Most Digestive Enzymes Are Produced By The
.jpg)
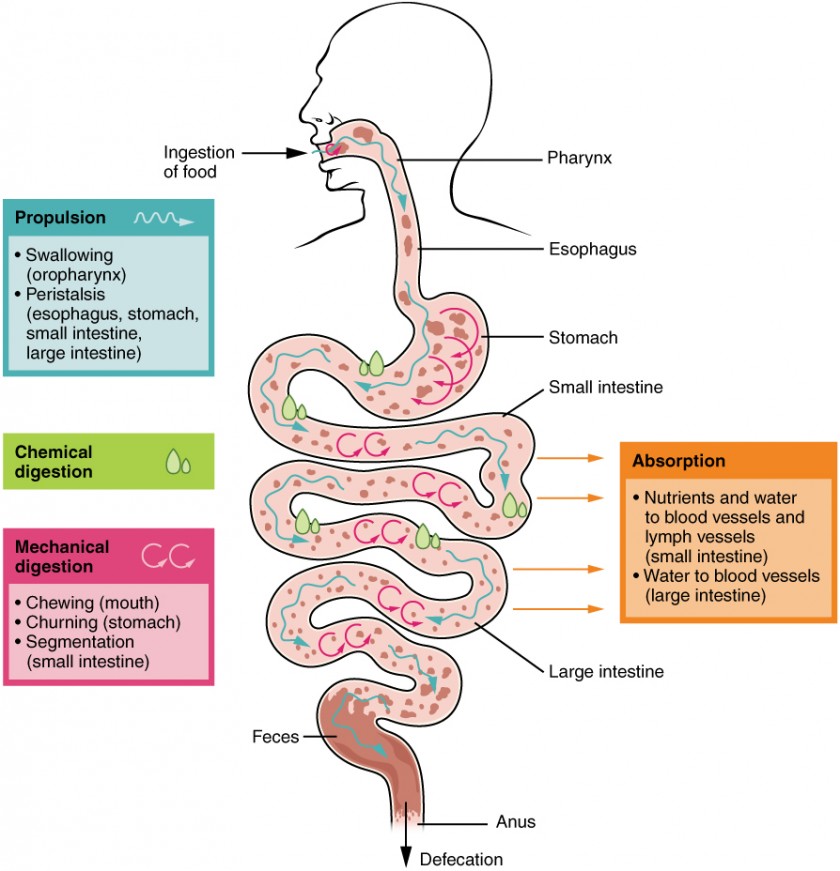
The human body, a marvel of biological engineering, relies on a complex interplay of systems to sustain life. At the heart of this intricate machinery lies the digestive system, responsible for breaking down food into absorbable nutrients. While we often focus on the stomach's role, a lesser-known organ, the pancreas, shoulders a significant burden in this vital process.
This article delves into the crucial role of the pancreas in digestive enzyme production, examining its dominance in supplying the enzymes necessary for nutrient breakdown. We will explore the specific enzymes produced by the pancreas, the implications of pancreatic dysfunction on digestion, and emerging research aimed at addressing digestive enzyme deficiencies. Understanding the pancreas's contribution is essential for comprehending overall digestive health and managing related conditions.
The Pancreas: A Digestive Powerhouse
The pancreas is a gland located behind the stomach in the upper abdomen. It serves a dual function, acting as both an endocrine and exocrine organ. Its endocrine function involves producing hormones like insulin and glucagon, crucial for regulating blood sugar levels.
