What Is A Pcc In Healthcare
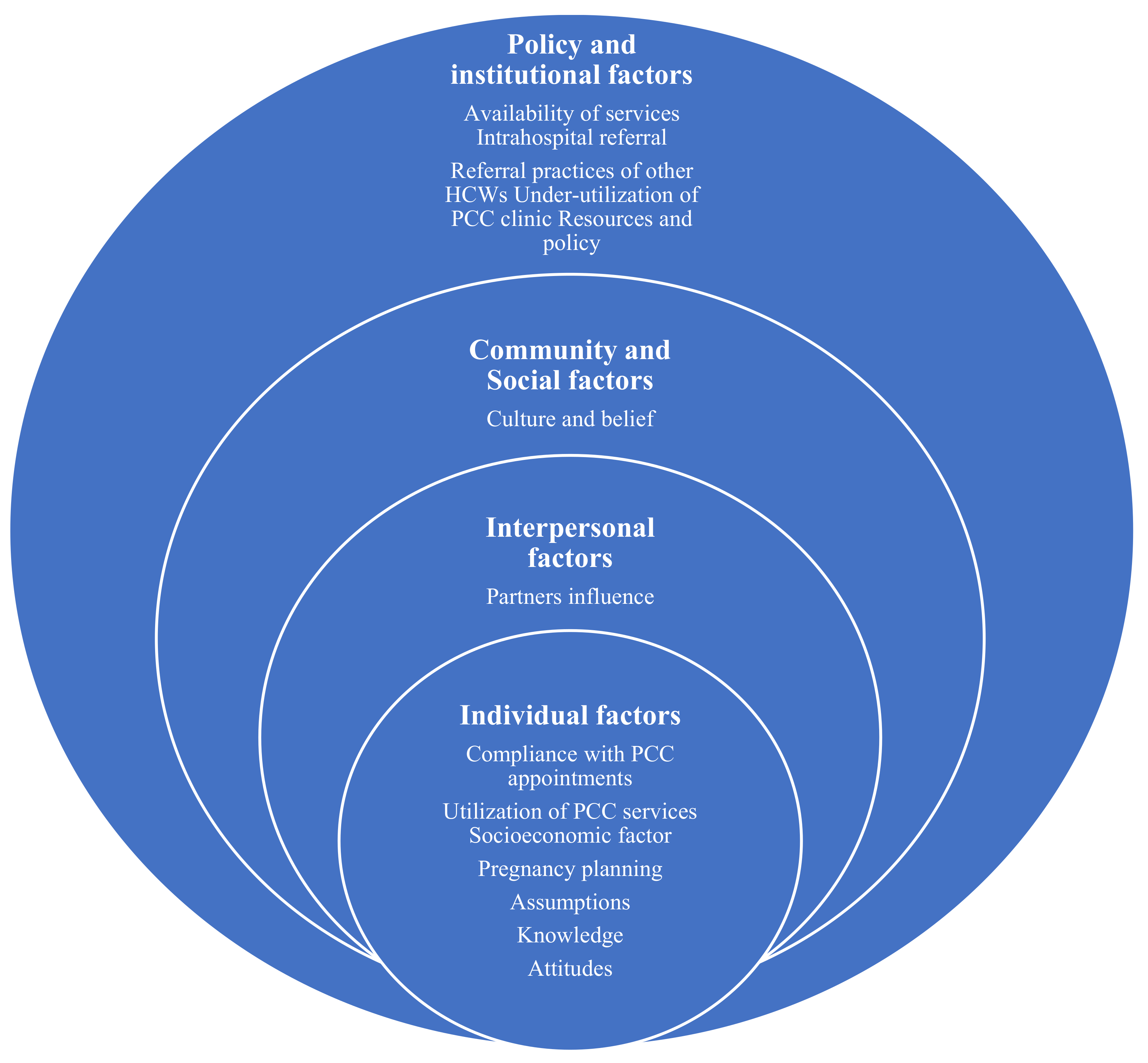
Healthcare providers are scrambling to implement Patient-Centered Care (PCC) models amidst rising demands for personalized and efficient medical services. This shift, driven by evolving patient expectations and a greater emphasis on value-based care, requires a fundamental change in how healthcare is delivered.
PCC places the individual patient's needs, preferences, and values at the heart of all healthcare decisions. It involves actively engaging patients in their own care, ensuring they are informed, respected, and empowered to make choices that align with their personal goals.
What Exactly is Patient-Centered Care?
