Problems In Balance May Follow Trauma To Which Nerve
.png)
The world tilts, spins, and sways for those grappling with balance disorders following traumatic injuries. What was once a subconscious act – maintaining upright posture – becomes a daily struggle, a constant negotiation with gravity. Researchers are increasingly focused on the link between traumatic events and damage to a specific nerve, the vestibular nerve, as a primary cause of these debilitating balance issues.
Understanding the intricate connection between trauma, the vestibular nerve, and subsequent balance problems is crucial. This knowledge paves the way for improved diagnostics, targeted therapies, and ultimately, a better quality of life for those affected. This article delves into the complexities of this relationship, exploring the challenges in diagnosis, current treatment approaches, and future research directions aimed at restoring equilibrium.
The Vestibular Nerve: Gateway to Balance
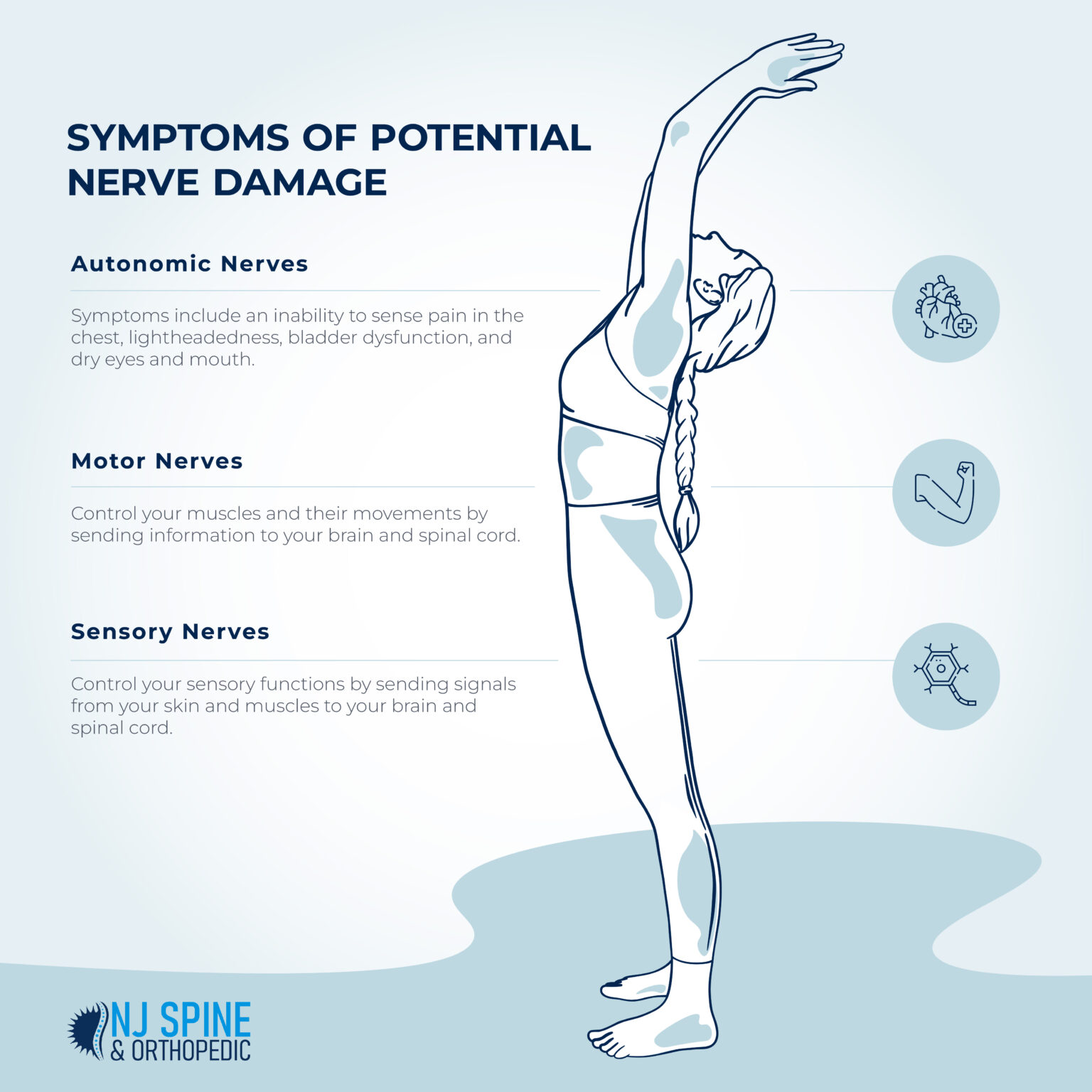
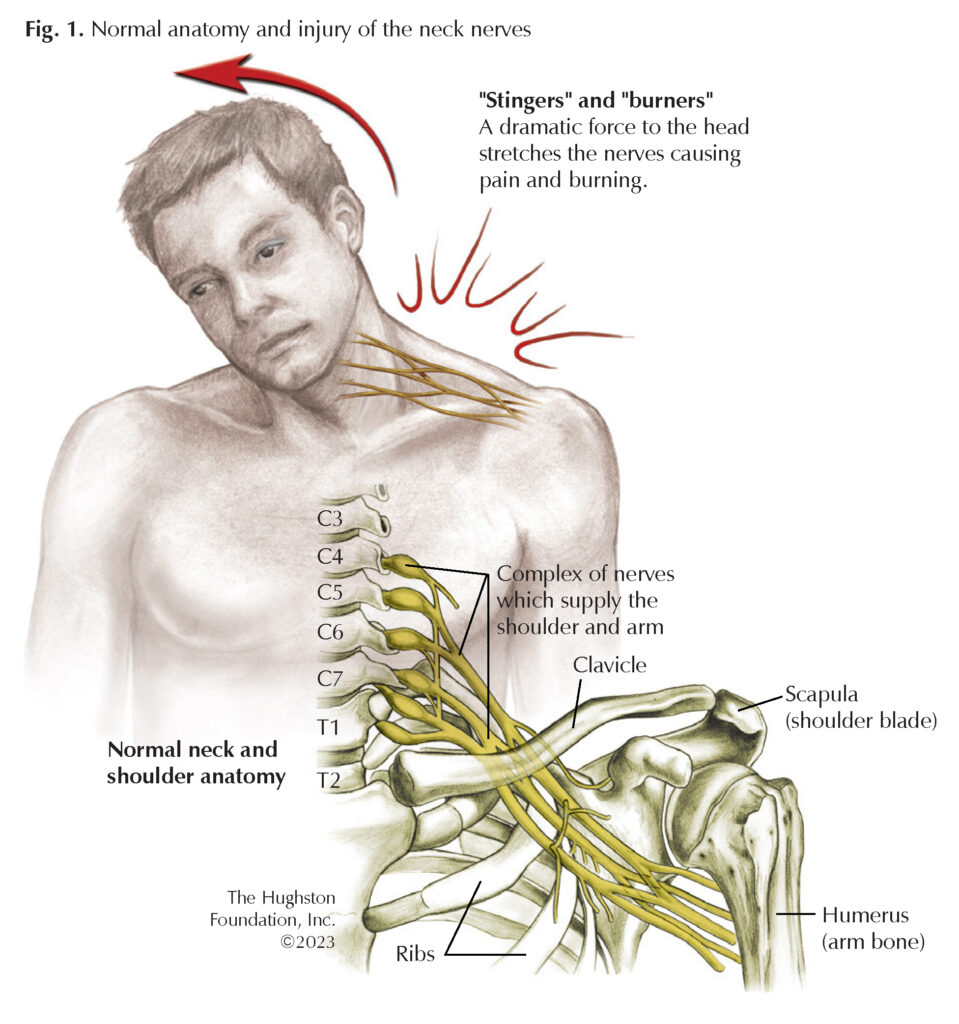
The vestibular system, located in the inner ear, is responsible for sensing head movements and spatial orientation. The vestibular nerve is a critical component of this system. It transmits information from the inner ear's sensory organs to the brainstem, where the data is processed and integrated with other sensory inputs to maintain balance and coordination.