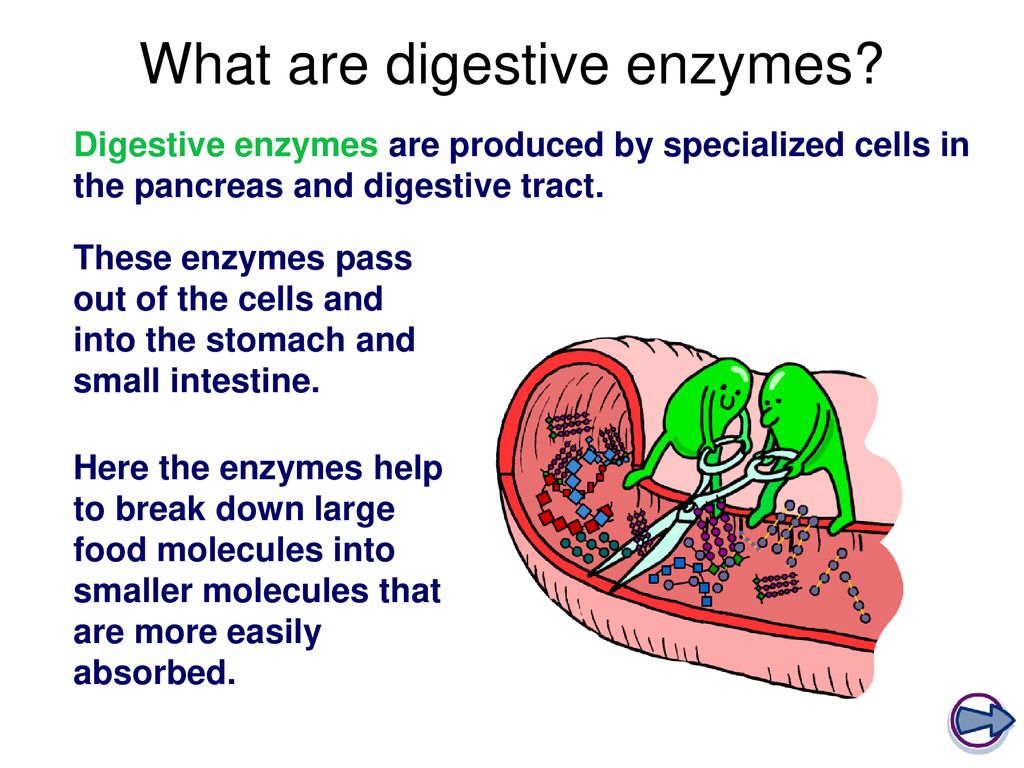
However, for the purpose of digestion, the pancreas's exocrine function takes center stage. Exocrine cells, specifically acinar cells, are responsible for synthesizing and secreting the vast majority of digestive enzymes.
Key Digestive Enzymes Produced by the Pancreas
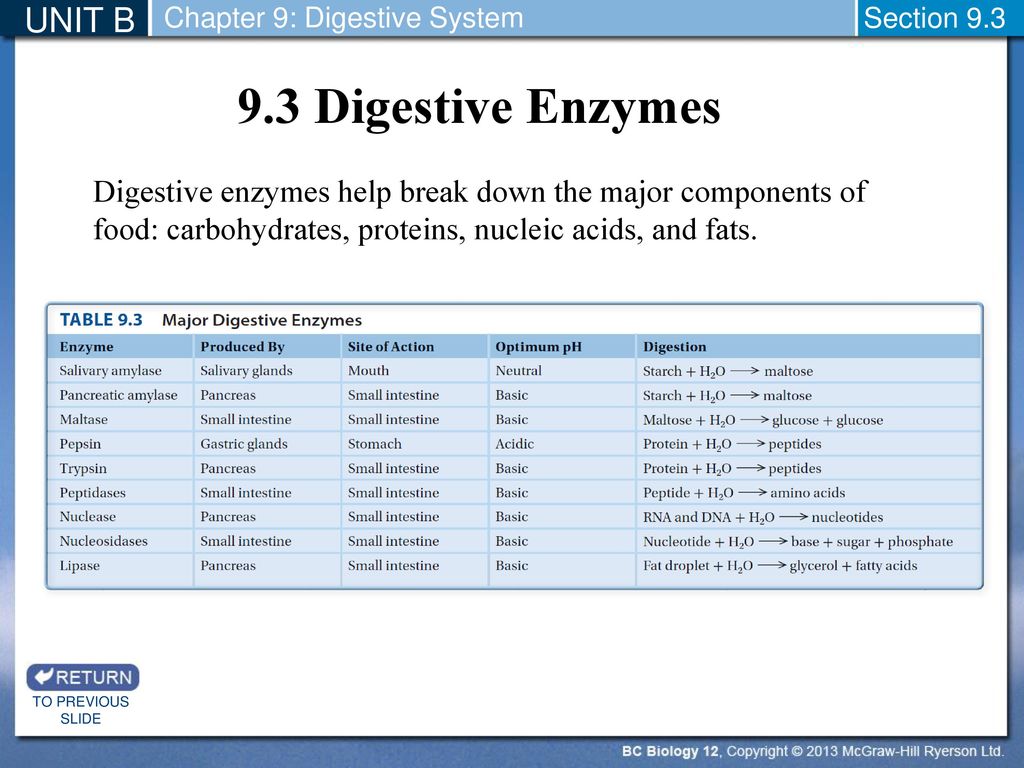
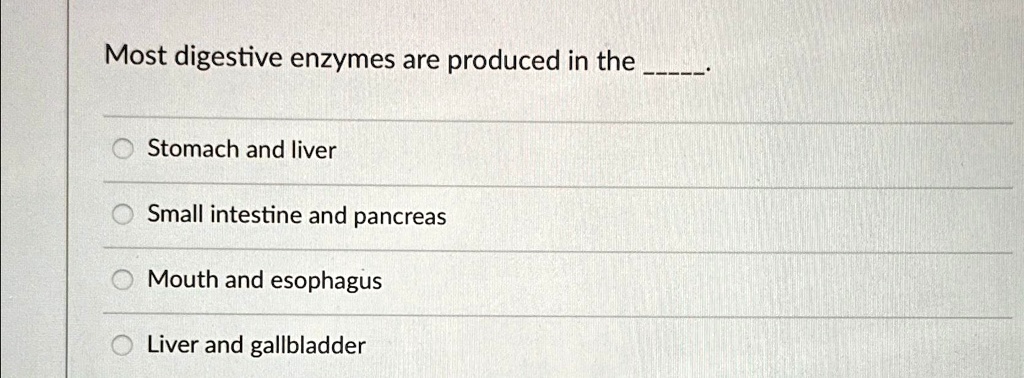
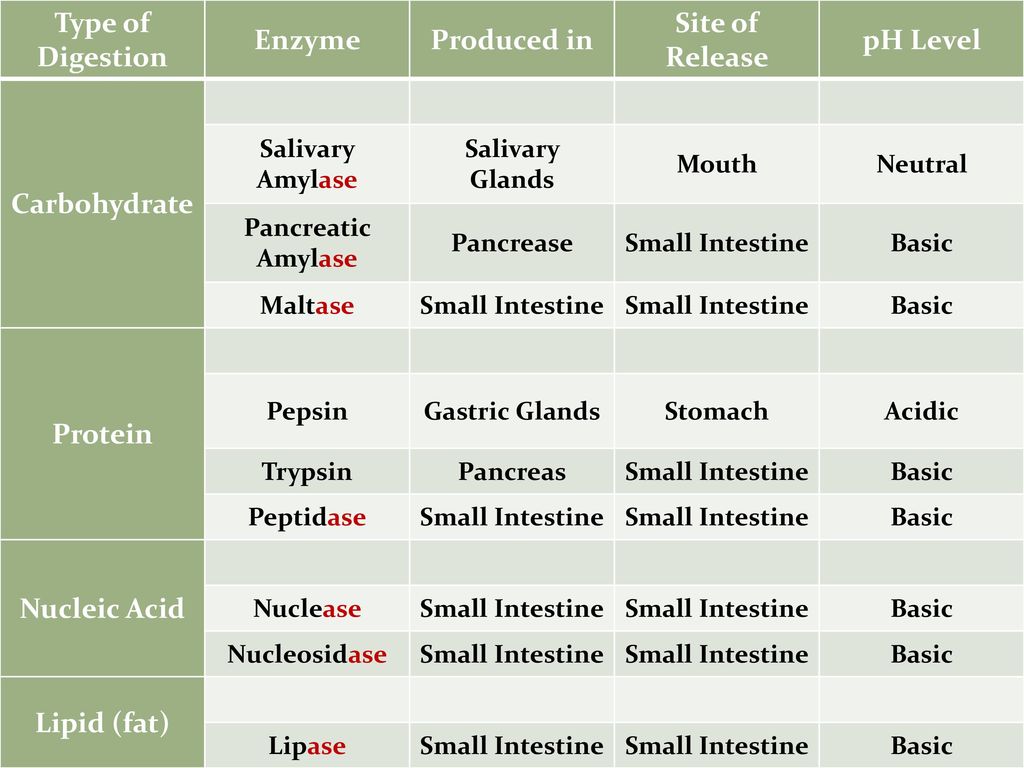
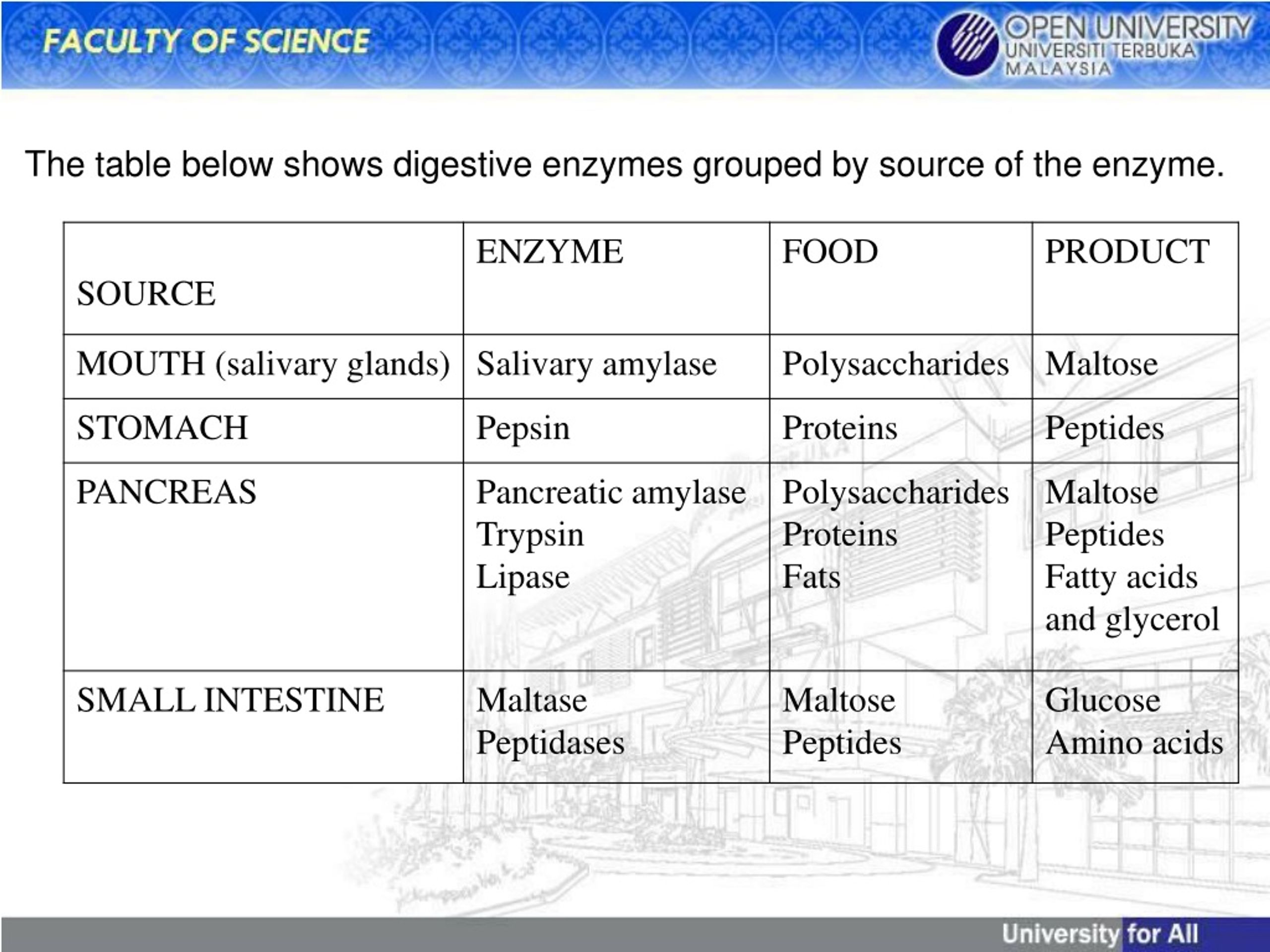
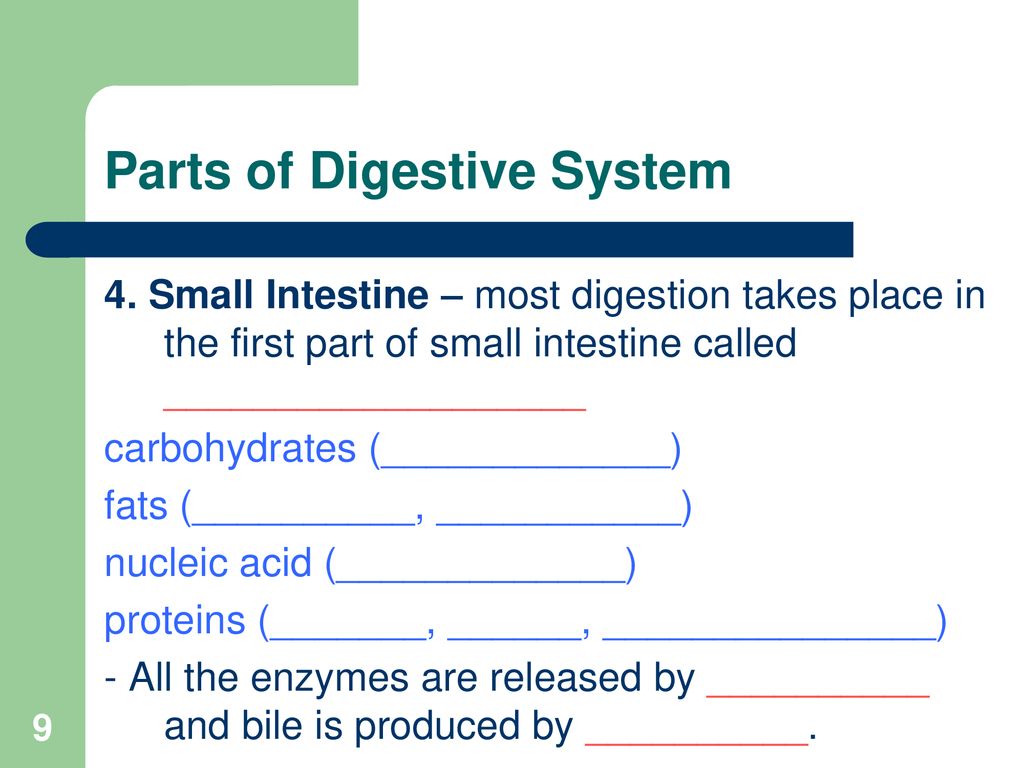
The pancreas produces a wide array of enzymes tailored to break down different macronutrients. These enzymes are secreted into the small intestine, where they play a crucial role in nutrient absorption. The following are some of the most important:
Pancreatic Amylase: This enzyme breaks down complex carbohydrates, such as starches, into simpler sugars like glucose. It complements the work of salivary amylase, which initiates carbohydrate digestion in the mouth.
Pancreatic Lipase: Lipase is essential for the digestion of fats (triglycerides). It breaks down fats into fatty acids and glycerol, which can then be absorbed by the small intestine.