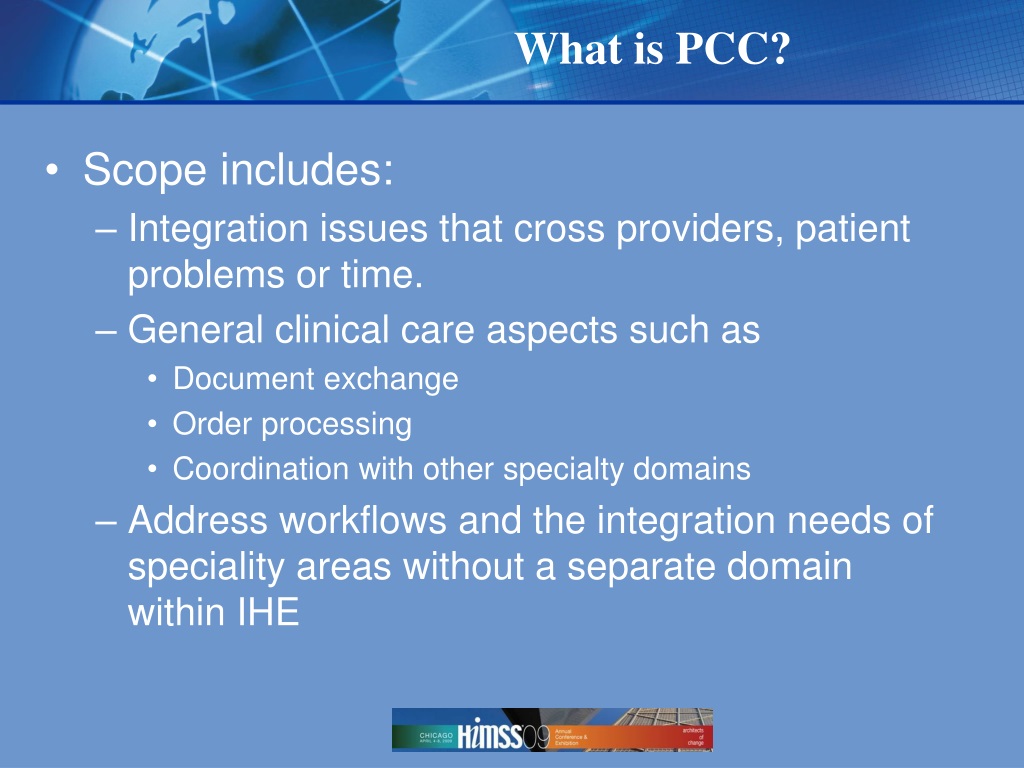
Patient-Centered Care (PCC) is a healthcare delivery model that prioritizes the patient's active role in their treatment. It moves away from a traditional, doctor-centric approach to one where the patient is a key partner in managing their health.
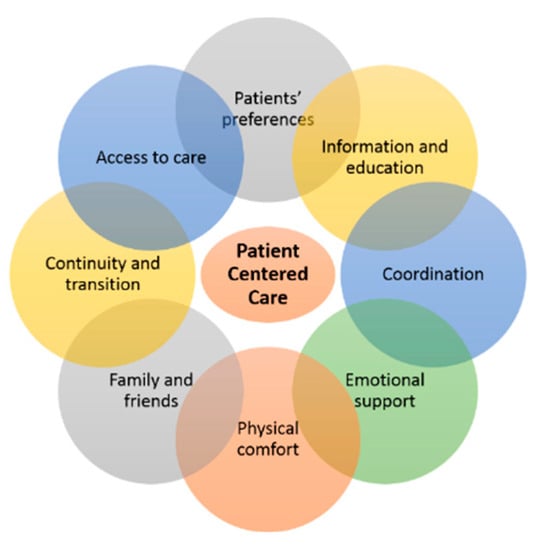
Core elements of PCC include shared decision-making, clear communication, and a focus on the patient's overall well-being. This includes not only their physical health but also their emotional, mental, and social needs.
