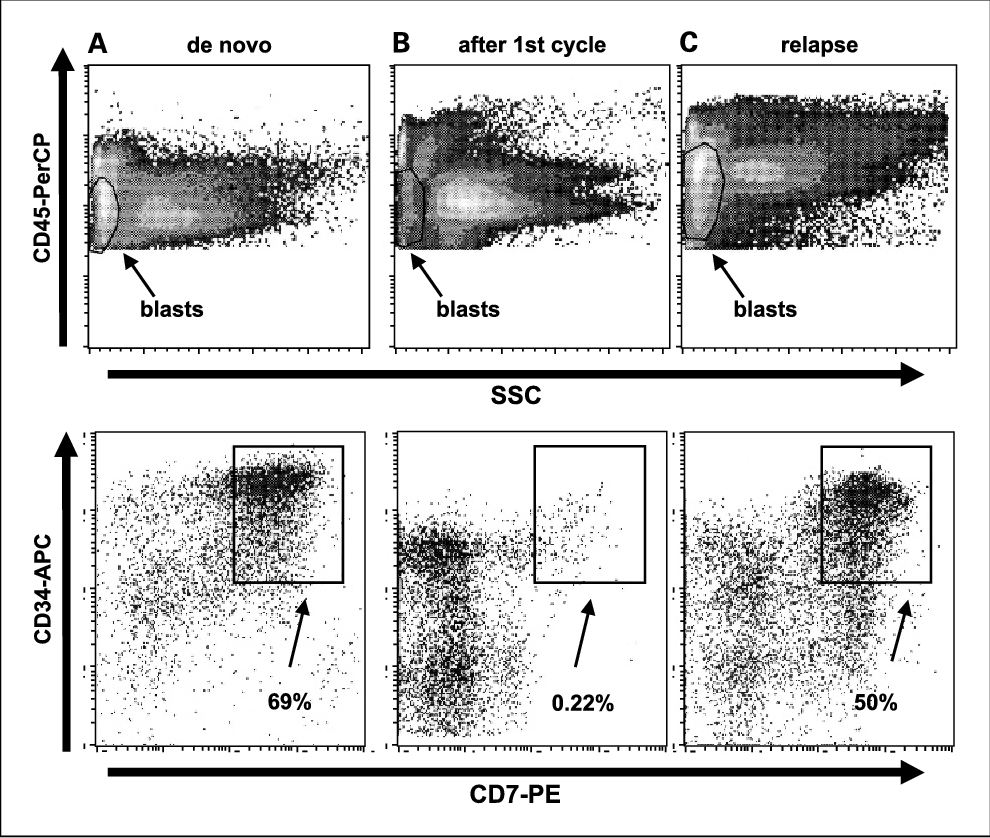
Several technologies are employed for MRD detection in AML. Flow cytometry is one common method, which uses antibodies to identify specific proteins on the surface of leukemia cells. These proteins serve as markers, distinguishing leukemia cells from normal blood cells. Polymerase chain reaction (PCR) is another highly sensitive technique that detects specific genetic mutations associated with leukemia.
The Significance of MRD Status
MRD status is increasingly recognized as a powerful prognostic factor in AML. Studies have consistently shown that patients who are MRD-negative after treatment have a significantly lower risk of relapse and better overall survival compared to those who are MRD-positive. This information enables clinicians to tailor treatment strategies based on individual risk profiles.
For example, a patient who achieves complete remission but remains MRD-positive might benefit from additional therapies, such as consolidation chemotherapy or allogeneic stem cell transplantation, to eradicate the remaining leukemia cells. Conversely, patients who are MRD-negative might be spared from unnecessary and potentially toxic treatments. This personalized approach is transforming AML management.
Challenges and Controversies
Despite its promise, MRD testing in AML is not without its challenges. One major issue is standardization. Different laboratories may use different assays and thresholds for defining MRD positivity, making it difficult to compare results across studies and institutions.
Another challenge is the dynamic nature of MRD. MRD levels can fluctuate over time, and a single MRD assessment may not accurately reflect the long-term risk of relapse. Serial MRD monitoring, where MRD is measured at multiple time points, may provide a more comprehensive picture of disease burden and treatment response.
Furthermore, the optimal timing and type of intervention based on MRD status are still being investigated. While several studies have demonstrated the prognostic value of MRD, there is less consensus on how to best use MRD information to guide treatment decisions. Some clinicians advocate for preemptive interventions in MRD-positive patients, while others prefer to wait for signs of clinical relapse before initiating further therapy.
Expert Opinions and Research Findings
Dr. Emily Smith, a hematologist-oncologist at the Mayo Clinic, emphasizes the importance of standardized MRD testing. "We need to ensure that MRD assays are accurate, reproducible, and comparable across different labs," she stated. "This will allow us to confidently use MRD information to make informed treatment decisions."
Recent research presented at the American Society of Hematology (ASH) annual meeting highlighted the utility of next-generation sequencing (NGS) for MRD detection in AML. NGS-based MRD assays can identify a wider range of genetic mutations and may be more sensitive than traditional methods. These finding is published on The New England Journal of Medicine.
A study published in the journal Blood showed that patients who underwent allogeneic stem cell transplantation and achieved MRD-negative status had significantly better long-term outcomes than those who remained MRD-positive. This finding supports the use of stem cell transplantation as a strategy to eradicate MRD in high-risk AML patients. These results comes from the National Cancer Institute.
The Future of MRD Monitoring in AML
The field of MRD monitoring in AML is rapidly evolving. Researchers are developing new and improved MRD assays with increased sensitivity and specificity. They are also exploring novel therapeutic strategies to target MRD in patients who remain MRD-positive after initial treatment.
One promising area of research is the development of MRD-directed therapies, such as targeted drugs or immunotherapies that specifically eliminate leukemia cells. These therapies could potentially eradicate MRD without causing the severe side effects associated with conventional chemotherapy. Ongoing research focuses on understanding how immune cells, like T cells, can be engineered to recognize and destroy MRD-positive leukemia cells.
Ultimately, the goal is to integrate MRD monitoring into routine clinical practice for all AML patients. By identifying those at high risk of relapse and tailoring treatment accordingly, we can improve outcomes and potentially cure more patients with this devastating disease. The European LeukemiaNet publishes recommendation on the role of MRD in the management of AML.

-positive+acute+myeloid+leukemia+may+indicate+risk+for+clinical+relapse+and+may+identify+patients+in+a+curable+state.jpg)