Proteases (Trypsin, Chymotrypsin, Carboxypeptidase): These enzymes are responsible for breaking down proteins into smaller peptides and amino acids. They are secreted in an inactive form (zymogens) to prevent self-digestion of the pancreas, and are activated in the small intestine.
Other Enzymes: The pancreas also produces enzymes like ribonuclease and deoxyribonuclease, which break down RNA and DNA respectively. These enzymes are crucial for processing nucleic acids from ingested food.
The Limited Role of Other Organs
While the pancreas is the primary source of digestive enzymes, other organs contribute to the digestive process. The stomach, for instance, produces pepsin, an enzyme that breaks down proteins into smaller peptides.
The small intestine itself also produces some enzymes, such as lactase, maltase, and sucrase, which break down specific sugars. However, the quantities of these enzymes are significantly less than those produced by the pancreas.
The liver, via bile production, aids in fat digestion by emulsifying fats. This process increases the surface area for lipase to act upon, but the liver does not directly produce digestive enzymes.
Consequences of Pancreatic Enzyme Deficiency
When the pancreas fails to produce sufficient quantities of digestive enzymes, a condition known as pancreatic exocrine insufficiency (PEI) arises. This can lead to a variety of digestive problems.
Symptoms of PEI: Common symptoms include steatorrhea (fatty stools), abdominal pain, bloating, and weight loss. These symptoms arise due to the malabsorption of nutrients, particularly fats.
Causes of PEI: PEI can be caused by various conditions, including chronic pancreatitis, cystic fibrosis, pancreatic cancer, and surgical removal of part of the pancreas.
Diagnosis and Treatment: PEI is typically diagnosed through stool tests that measure the level of pancreatic enzymes, such as fecal elastase-1. Treatment usually involves pancreatic enzyme replacement therapy (PERT), where patients take oral enzyme supplements with meals to aid digestion.
Emerging Research and Future Directions
Ongoing research aims to improve the diagnosis and treatment of pancreatic enzyme deficiencies. One area of focus is developing more effective and convenient enzyme replacement therapies.
Scientists are also exploring ways to prevent or delay the progression of conditions that lead to PEI, such as chronic pancreatitis. This includes investigating potential therapeutic targets and lifestyle interventions.
Furthermore, researchers are examining the role of the gut microbiome in digestive health and its potential impact on pancreatic enzyme function. Understanding the complex interplay between the pancreas, gut microbiota, and other digestive organs could lead to novel therapeutic strategies.
The pancreas, often overshadowed by other digestive organs, stands as a critical player in ensuring efficient nutrient breakdown. Its unparalleled production of digestive enzymes underscores its central role in maintaining digestive health. Recognizing the importance of the pancreas and addressing enzyme deficiencies are vital for preventing and managing a range of digestive disorders. The future of digestive health hinges, in part, on continued research and advancements in understanding and treating pancreatic dysfunction.
..jpg)






.jpg)

.jpg)