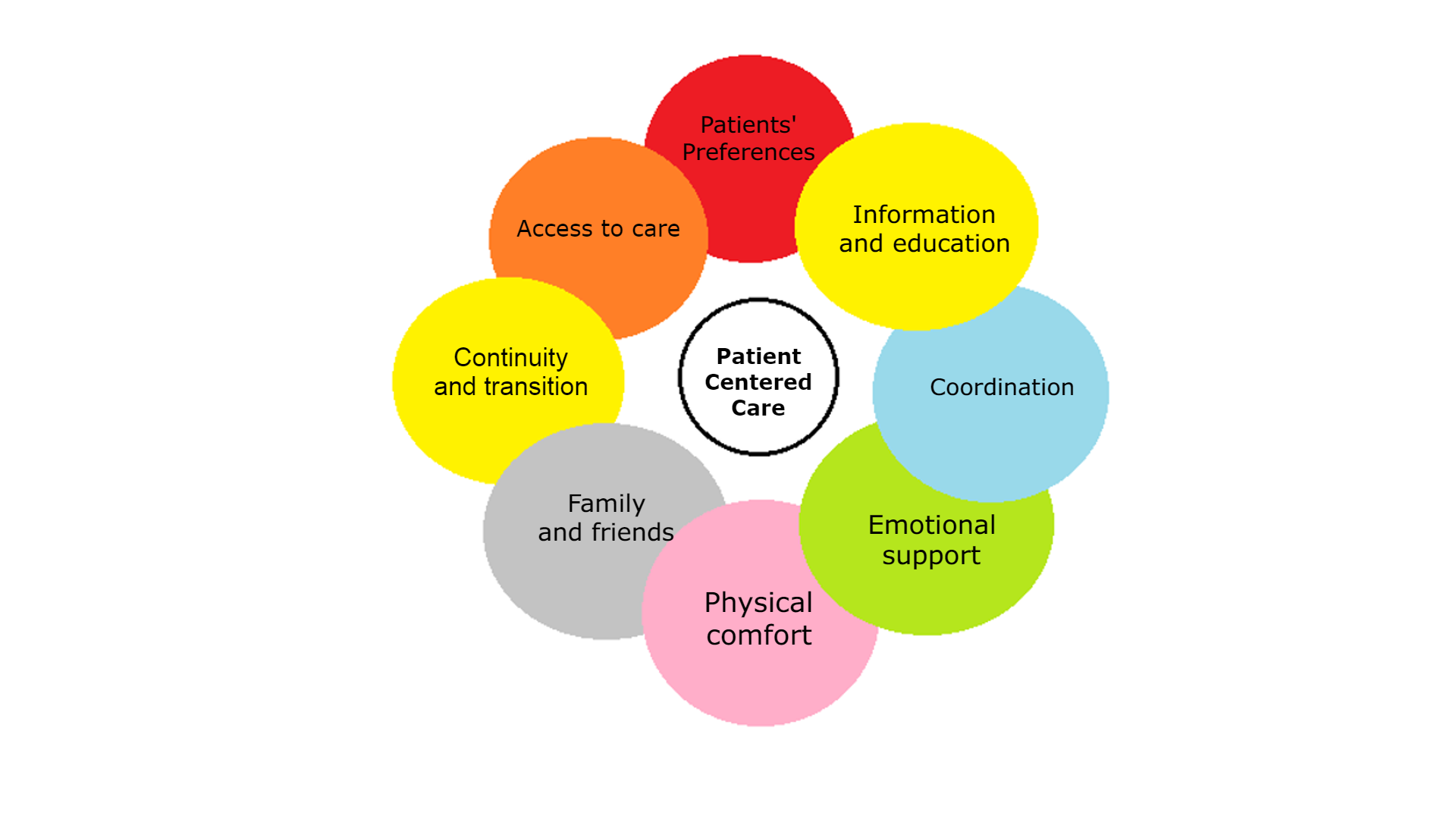
Key Principles of PCC
Several key principles underpin the PCC model. These principles guide healthcare providers in delivering care that is truly patient-focused.
- Respect for Patient Values: Recognizing and honoring the patient's individual beliefs, cultural background, and preferences.
- Coordination and Integration of Care: Ensuring seamless transitions between different healthcare providers and settings.
- Information, Communication, and Education: Providing patients with clear, accessible, and timely information about their health conditions and treatment options.
- Physical Comfort: Creating a healing environment that is comfortable, safe, and conducive to well-being.
- Emotional Support: Addressing the patient's emotional and psychological needs, providing empathy and understanding.
- Involvement of Family and Friends: Recognizing the importance of family and friends in the patient's support system.
- Access to Care: Ensuring that patients have timely and convenient access to the healthcare services they need.
Who is Involved in PCC?
PCC requires a collaborative effort from all members of the healthcare team. This includes physicians, nurses, therapists, pharmacists, and administrative staff.
Patients are, of course, the central figures, actively participating in decisions. Families and caregivers also play a vital role in supporting the patient's care.
Where is PCC Being Implemented?
PCC is being implemented across a wide range of healthcare settings. This includes hospitals, clinics, physician offices, and long-term care facilities.
The adoption of PCC is growing globally, with healthcare systems in countries like the United States, Canada, and the United Kingdom actively promoting its implementation.
When is PCC Important?
PCC is important at every stage of the healthcare journey. From initial diagnosis to treatment and ongoing management, the patient's perspective should be central.
It's particularly crucial when dealing with complex or chronic conditions. Effective PCC can improve patient outcomes, enhance satisfaction, and reduce healthcare costs.
How is PCC Implemented?