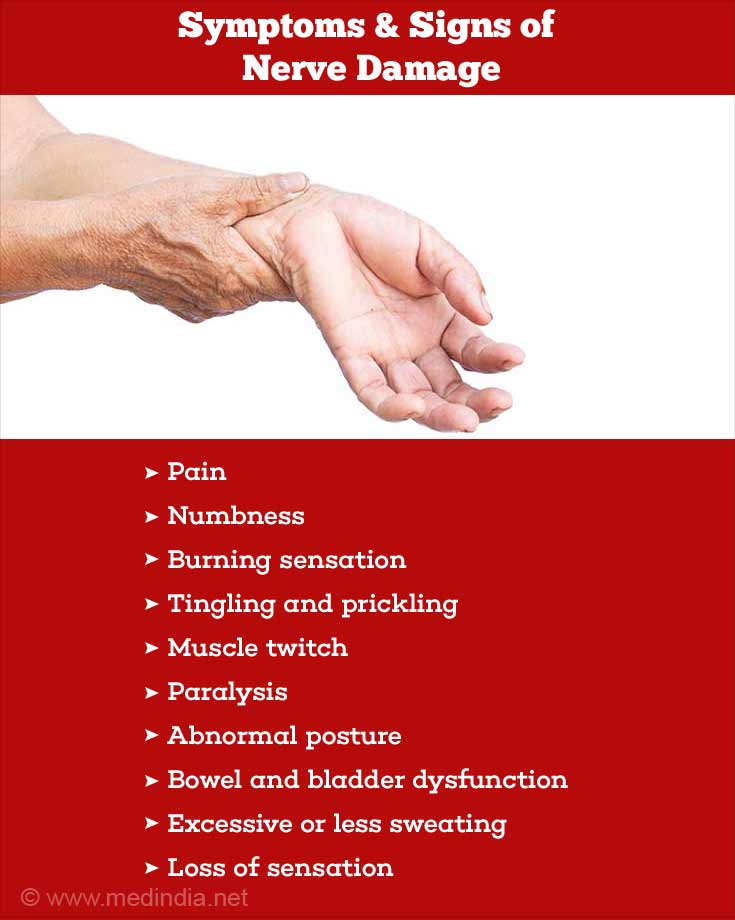
Trauma, especially head injuries like concussions or more severe traumatic brain injuries (TBIs), can directly damage the vestibular nerve. Indirect damage can also occur. This disrupts the flow of information and leads to a variety of balance disorders.
Causes of Vestibular Nerve Damage Post-Trauma
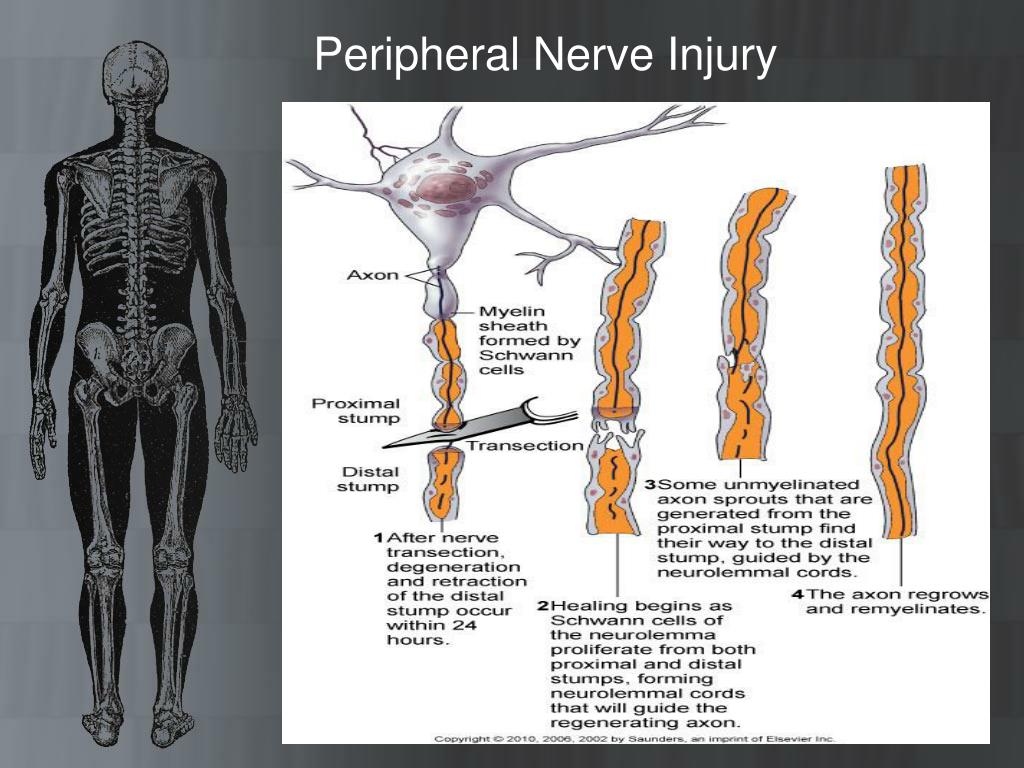
Several mechanisms contribute to vestibular nerve damage following trauma. Physical impact can cause fractures of the temporal bone, which houses the inner ear, directly injuring the nerve.