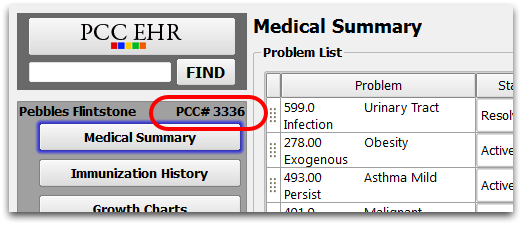
Implementing PCC requires a multi-faceted approach. This includes training healthcare providers, redesigning care processes, and using technology to enhance communication.
Electronic health records (EHRs) can play a vital role in facilitating information sharing and promoting patient engagement. Patient portals allow patients to access their medical records, communicate with their providers, and schedule appointments online.
Tools like decision aids can help patients understand their treatment options. Support shared decision-making with their healthcare providers.
Benefits of Patient-Centered Care
Numerous studies have demonstrated the benefits of PCC. Improved patient satisfaction is a consistent finding.
PCC can also lead to better health outcomes, reduced medical errors, and lower healthcare costs. By actively engaging patients in their care, providers can empower them to make informed decisions and take greater responsibility for their health.
Challenges to Implementation
Despite the benefits, implementing PCC can be challenging. Resistance to change from healthcare providers and a lack of resources are common obstacles.
Effective communication between patients and providers is essential, but barriers such as language differences or health literacy can hinder this process. Overcoming these challenges requires a commitment from healthcare leaders and a willingness to invest in training and infrastructure.
Next Steps and Ongoing Developments
Healthcare organizations are continuing to explore innovative ways to improve PCC. This includes using telehealth technologies to expand access to care and developing new models of care delivery that are more patient-focused.
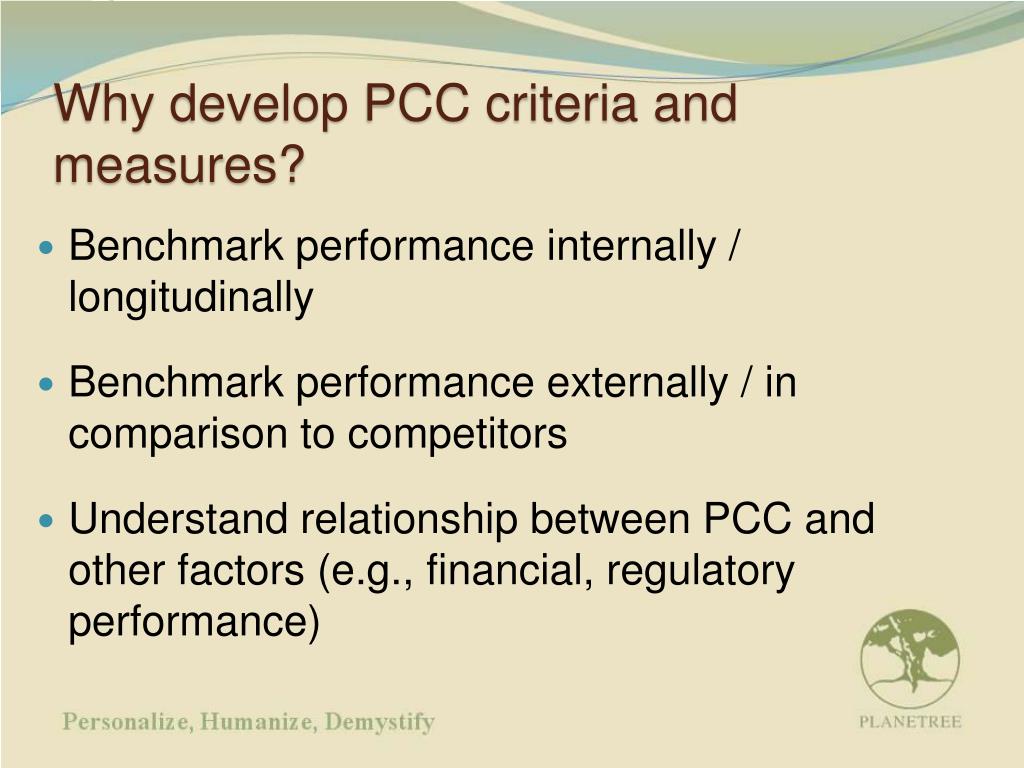
The ongoing development of quality metrics and performance indicators will help to track the effectiveness of PCC initiatives and identify areas for improvement. The emphasis remains on creating a healthcare system where the patient's voice is heard and respected at every step.






+improves+outcomes+of+pregnancies+complicated+by+diabetes.+Nationally%2C+the+uptake+of+PCC+remains+poor..jpg)