Shearing forces generated during rapid head movements can also stretch or tear the nerve fibers. Inflammation and edema (swelling) following trauma can compress the nerve, further disrupting its function.
Furthermore, vascular injuries affecting blood supply to the inner ear can lead to ischemia (lack of blood flow) and subsequent nerve damage. The location and severity of the trauma greatly influence the extent of vestibular nerve involvement.
Diagnosing Post-Traumatic Vestibular Dysfunction
Diagnosing vestibular dysfunction after trauma can be challenging. The symptoms, like dizziness, vertigo, and imbalance, can overlap with other post-concussive symptoms such as headaches and cognitive difficulties.
A comprehensive evaluation typically includes a detailed medical history, neurological examination, and specific vestibular tests. These tests assess the function of the inner ear and the vestibular nerve.
Videonystagmography (VNG) measures eye movements in response to various stimuli, providing insights into the function of the vestibular system. Rotary chair testing and vestibular evoked myogenic potentials (VEMPs) offer further objective data. The interpretation of these tests requires expertise and careful correlation with the patient's symptoms.
Treatment Strategies and Rehabilitation
Treatment for post-traumatic vestibular dysfunction often involves a multi-faceted approach. Vestibular rehabilitation therapy (VRT) is a cornerstone of treatment.
VRT is a specialized exercise program designed to retrain the brain to compensate for the damaged vestibular system. Exercises may include gaze stabilization, balance training, and habituation exercises to reduce sensitivity to movement.
Medications can also be used to manage symptoms such as nausea and vertigo. In rare cases, surgery may be considered if other treatments are ineffective and a specific structural problem is identified. The specific treatment plan is tailored to the individual's needs and the nature of their vestibular dysfunction.
The Patient Perspective: Living with Imbalance
Living with a post-traumatic balance disorder can significantly impact a person's quality of life. Simple tasks like walking, climbing stairs, or even turning the head can become challenging and anxiety-provoking.
The constant feeling of dizziness and instability can lead to fatigue, depression, and social isolation. Many individuals struggle to return to work or participate in activities they once enjoyed.
Support groups and counseling can be invaluable resources for patients and their families. These avenues offer emotional support, education, and strategies for coping with the challenges of living with a balance disorder. Patient advocacy groups like the Vestibular Disorders Association (VeDA) also play a crucial role.
Future Directions in Research
Research continues to explore new and improved methods for diagnosing and treating post-traumatic vestibular dysfunction. Scientists are investigating the potential of advanced imaging techniques, such as high-resolution MRI, to better visualize the vestibular nerve and identify subtle damage.
Studies are also exploring the use of regenerative therapies to promote nerve repair and regeneration. Pharmacological interventions are being developed to target specific mechanisms of vestibular dysfunction.
Ultimately, the goal is to develop more effective and personalized treatments to restore balance and improve the lives of individuals affected by post-traumatic vestibular disorders. Further investigation into biomarkers that can predict recovery outcomes is crucial for effective intervention planning.
Conclusion: Restoring Equilibrium, Reclaiming Lives
The link between trauma and vestibular nerve damage is increasingly recognized as a significant contributor to balance disorders. By understanding the mechanisms involved, improving diagnostic techniques, and developing targeted therapies, healthcare professionals can help individuals regain their equilibrium and reclaim their lives.
Continued research and collaboration are essential to further advance our knowledge and improve outcomes for those affected by these debilitating conditions. The pursuit of balance is not just a medical endeavor, but a commitment to restoring hope and independence.
The complexities of the vestibular system and its response to trauma require a holistic and patient-centered approach to care, ensuring that individuals receive the support and treatment they need to navigate their journey towards recovery and a more stable future.



:max_bytes(150000):strip_icc()/radial-nerve-injury-2488802-FINAL-fd11d7465f8f465db5848ea726e89b65.png)